Abstract
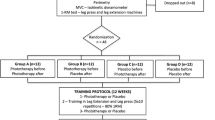
To investigate the effect of two photobiomodulation approaches on trunk flexor performance after incisional hernia repair and to compare the effects of both wavelengths. Forty-five patients were randomly distributed after isokinetic trunk flexor assessments into infrared laser, red laser, and placebo groups. Each patient received laser treatment followed by a traditional physical therapy program. In laser treatment, 24 points in both recti were irradiated by infrared or red laser light with the following parameters; 0.6 J per point, 214.28 J/cm2 as energy density, and 17.85 W/cm2 as intensity, while the control group received a placebo approach. All groups received clinical treatments at a rate of 3 sessions per week for 4 weeks; in addition, the physical therapy program was continued on other days for all groups. Isokinetic trunk flexor strength was measured before treatment and 4 weeks after treatment as in each measurement, fatigue protocol was designed, and the trunk flexor strength was measured before fatigue test while the trunk flexor resistance to fatigue was measured after fatigue test. After 4 weeks, pre-and post-fatigue trunk flexor strengths in both laser groups were significantly increased compared to pre-and post-fatigue trunk flexor strength in the placebo group, respectively, and there was no significant difference between the two laser groups. Photobiomodulation approaches enhance trunk flexor response to exercise after incisional hernia repair. This enhancement leads to greater strength and more fatigue resistance for the trunk flexors in photobiomodulation groups compared to the placebo group and no difference between the two photobiomodulation effects.



Similar content being viewed by others
Data availability and material
The datasets generated and/or analysed during the current study are available in the figshare repository, https://figshare.com/s/e944ebe8a37bb1426b4f.
References
Bucknall TE, Cox PJ, Ellis H (1982) Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. Br Med J 284:931–933. https://doi.org/10.1136/bmj.284.6320.931
Kurmann A, Beldi G, Vorburger SA et al (2010) Laparoscopic incisional hernia repair is feasible and safe after liver transplantation. Surg Endosc 24:1451–1455. https://doi.org/10.1007/s00464-009-0799-2
Yagnik VD, Joshipura V (2017) Non-incisional traumatic lateral abdominal wall hernia. ANZ J Surg 87(11):952–953. https://doi.org/10.1111/ans.14052
Hesselink VJ, Luijendijk RW, De Wilt JH, Heide R, Jeekel J (1993) An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet 176:228–234
Abrahamsom J, Eldar S (1989) Abdominal incision. Lancet 1:847
Zucker BE, Simillis C, Tekkis P, Kontovounisios C (2019) Suture choice to reduce occurrence of surgical site infection, hernia, wound dehiscence and sinus/fistula: a network meta-analysis. Ann R Coll Surg Engl 101(3):150–161. https://doi.org/10.1308/rcsann.2018.0170
Grevious MA, Cohen M, Shah SR, Rodriguez P (2006) Structural and functional anatomy of the abdominal wall. Clin Plast Surg 33:169–179. https://doi.org/10.1016/j.cps.2005.12.005
Flament JB, Avisse C, Palot JP, Pluot M, Burde A, Rives J (1997) Trophic ulcers in giant incisional hernias-pathogenesis and treatment. A report of 33 cases. Hernia 1:71–76. https://doi.org/10.1007/bf02427665
DuBay DA, Choi W, Urbanchek MG, Wang X, Adamson B, Dennis RG et al (2007) Incisional herniation induces decreased abdominal wall compliance via oblique muscle atrophy and fibrosis. Ann Surg 245:40–6. https://doi.org/10.1097/01.sla.0000251267.11012.85
Blondeel N, Vanderstraeten GG, Monstrey SJ (1997) The donor site morbidity of free DIEP flaps and free TRAM flaps in breast reconstruction. Br J Plast Surg 50:322–330. https://doi.org/10.1016/s0007-1226(97)90540-3
Lam KS, Mehdian H (1992) The importance of an intact abdominal musculature mechanism in maintaining spinal sagittal balance: case illustration in prune-belly syndrome. Spine 24:712–722. https://doi.org/10.1097/00007632-199904010-00022
