Abstract
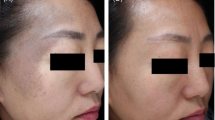
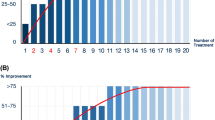
Q-Switched laser devices have been a standard treatment modality for dermal pigmentary disorders since the 1990s. However, the adverse events are sometimes intolerable even if the efficacy has been well accepted. These adverse events stop the patient from continuing the treatment and cause other cosmetic issues. Since 2012, the first picosecond laser for cosmetic applications was approved; it seems promising for treating pigmentary disorders in a new way, but lack strong evidence. We evaluated the efficacy and safety of a 755-nm picosecond laser for treatment of dermal pigmentary disorders in Asians. This is a 2-year retrospective study. We reviewed 36 female cases, including 8 cases of nevus of Ota and 28 cases of acquired bilateral nevus of Ota-like macules. Institutional Review Board (IRB) approval was granted by the Chang Gung Memorial Hospital medical research ethics committee (IRB 201900833B0). The epidemiologic data was collected. These patients have been treated with the 755-nm picosecond laser for 1 to 4 sessions at variable treatment interval. Our parameter settings were fluence of 2.73–3.98 J/cm2, with a spot size of 2.9 to 2.4 mm under the 650-ps mode. The pulse duration is 650 ps and fluence range is from 2.73 to 3.98 J/cm. Photographs were taken prior to every treatment and 1 month following the treatment. Two dermatologists conducted the clinical evaluation independently. Clinical improvement was observed in all with a minimal side effect. A total of 88.89% of patients had moderate to marked improvement in following 1 to 4 sessions. Transient swelling and erythema were observed in all patients but resolved within 24 h. Only one patient (2.78%) developed hypopigmentation and two patients (5.56%) had hyperpigmentation temporarily. Faster clearance could be achieved by the picosecond 755-nm laser for treating dermal pigmentary disorders in Asians. The treatment course is well tolerable and has minimal side effects.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Ee HL, Wong HC, Goh CL, Ang P (2006) Characteristics of Hori naevus: a prospective analysis. Br J Dermatol 154(1):50–53
Wang BQ, Shen ZY, Fei Y, Li H, Liu JH, Xu H, Zhang Z, Yu XH, Chen XD (2011) A population-based study of acquired bilateral nevus-of-Ota-like macules in Shanghai, China. J Invest Dermatol 131(2):358–362
Zhang Q, Jiang P, Tan C, Yang G (2017) Clinical profile and triggering factors for acquired, bilateral nevus of Ota-like macules. Cutan Ocul Toxicol 36(4):327–330
Lee WJ, Lee GY, Won KH, Won CH, Lee MW, Choi JH, Chang SE (2014) Comparison of acquired bilateral nevus of Ota-like macules in men and women. Indian J Dermatol Venereol Leprol 80(4):313–319
Geronemus RG (1992) Q-switched ruby laser therapy of nevus of Ota. Arch Dermatol 128(12):1618–1622
Pfeiffer N (1993) Q-switched ruby laser used to remove pigmented lesions. J Clin Laser Med Surg 11(3):147–148
Yang HY, Lee CW, Ro YS, Yu HJ, Kim YT, Kim JH, Kim JH (1996) Q-switched ruby laser in the treatment of nevus of Ota. J Korean Med Sci 11(2):165–170
Taylor CR, Flotte TJ, Gange RW, Anderson RR (1994) Treatment of nevus of Ota by Q-switched ruby laser. J Am Acad Dermatol 30(5 Pt 1):743–751
Alster TS, Williams CM (1995) Treatment of nevus of Ota by the Q-switched alexandrite laser. Dermatol Surg 21(7):592–596
Moreno-Arias GA, Camps-Fresneda A (2001) Treatment of nevus of Ota with the Q-switched alexandrite laser. Lasers Surg Med 28(5):451–455
