Abstract
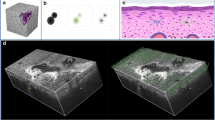
The present study proposed a noninvasive, automated, in vivo assessment method based on optical coherence tomography (OCT) and deep learning techniques to qualitatively and quantitatively analyze the biological effects of 2-µm laser-induced skin damage at different irradiation doses. Different doses of 2-µm laser irradiation established a mouse skin damage model, after which the skin-damaged tissues were imaged non-invasively in vivo using OCT. The acquired images were preprocessed to construct the dataset required for deep learning. The deep learning models used were U-Net, DeepLabV3+, PSP-Net, and HR-Net, and the trained models were used to segment the damage images and further quantify the damage volume of mouse skin under different irradiation doses. The comparison of the qualitative and quantitative results of the four network models showed that HR-Net had the best performance, the highest agreement between the segmentation results and real values, and the smallest error in the quantitative assessment of the damage volume. Based on HR-Net to segment the damage image and quantify the damage volume, the irradiation doses 5.41, 9.55, 13.05, 20.85, 32.71, 52.92, 76.71, and 97.24 J/cm² corresponded to a damage volume of 4.58, 12.56, 16.74, 20.88, 24.52, 30.75, 34.13, and 37.32 mm³. The damage volume increased in a radiation dose-dependent manner.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.





Similar content being viewed by others
Data availability
Data underlying the results presented in this paper are not publicly available at this time but may be obtained from the authors upon reasonable request.
References
Arash PM, Milad GM, Farnoosh S, Yeganeh K, Sogand S, Maryam A et al (2023) A systematic review and meta-analysis of efficacy, safety, and satisfaction rates of laser combination treatments vs laser monotherapy in skin rejuvenation resurfacing. Lasers Med Sci 38(1):228–530
Chen WR, Bartels KE, Liu H, Nordquist RE (2006) Laser-photothermal effect on skin tissue – damage and recovery. J X-Ray Sci Technol 14(3):207–215
Michael PD, Nicholas JG, Clifton DC, Semih SK, Benjamin AR, Robert JT (2021) Computational modeling and damage threshold prediction of continuous-wave and multiple-pulse porcine skin laser exposures at 1070nm. J Laser Appl 33(2):022023
Jabczynski JK, Zendzian W, Kwiatkowski J, Jelínková H, Šulc J (2010) Actively Q-switched, diode pumped thulium laser. Laser Phys Lett 4(12):863–867
Batay LE, Khodasevich IA, Khodasevich MA, Gorbunova NB, Manina EY (2016) Signs of the biological effect of ~ 2 µm low-intensity laser radiation in raman and absorption spectra of blood. J Appl Spectrosc 83(4):1–7
Tsvetkov VB (2021) Ex-vivo exposure on biological tissues in the 2-µm spectral range with an all-fiber continuous-wave holmium laser. Photonics 9(20):20
Zhao C, Wang K, Men C, Xin Y, Xia H (2022) The efficacy and safety of transurethral 2-µm laser bladder lesion mucosal en bloc resection in the treatment of cystitis glandularis. Front Med 9:840378
Artemov SA, Belyaev AN, Bushukina OS, Khrushchalina SA, Kostin SV, Lyapin AA et al (2022) Morphological changes of veins and perivenous tissues during endovenous laser coagulation using 2-µm laser radiation and various types of optical fibers. J Vasc Surg Venous Lymphat Disord 10(3):749–757
Filip T, Jan A, Pavel P, Ondřej S, Ali AJ et al (2020) Active optical fibers and components for Fiber lasers emitting in the 2-µm spectral range. Materials 13(22):E5177
Artemov SA, Belyaev AN, Bushukina OS, Khrushchalina SA, Kostin SV et al (2022) Morphological changes of veins and perivenous tissues during endovenous laser coagulation using 2-µm laser radiation and various types of optical fibers. JVS-VL 10(3):749–757
Uwe P, Miriam Z, Jens MB, Thorsten B, Hans JC, Michael D et al (2022) S2k guideline: laser therapy of the skin. J Dtsch Dermatol Ges 20(9):1248–1267
Stella XC, Judy C, Jacqueline W, Jeffrey SD, Hye JC (2022) Review of lasers and energy-based devices for skin rejuvenation and scar treatment with histologic correlations. Dermatol Surg 48(4):441–448
Ma Q, Fan Y, Luo Z, Cui Y, Kang H (2020) Quantitative analysis of collagen and capillaries of 3.8-µm laser-induced cutaneous thermal injury and wound healing. Lasers Med Sci 36(7):1469–1477