Balogh B, Zauner-Dung A, Nicolakis P, Armbruster C, Kriwanek S, Piza-Katzer H (2002) Functional impairment of the abdominal wall following laparoscopic and open cholecystectomy. Surg Endosc 16:481–486. https://doi.org/10.1007/s004640090105
Huang YY, Chen AC, Carrol JD, Hamblin MR (2009) Biphasic dose response in low level light therapy. Dose Response 7:358–383. https://doi.org/10.2203/dose-response.09-027.hamblin
Enwemeka CS, Parker JC, Dowdy DS, Harkness EE, Sanford LE, Woodruff LD (2004) The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg 22:323–329. https://doi.org/10.1089/pho.2004.22.323
De Marchi T, Leal Junior EC, Bortoli C, Tomazoni SS, Lopes-Martins RA, Salvador M (2012) Low-level laser therapy (PBMT) in human progressive-intensity running: effects on exercise performance, skeletal muscle status, and oxidative stress. Lasers Med Sci 27:231–236. https://doi.org/10.1007/s10103-011-0955-5
de Almeida P, Lopes-Martins RÁ, Tomazoni SS, Silva JA Jr, de Carvalho PT, Bjordal JM et al (2011) Low-level laser therapy improves skeletal muscle performance, decreases skeletal muscle damage and modulates mRNA expression of COX-1 and COX-2 in a dose-dependent manner. Photochem Photobiol 87:1159–1163. https://doi.org/10.1111/j.1751-1097.2011.00968.x
Corin G, Strutton PH, McGregor AH (2005) Establishment of a protocol to test fatigue of the trunk muscles. Br J Sports Med 39:731–735. https://doi.org/10.1136/bjsm.2004.015537
Dos Reis FA, da Silva BAK, Laraia EMS, de Melo RM, Silva PH, Leal-Junior ECP et al (2014) Effects of pre- or post-exercise low-level laser therapy (830 nm) on skeletal muscle fatigue and biochemical markers of recovery in humans: double-blind placebo-controlled trial. Photomed Laser Surg 32:106–112. https://doi.org/10.1089/pho.2013.3617
Jówko E, Płaszewski M, Cieśliński M, Sacewicz T, Cieśliński I, Jarocka M (2019) The effect of low level laser irradiation on oxidative stress, muscle damage and function following neuromuscular electrical stimulation. A double blind, randomised, crossover trial. BMC Sports Sci Med Rehabil 11(1):38. https://doi.org/10.1186/s13102-019-0147-3
De Carli ML, Guerra MB, Nunes TB, di Matteo RC, de Luca CEP, Aranha ACC, Witzel AL (2012) Piroxicam and laser phototherapy in the treatment of TMJ arthralgia: a double-blind randomised controlled trial. J Oral Rehabil 40(3):171–178. https://doi.org/10.1111/joor.12022
Thompson MJ, Trainor B (2007) Prevention of parastomal hernia: a comparison of results 3 years on. Gastrointest Nurs 5:22–28
Revicki DA, Israel RG (1986) Relationship between body mass indices and measures of body adiposity. Am J Public Health 76(8):992–994. https://doi.org/10.2105/ajph.76.8.992
Ferraresi C, de Brito OT, de Oliveira ZL, de Menezes Reiff RB, Baldissera V, de Andrade Perez SE (2011) Effects of low level laser therapy (808 nm) on physical strength training in humans. Lasers Med Sci 26:349–358. https://doi.org/10.1007/s10103-010-0855-0
Assis L, Moretti AI, Abrahao TB, de Souza HP, Hamblin MR, Parizotto NA (2013) Low-level laser therapy (808 nm) contributes to muscle regeneration and prevents fibrosis in rat tibialis anterior muscle after cryolesion. Lasers Med Sci 28:947–955. https://doi.org/10.1007/s10103-012-1183-3
Ben-Dov N, Shefer G, Irinitchev A, Wernig A, Oron U, Halevy O (1999) Low-energy laser irradiation affects satellite cell proliferation and differentiation in vitro. Biochim Biophys Acta (BBA) – Mol Cell Res 1448(3):372–380. https://doi.org/10.1016/s0167-4889(98)00147-5
de Almeida P, Lopes-Martins RA, De Marchi T, Tomazoni SS, Albertini R, Corrêa JC et al (2012) Red (660 nm) and infrared (830 nm) low-level laser therapy in skeletal muscle fatigue in humans: what is better? Lasers Med Sci 27:453–458. https://doi.org/10.1007/s10103-011-0957-3
Ravera S, Ferrando S, Agas D, De Angelis N, Raffetto M, Sabbieti MG et al (2019) 1064 nm Nd:YAG laser light affects transmembrane mitochondria respiratory chain complexes. J Biophotonics 12(9):e201900101. https://doi.org/10.1002/jbio.201900101
Amaroli A, Ravera S, Parker S, Panfoli I, Benedicenti A, Benedicenti S (2016) An 808-nm diode laser with a flat-top handpiece positively photobiomodulates mitochondria activities. Photomed Laser Surg 34(11):564–571. https://doi.org/10.1089/pho.2015.4035