Belkin DA, Jeon H, Weiss E, Brauer JA, Geronemus RG (2018) Successful and safe use of Q-switched lasers in the treatment of nevus of Ota in children with phototypes IV-VI. Lasers Surg Med 50(1):56–60
Yongqian C, Li L, Jianhai B, Ran H, Li G, Hao W, Xining W, Shigang X, Yibing W (2017) A split-face comparison of Q-switched Nd:YAG 1064-nm laser for facial rejuvenation in nevus of Ota patients. Lasers Med Sci 32(4):765–769
Cho SB, Park SJ, Kim MJ, Bu TS (2009) Treatment of acquired bilateral nevus of Ota-like macules (Hori’s nevus) using 1064-nm Q-switched Nd:YAG laser with low fluence. Int J Dermatol 48(12):1308–1312
Watanabe S, Takahashi H (1994) Treatment of nevus of Ota with the Q-switched ruby laser. N Engl J Med 331(26):1745–1750
Chang CJ, Nelson JS, Achauer BM (1996) Q-switched ruby laser treatment of oculodermal melanosis (nevus of Ota). Plast Reconstr Surg 98(5):784–790
Manuskiatti W, Sivayathorn A, Leelaudomlipi P, Fitzpatrick RE (2003) Treatment of acquired bilateral nevus of Ota-like macules (Hori’s nevus) using a combination of scanned carbon dioxide laser followed by Q-switched ruby laser. J Am Acad Dermatol 48(4):584–591
Shah VV, Bray FN, Aldahan AS, Mlacker S, Nouri K (2016) Lasers and nevus of Ota: a comprehensive review. Lasers Med Sci 31(1):179–185
Suh DH, Hwang JH, Lee HS, Youn JI, Kim PM (2000) Clinical features of Ota’s naevus in Koreans and its treatment with Q-switched alexandrite laser. Clin Exp Dermatol 25(4):269–273
Moody MN, Landau JM, Vergilis-Kalner IJ, Goldberg LH, Marquez D, Friedman PM (2011) 1,064-nm Q-switched neodymium-doped yttrium aluminum garnet laser and 1,550-nm fractionated erbium-doped fiber laser for the treatment of nevus of Ota in Fitzpatrick skin type IV. Dermatol Surg 37(8):1163–1167
Liu Y, Zeng W, Li D, Wang W, Liu F (2018) A retrospective analysis of the clinical efficacies and recurrence of Q-switched Nd:YAG laser treatment of nevus of Ota in 224 Chinese patients. J Cosmet Laser Ther 20(7–8):410–414
Chang CJ, Kou CS (2011) Comparing the effectiveness of Q-switched Ruby laser treatment with that of Q-switched Nd:YAG laser for oculodermal melanosis (nevus of Ota). J Plast Reconstr Aesthet Surg 64(3):339–345
Kagami S, Asahina A, Watanabe R, Mimura Y, Shirai A, Hattori N, Watanabe T, Tamaki K (2007) Treatment of 153 Japanese patients with Q-switched alexandrite laser. Lasers Med Sci 22(3):159–163
Yan L, Di L, Weihua W, Feng L, Ruilian L, Jun Z, Hui S, Zhaoxia Y, Weihui Z (2018) A study on the clinical characteristics of treating nevus of Ota by Q-switched Nd:YAG laser. Lasers Med Sci 33(1):89–93
Zong W, Lin T (2014) A retrospective study on laser treatment of nevus of Ota in Chinese children--a seven-year follow-up. J Cosmet Laser Ther 16(4):156–160
Kunachak S, Leelaudomlipi P, Sirikulchayanonta V (1999) Q-Switched ruby laser therapy of acquired bilateral nevus of Ota-like macules. Dermatol Surg 25(12):938–941
Lee WJ, Han Ss Fau-Chang SE, Chang Se Fau-Lee MW, Lee Mw Fau-Choi JH, Choi Jh Fau-Moon KC, Moon Kc Fau-Koh JK, Koh JK. Q-Switched Nd:YAG laser therapy of acquired bilateral nevus of Ota-like macules. (2005–3894 (Electronic))
Lam AY, Wong DS, Lam LK, Ho WS, Chan HH (2001) A retrospective study on the efficacy and complications of Q-switched alexandrite laser in the treatment of acquired bilateral nevus of Ota-like macules. Dermatol Surg 27(11):937–941 discussion 941-932
