Abstract
Purpose
Diagnosing pneumonia by radiograph is improvable. We aimed (a) to compare radiograph and digital thoracic tomosynthesis (DTT) performances and agreement for COVID-19 pneumonia diagnosis, and (b) to assess the DTT ability for COVID-19 diagnosis when polymerase chain reaction (PCR) and radiograph are negative.
Methods
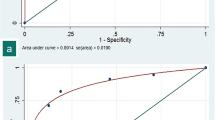
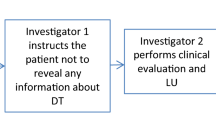
Two emergency radiologists with 11 (ER1) and 14 experience-years (ER2) retrospectively evaluated radiograph and DTT images acquired simultaneously in consecutively clinically suspected COVID-19 pneumonia patients in March 2020–January 2021. Considering PCR and/or serology as reference standard, DTT and radiograph diagnostic performance and interobserver agreement, and DTT contributions in unequivocal, equivocal, and absent radiograph opacities were analysed by the area under the curve (AUC), Cohen’s Kappa, Mc-Nemar’s and Wilcoxon tests.
Results
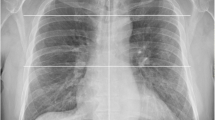
We recruited 480 patients (49 ± 15 years, 277 female). DTT increased ER1 (from 0.76, CI95% 0.7–0.8 to 0.79, CI95% 0.7–0.8; P=.04) and ER2 (from 0.77 CI95% 0.7–0.8 to 0.80 CI95% 0.8–0.8, P=.02) radiograph—AUCs, sensitivity, specificity, predictive values, and positive likelihood ratio. In false negative microbiological cases, DTT suggested COVID-19 pneumonia in 13% (4/30; P=.052, ER1) and 20% (6/30; P=.020, ER2) more than radiograph. DTT showed new or larger opacities in 33–47% of cases with unequivocal opacities in radiograph, new opacities in 2–6% of normal radiographs and reduced equivocal opacities by 13–16%. Kappa increased from 0.64 (CI95% 0.6–0.8) to 0.7 (CI95% 0.7–0.8) for COVID-19 pneumonia probability, and from 0.69 (CI95% 0.6–0.7) to 0.76 (CI95% 0.7–0.8) for pneumonic extension.
Conclusion
DTT improves radiograph performance and agreement for COVID-19 pneumonia diagnosis and reduces PCR false negatives.






Similar content being viewed by others
References
Coronavirus disease (COVID-19) – World Health Organization n.d.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed March 5, 2023)
Chen Y-J, Jian W-H, Liang Z-Y et al (2021) Earlier diagnosis improves COVID-19 prognosis: a nationwide retrospective cohort analysis. Annals of Translational Medicine 9:941–941. https://doi.org/10.21037/atm-20-7210
Plasencia-Martínez JM, Carrillo-Alcaraz A, Martín-Cascón M et al (2022) Early radiological worsening of SARS-CoV-2 pneumonia predicts the need for ventilatory support. Eur Radiol 32:3490–3500. https://doi.org/10.1007/s00330-021-08418-3
Maroldi R, Rondi P, Agazzi GM, Ravanelli M, Borghesi A, Farina D (2021) Which role for chest xray score in predicting the outcome in COVID-19 pneumonia? Eur Radiol 31:4016–4022. https://doi.org/10.1007/s00330-020-07504-2
Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH (2020) Essentials for radiologists on COVID-19: an update-radiology scientific expert panel. Radiology 296:E113–E114. https://doi.org/10.1148/radiol.2020200527
Böger B, Fachi MM, Vilhena RO, Cobre AF, Tonin FS, Pontarolo R (2021) Systematic review with meta-analysis of the accuracy of diagnostic tests for COVID-19. Am J Infect Control 49:21–29. https://doi.org/10.1016/j.ajic.2020.07.011
Alcoba-Florez J, Gil-Campesino H, de Artola DGM, Gonzalez-Montelongo R, Valenzuela-Fernandez A, Ciuffreda L, Flores C (2020) Sensitivity of different RT-qPCR solutions for SARS-CoV-2 detection. Int J Infect Dis 99:190–192. https://doi.org/10.1016/j.ijid.2020.07.058