Passarella S, Karu T (2014) Absorption of monochromatic and narrow band radiation in the visible and near IR by both mitochondrial and non-mitochondrial photoacceptors results in photobiomodulation. J Photochem Photobiol B 140:344. https://doi.org/10.1016/j.jphotobiol.2014.07.021
Karu T, Pyatibrat L, Kalendo G (1995) Irradiation with He-Ne laser increases ATP level in cells cultivated in vitro. J Photochem Photobiol B 27:219–223. https://doi.org/10.1016/1011-1344(94)07078-3
Gorgey AS, Wadee AN, Sobhi NN (2008) The effect of low-level laser therapy on electrically induced muscle fatigue: a pilot study. Photomed Laser Surg 26:501–506. https://doi.org/10.1089/pho.2007.2161
Avni D, Levkovitz S, Maltz L, Oron U (2005) Protection of skeletal muscles from ischemic injury: low-level laser therapy increases antioxidant activity. Photomed Laser Surg 23:273–277. https://doi.org/10.1089/pho.2005.23.273
De Brito Vieira WH, Ferraresi C, de Andrade Perez SE, Baldissera V, Parizotto NA (2011) Effects of low-level laser therapy (808 nm) on isokinetic muscle performance of young women submitted to endurance training: a randomized controlled clinical trial. Lasers Med Sci 27(2):497–504. https://doi.org/10.1007/s10103-011-0984-0
Vanin AA, Verhagen E, Barboza SD, Costa LOP, Leal-Junior ECP (2018) Photobiomodulation therapy for the improvement of muscular performance and reduction of muscular fatigue associated with exercise in healthy people: a systematic review and meta-analysis. Lasers Med Sci 33(1):181–214. https://doi.org/10.1007/s10103-017-2368-6
Leal-Junior E, Lopes-Martins R, Bjordal JM (2019) Clinical and scientific recommendations for the use of photobiomodulation therapy in exercise performance enhancement and post-exercise recovery: current evidence and future directions. Braz J Phys Ther 23(1):71–75. https://doi.org/10.1016/j.bjpt.2018.12.002
Machado AF, Micheletti JK, Lopes JSS et al (2020) Phototherapy on management of creatine kinase activity in general versus localized exercise: a systematic review and meta-analysis. Clin J Sport Med 30(3):267–274. https://doi.org/10.1097/JSM.0000000000000606
Ferraresi C, de Brito Oliveira T, De Oliveira Zafalon L, DeMenezesReiff RB, Baldissera V, de Andrade Perez SE et al (2011) Effects of low level laser therapy (808 nm) on physical strength training in humans. Lasers Med Sci 26:349–358. https://doi.org/10.1007/s10103-010-0855-0
Vieira WHB, Ferraresi C, Andrade Perez SE, Baldissera V, Parizotto NA (2012) Effects of low-level laser therapy (808 nm) on isokinetic muscle performance of young women submitted to endurance training: a randomized controlled clinical trial. Lasers Med Sci 27(2):497–504. https://doi.org/10.1007/s10103-011-0984-0
Machado C dos SM, Casalechi HL, Vanin AA, de Azevedo JB, de Carvalho P de TC, Leal-Junior ECP (2020) Does photobiomodulation therapy combined to static magnetic field (PBMT-sMF) promote ergogenic effects even when the exercised muscle group is not irradiated? A randomized, triple-blind, placebo-controlled trial. BMC Sports Sci Med and Rehabil 12(1):49. https://doi.org/10.1186/s13102-020-00197-6
Dannecker EA, Koltyn KF (2014) Pain during and within hours after exercise in healthy adults. Sports Med 44:921–42. https://doi.org/10.1007/s40279-014-0172-z
Lau WY, Muthalib M, Nosaka K (2013) Visual analog scale and pressure pain threshold for delayed onset muscle soreness assessment. J Musculoskelet Pain 21:320–326. https://doi.org/10.3109/10582452.2013.848967
Antonialli FC, De Marchi T, Tomazoni SS, Vanin AA, dos Santos GV, de Paiva PR, Pinto HD, Miranda EF, de Tarso Camillo de Carvalho P, Leal-Junior EC (2014) Phototherapy in skeletal muscle performance and recovery after exercise: effect of combination of super-pulsed laser and light-emitting diodes. Lasers Med Sci 29(6):1967–76. https://doi.org/10.1007/s10103-014-1611-7
De Paiva PV, Tomazoni SS, Johnson DS, Vanin AA, Albuquerque-Pontes GM, Machado CSM, Casalechi HL, De Carvalho PTC, Leal-Junior ECP (2016) Photobiomodulation therapy (PBMT) and/or cryotherapy in skeletal muscle restitution, what is better? A randomized, double-blinded, placebo controlled clinical trial. Lasers Med Sci 31(9):1925–33. https://doi.org/10.1007/s10103-016-2071-z