Sang X, Li D, Chen B (2020) Improving imaging depth by dynamic laser speckle imaging and topical optical clearing for in vivo blood flow monitoring. Lasers Med Sci 36(2):387–399
Wido H, Wiendelt S, Gooitzen MD, Christiaan B (2019) Clinical applications of laser speckle contrast imaging: a review. J Biomed Opt 24(8):080901
Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W et al (1991) Optical coherence tomography. Science 254(5035):1178–1181
Tadrous PJ (2021) Methods for imaging the structure and function of living tissues and cells: optical coherence tomography. J Pathol 191(2):115–119
Pan L, Chen X (2021) Retinal OCT image registration: methods and applications. IEEE Rev Biomed Eng 16(99):307–318
Fan Y, Ma Q, Wang J, Wang W, Kang H (2021) Evaluation of a 3.8-µm laser-induced skin injury and their repair with in vivo OCT imaging and noninvasive monitoring. Lasers Med Sci 37(2):1299–1309
Gong P, Shaghayegh E, Karl AH, Alexandra M, Suzanne R, Fiona MW (2016) In vivo label-free lymphangiography of cutaneous lymphatic vessels in human burn scars using optical coherence tomography. Biomed Opt Express 7(12):4886–4898
Rammah Y, Gaurav G, Nabhan Y, Manju K (2022) A holistic overview of deep learning approach in medical imaging. Multimed Syst 28(3):881–914
Wang R, Lei T, Cui R, Zhang B, Meng H, Nandi AK (2023) Medical image segmentation using deep learning: a survey. IET Image Process 53(18):20891–20916
Yang H, Wang Z, Liu X, Li C, Xin J, Wang Z (2022) Deep learning in medical image super resolution: a review. IET Image Process 16(5):1243–1267
Fischman S, Pérez AJ, Tognetti L, Di NA, Suppa M, Cinotti E (2022) Non-invasive scoring of cellular atypia in keratinocyte cancers in 3D LC-OCT images using deep learning. Sci Rep 12(1):481
Luo Y, Wang X, Yu X, Jin R, Liu L (2021) Imaging sebaceous gland using optical coherence tomography with deep learning assisted automatic identification. J Biophotonics 14(6):e202100015
Martin P, Hannes S, Kornelia S, Bhavapriya JS, Christine H, Leopold S (2021) Deep learning differentiates between healthy and diabetic mouse ears from optical coherence tomography angiography images. Ann N Y Acad Sci 1497(1):15–26
Timo K, Christine D, Malte C, Michael E, Gereon H, Nunciada S (2019) Segmentation of mouse skin layers in optical coherence tomography image data using deep convolutional neural networks. Biomed Opt Express 10(7):3484–3496
Breugnot J, Rouaud TP, Gilardeau S, Rondeau D, Bordes S, Aymard E et al (2022) Utilizing deep learning for dermal matrix quality assessment on in vivo line-field confocal optical coherence tomography images. Skin Res Technol 29(1):1–8
Chou H, Huang S, Tjiu J, Chen H (2021) Dermal epidermal junction detection for full-field optical coherence tomography data of human skin by deep learning. Comput Med Imaging Graph 87
Chen I, Wang Y, Chang C, Wu Y, Lu C, Shen J (2021) Computer-aided detection (cade) system with optical coherent tomography for melanin morphology quantification in melasma patients. Diagnostics 11(8):1498
Ji Y, Yang S, Zhou K, Rocliffe HR, Pellicoro A, Cash JL (2022) Deep-learning approach for automated thickness measurement of epithelial tissue and scab using optical coherence tomography. J Biomed Opt 27(1):015002
Gao T, Liu S, Gao E, Wang A, Tang X, Fan Y (2022) Automatic segmentation of laser-induced injury oct images based on a deep neural network model. Int J Mol Sci 23(19):11079
Zhu M, Chen W, Sun Y, Li Z (2023) Improved u-net-based leukocyte segmentation method. J Biomed Opt 28(4):045002
Bai Y, Li J, Shi L, Jiang Q, Yan B, Wang Z (2023) DME-DeepLabV3+: a lightweight model for diabetic macular edema extraction based on DeepLabV3 + architecture. Front Med 10:1150295
Wang S, Li Z, Liao L, Zhang C, Zhao J, Sang L et al (2023) DPAM-PSPNet: Ultrasonic image segmentation of thyroid nodule based on dual-path attention mechanism. Phys Med Biol 68(16):165002
Zhu L, Zhu H, Yang S, Wang P, Huang H (2023) Pulmonary nodule detection based on hierarchical-Split HRNet and feature pyramid network with atrous convolution. Biomed Signal Process Control 85:105024
Acknowledgements
Nothing.
Funding
Nothing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, C., Ma, Q., Wei, Y. et al. Deep learning automatically assesses 2-µm laser-induced skin damage OCT images. Lasers Med Sci 39, 106 (2024). https://doi.org/10.1007/s10103-024-04053-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-024-04053-8