Tahan S, Parikh BA, Droit L, Wallace MA, Burnham C-AD, Wang D (2021) SARS-CoV-2 e gene variant alters analytical sensitivity characteristics of viral detection using a commercial reverse transcription-PCR assay. J Clin Microbiol 59:e0007521. https://doi.org/10.1128/JCM.00075-21
Clinical management of COVID-19: Living guideline, 23 June 2022. Geneva: World health organization; 2022 (WHO/2019-nCoV/Clinical/2022.1). https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2022-1
Sadiq Z, Rana S, Mahfoud Z, Raoof A (2021) Systematic review and meta-analysis of chest radiograph (CXR) findings in COVID-19. Clin Imaging 80:229–238. https://doi.org/10.1016/j.clinimag.2021.06.039
Ebrahimzadeh S, Islam N, Dawit H et al (2022) Thoracic imaging tests for the diagnosis of COVID- 19. Cochrane Database Syst Rev 16(5):CD013639. https://doi.org/10.1002/14651858.CD013639.pub5
Tsakok M, Shaw R, Murchison A et al (2020) Diagnostic accuracy of initial chest radiograph compared to SARS-CoV-2 PCR in patients with suspected COVID-19. BJR Open 2:20200034. https://doi.org/10.1259/bjro.20200034
Stephanie S, Shum T, Cleveland H et al (2020) Determinants of chest X-ray sensitivity for COVID-19: a multi-institutional study in the United States. Radiol Cardiothorac Imaging 2:e200337. https://doi.org/10.1148/ryct.2020200337
Wong HYF, Lam HYS, Fong AH-T et al (2020) Frequency and distribution of chest radiographic findings in patients positive for COVID-19. Radiology 296:E72–E78. https://doi.org/10.1148/radiol.2020201160
Bao C, Liu X, Zhang H, Li Y, Liu J (2020) Coronavirus disease 2019 (COVID-19) CT findings: a systematic review and meta-analysis. J Am Coll Radiol 17:701–709. https://doi.org/10.1016/j.jacr.2020.03.006
Kovács A, Palásti P, Veréb D, Bozsik B, Palkó A, Kincses ZT (2021) The sensitivity and specificity of chest CT in the diagnosis of COVID-19. Eur Radiol 31:2819–2824. https://doi.org/10.1007/s00330-020-07347-x
Rubin GD, Ryerson CJ, Haramati LB et al (2020) The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Chest 158:106–116. https://doi.org/10.1016/j.chest.2020.04.003
Vikgren J, Zachrisson S, Svalkvist A et al (2008) Comparison of chest tomosynthesis and chest radiography for detection of pulmonary nodules: human observer study of clinical cases. Radiology 249:1034–1041. https://doi.org/10.1148/radiol.2492080304
Cho HJ, Feldman LS, Keller S, Hoffman A, Pahwa AK, Krouss M (2020) Choosing wisely in the COVID-19 era: preventing harm to healthcare workers. J Hosp Med 15:360–362. https://doi.org/10.12788/jhm.3457
Kwee TC, Kwee RM (2020) Chest CT in COVID-19: what the radiologist needs to know. Radiographics 40:1848–1865. https://doi.org/10.1148/rg.2020200159
Valdés P, Rovira A, Guerrero J, Morales Á, Rovira M, Martínez C (2020) Managing the pandemic from the radiology department’s point of view. Radiologia (Engl Ed) 62:503–514. https://doi.org/10.1016/j.rx.2020.10.004
García Santos JM, Plasencia Martínez JM, Fabuel Ortega P et al (2021) Radiology departments as COVID-19 entry-door might improve healthcare efficacy and efficiency, and emergency department safety. Insights Imaging 12:1. https://doi.org/10.1186/s13244-020-00954-8
Dobbins JT, McAdams HP (2009) Chest tomosynthesis: technical principles and clinical update. Eur J Radiol 72:244–251. https://doi.org/10.1016/j.ejrad.2009.05.054
COVID-19 BSTI Reporting templates | The British Society of Thoracic Imaging n.d. https://www.bsti.org.uk/covid-19-resources/covid-19-bsti-reporting-templates/ (accessed July 4, 2020)