Leal-Junior EC, Vanin AA, Miranda EF, de Carvalho PT, Dal Corso S, Bjordal JM (2015) Effect of phototherapy (low-level laser therapy and lightemitting diode therapy) on exercise performance and markers of exercise recovery: a systematic review with meta-analysis. Lasers Med Sci 30:925–939. https://doi.org/10.1007/s10103-013-1465-4
Ihsan FR (2005) Low-level laser therapy accelerates collateral circulation and enhances microcirculation. Photomed Laser Surg 23(3):289–94. https://doi.org/10.1089/pho.2005.23.289
Pinto HD, Vanin AA, Miranda EF, Tomazoni SS, Johnson DS, Albuquerque- Pontes GM, Junior AIO, Grandinetti VD, Casalechi HL, de Carvalho PT, Leal-Junior EC (2016) Photobiomodulation therapy improves performance and accelerates recovery of high-level rugby players in field test: a randomized, crossover, double-blind, placebo-controlled clinical study. J Strength Cond Res 30(12):3329–3338. https://doi.org/10.1519/jsc.0000000000001439
Batista JD, Sargenti-Neto S, Dechichi P, Rocha FS, Pagnoncelli RM (2015) Low-level laser therapy on bone repair: is there any effect outside the irradiated field? Lasers Med Sci 30(5):1569–1574. https://doi.org/10.1007/s10103-015-1752-3
Vanin AA, Miranda EF, Machado CSM, de Paiva PRV, Albuquerque-Pontes GM, Casalechi HL, Leal-Junior ECP (2016) What is the best moment to apply phototherapy when associated to a strength training program? A randomized, double-blinded, placebo-controlled trial. Lasers Med Sci 31(8):1555–1564. https://doi.org/10.1007/s10103-016-2015-7
Folland JP, Williams AG (2007) The adaptations to strength training: morphological and neurological contributions to increased strength. Sports Med 37:145–168. https://doi.org/10.2165/00007256-200737020-00004
Kadi F, Charifi N, Denis C, Lexell J, Andersen JL, Schjerling P, Olsen S, Kjaer M (2005) The behaviour of satellite cells in response to exercise: what have we learned from human studies? Pflugers Arch 451:319–327. https://doi.org/10.1007/s00424-005-1406-6
Mackey AL (2013) Does an NSAID a day keep satellite cells at bay? J Appl Physiol (1985) 115:900–908. https://doi.org/10.1152/japplphysiol.00044.2013
Leal-Junior ECP, de Oliveira MFD, Joensen J, Stausholm MB, Bjordal JM, Tomazoni SS (2020) What is the optimal time-response window for the use of photobiomodulation therapy combined with static magnetic field (PBMT-sMF) for the improvement of exercise performance and recovery, and for how long the effects last? A randomized, triple-blinded, placebo-controlled trial. BMC Sports Sci Med Rehabil 19(12):64. https://doi.org/10.1186/s13102-020-00214-8
Ferraresi C, de Sousa MV, Huang YY et al (2015) Time response of increases in ATP and muscle resistance to fatigue after low-level laser (light) therapy (LLLT) in mice. Lasers Med Sci 30(4):1259–67. https://doi.org/10.1007/s10103-015-1723-8
Acknowledgements
The author would like to thank the out clinic staff members at the Faculty of Physical Therapy, Cairo University, for their assistance and cooperation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This randomized double-blind study was followed the ethical principles of the Helsinki Declaration and approved by the Institutional Review Board of the Faculty of Physical Therapy at Cairo University (approval No: P.T.REC/012/002813). Written informed consent was obtained from all included patients.
Conflict of interest
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data citationMahran HG. Effect of photobiomodulation therapy on trunk flexor performance after incisional hernia repair: a randomized controlled trial Data sets.figshare. https://doi.org/10.6084/m9.figshare.14061458 (2021).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mahran, H.G. Effect of photobiomodulation therapy on trunk flexor performance after incisional hernia repair: a randomized controlled trial. Lasers Med Sci 37, 929–940 (2022). https://doi.org/10.1007/s10103-021-03337-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03337-7