Chan HH, Leung RS, Ying SY, Lai CF, Kono T, Chua JK, Ho WS (2000) A retrospective analysis of complications in the treatment of nevus of Ota with the Q-switched alexandrite and Q-switched Nd:YAG lasers. Dermatol Surg 26(11):1000–1006
Wang B, Xie HF, Tan J, Xie HJ, Xu LY, Ding R, Liu FF, Chen X, Jian D, Li J (2016) Induction of melasma by 1064-nm Q-switched neodymium:yttrium-aluminum-garnet laser therapy for acquired bilateral nevus of Ota-like macules (Hori nevus): a study on related factors in the Chinese population. J Dermatol 43(6):655–661
Kunachak S, Leelaudomlipi P (2000) Q-switched Nd:YAG laser treatment for acquired bilateral nevus of ota-like maculae: a long-term follow-up. Lasers Surg Med 26(4):376–379
Freedman JR, Kaufman J, Metelitsa AI, Green JB (2014) Picosecond lasers: the next generation of short-pulsed lasers. Semin Cutan Med Surg 33(4):164–168
Yu W, Zhu J, Yu W, Lyu D, Lin X, Zhang Z (2018) A split-face, single-blinded, randomized controlled comparison of alexandrite 755-nm picosecond laser versus alexandrite 755-nm nanosecond laser in the treatment of acquired bilateral nevus of Ota-like macules. J Am Acad Dermatol 79(3):479–486
Wong THS (2018) Picosecond laser treatment for acquired bilateral nevus of Ota-like macules. JAMA Dermatol 154(10):1226–1228
Chan HH, Lam LK, Wong DS, Leung RS, Ying SY, Lai CF, Ho WS, Chua JK (2001) Nevus of Ota: a new classification based on the response to laser treatment. Lasers Surg Med 28(3):267–272
Hirayama T, Suzuki T (1991) A new classification of Ota’s nevus based on histopathological features. Dermatologica 183(3):169–172
Nam JH, Kim HS, Choi YJ, Jung HJ, Kim WS (2017) Treatment and classification of nevus of Ota: a seven-year review of a single institution’s experience. Ann Dermatol 29(4):446–453
Huang WH, Wang HW, Sun QN, Jin HZ, Liu YH, Ma DL, Zuo YG, Zheng HY, Wan K, Jing Q, Zhao YL (2013) A new classification of nevus of Ota. Chin Med J 126(20):3910–3914
Jerdan K, Hsu JT, Schnurstein E (2017) Successful treatment of Ota nevus with the 532-nm solid-state picosecond laser. Cutis 99(3):E29–e31
Chesnut C, Diehl J, Lask G (2015) Treatment of nevus of ota with a picosecond 755-nm alexandrite laser. Dermatol Surg 41(4):508–510
Sakio R, Ohshiro T, Sasaki K, Ohshiro T (2018) Usefulness of picosecond pulse alexandrite laser treatment for nevus of Ota. Laser Ther 27(4):251–255
Ohshiro T, Ohshiro T, Sasaki K, Kishi K (2016) Picosecond pulse duration laser treatment for dermal melanocytosis in Asians : a retrospective review. Laser Ther 25(2):99–104
Chan JC, Shek SY, Kono T, Yeung CK, Chan HH (2016) A retrospective analysis on the management of pigmented lesions using a picosecond 755-nm alexandrite laser in Asians. Lasers Surg Med 48(1):23–29
Levin MK, Ng E, Bae YS, Brauer JA, Geronemus RG (2016) Treatment of pigmentary disorders in patients with skin of color with a novel 755 nm picosecond, Q-switched ruby, and Q-switched Nd:YAG nanosecond lasers: a retrospective photographic review. Lasers Surg Med 48(2):181–187
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Yes, confirmed by the IRB committee
Informed consent
Yes
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, S., Yang, CS., Chang, SL. et al. Efficacy and safety of the picosecond 755-nm alexandrite laser for treatment of dermal pigmentation in Asians—a retrospective study. Lasers Med Sci 35, 1377–1383 (2020). https://doi.org/10.1007/s10103-020-02959-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-02959-7