Luo L, Luo Z, Jia Y et al (2020) CT differential diagnosis of COVID-19 and non-COVID-19 in symptomatic suspects: a practical scoring method. BMC Pulm Med 20:129. https://doi.org/10.1186/s12890-020-1170-1176
Calvo I, SantaCruz-Calvo S, Aranzana MG et al (2020) Digital tomosynthesis and COVID-19: an improvement in the assessment of pulmonary opacities. Arch Bronconeumol (Engl Ed) 56:761–763. https://doi.org/10.1016/j.arbres.2020.06.017
Baratella E, Ruaro B, Marrocchio C et al (2022) Diagnostic accuracy of chest digital tomosynthesis in patients recovering after COVID-19 pneumonia. Tomography 8:1221–1227. https://doi.org/10.3390/tomography8030100
Grosso M, Priotto R, Ghirardo D et al (2017) Comparison of digital tomosynthesis and computed tomography for lung nodule detection in SOS screening program. Radiol Med 122:568–574. https://doi.org/10.1007/s11547-017-0765-3
Ferrari A, Bertolaccini L, Solli P, Salvia POD, Scaradozzi D (2018) Digital chest tomosynthesis: the 2017 updated review of an emerging application. Ann Trans Med 6:91–91. https://doi.org/10.21037/atm.2017.08.18
Wan S, Li M, Ye Z et al (2020) CT manifestations and clinical characteristics of 1115 patients with coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Acad Radiol 27:910–921. https://doi.org/10.1016/j.acra.2020.04.033
Silva AC, Lawder HJ, Hara A, Kujak J, Pavlicek W (2010) Innovations in CT dose reduction strategy: application of the adaptive statistical iterative reconstruction algorithm. AJR Am J Roentgenol 194:191–199. https://doi.org/10.2214/AJR.09.2953
National Lung Screening Trial Research Team, Aberle DR, Adams AM et al (2011) Reduced lungcancer mortality with low-dose computed tomographic screening. N Engl J Med 365:395–409. https://doi.org/10.1056/NEJMoa1102873
Båth M, Svalkvist A, von Wrangel A, Rismyhr-Olsson H, Cederblad A (2010) Effective dose to patients from chest examinations with tomosynthesis. Radiat Prot Dosimetry 139:153–158. https://doi.org/10.1093/rpd/ncq092
Acknowledgements
We are very grateful for the essential statistical support provided by Mónica Ballesta Ruiz.
Author information
Authors and Affiliations
Contributions
Conceptualisation: JMPM, JMGS
Data curation: JMPM, AMP, MLR, CJP, IHE, GPH
Formal analysis: JMPM
Funding acquisition: n/a
Investigation: JMPM
Methodology: JMPM
Project administration: JMPM, JMGS
Resources: n/a
Software: n/a
Supervision: JMPM
Validation: JMPM
Visualisation: n/a
Writing—original draft: JMPM, AMP, MLR, CJP, IHE, GPH, JMGS
Writing—review and editing: JMPM, AMP, MLR, CJP, IHE, GPH, JMGS
All authors contributed to the study conception and design.
The first draft of the manuscript was written by Juana María Plasencia Martínez and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of our institution (internal code EST 55/20).
Conflict of interest
The authors Juana María Plasencia Martínez and José María García Santos received a speaking fee by General Electric Healthcare as webinars speakers on the application of digital thoracic tomosynthesis in COVID-19. They have been also engaged with the same company for clinical research to explore the utility in COVID-19 of artificial intelligence tools for chest radiography. The rest of authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Plasencia-Martínez, J.M., Moreno-Pastor, A., Lozano-Ros, M. et al. Digital tomosynthesis improves chest radiograph accuracy and reduces microbiological false negatives in COVID-19 diagnosis. Emerg Radiol 30, 465–474 (2023). https://doi.org/10.1007/s10140-023-02153-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-023-02153-6