Abstract
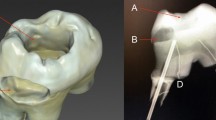
The objective of this proof-of-principle laboratory pilot study was to evaluate the temperature increase in the pulp chamber in a worst case scenario during Er:YAG laser debonding of all-ceramic crowns. Twenty extracted molars were prepared to receive all-ceramic IPS E.max CAD full contour crowns. The crowns were bonded to the teeth with Ivoclar Multilink Automix. Times for laser debonding and temperature rise in the pulp chamber using micro-thermocouples were measured. The Er:YAG was used with 560 mJ/pulse. The irradiation was applied at a distance of 5 mm from the crown surface. Additional air–water spray for cooling was utilized. Each all-ceramic crown was successfully laser debonded with an average debonding time of 135 ± 35 s. No crown fractured, and no damage to the underlying dentin was detected. The bonding cement deteriorated, but no carbonization at the dentin/cement interface occurred. The temperature rise in the pulp chamber averaged 5.4° ± 2.2 °C. During 8 out of the 20 crown removals, the temperature rise exceeded 5.5 °C, lasting 5 to 43 s (average 18.8 ± 11.6 s). A temperature rise of 11.5 °C occurred only once, while seven times the temperature rise was limited to 6.8 ± 0.5 °C. Temperature rises above 5.5 °C occurred only when the laser was applied from one side and additional cooling from the side opposite the irradiation. Er:YAG laser energy can successfully be used to efficiently debond all-ceramic crowns from natural teeth. Temperature rises exceeding 5.5 °C only occur when an additional air/water cooling from a dental syringe is inaccurately directed. To avoid possible thermal damage and to allow further heat diffusion, clinically temperature-reduced water might be applied.



Similar content being viewed by others
References
Deany IL (1996) Recent advances in ceramics for dentistry. Crit Rev Oral Biol Med 7(2):134–143
Shenoy A, Shenoy N (2010) Dental ceramics: an update. J Conserv Dent 13(4):195–203. doi:10.4103/0972-0707.73379
Bachhav VC, Aras MA (2011) Zirconia-based fixed partial dentures: a clinical review. Quintessence Int 42(2):173–182
Seghi RR, Denry IL, Rosenstiel SF (1995) Relative fracture toughness and hardness of new dental ceramics. J Prosthet Dent 74(2):145–150
Land MF, Hopp CD (2010) Survival rates of all-ceramic systems differ by clinical indication and fabrication method. J Evid Based Dent Pract 10(1):37–38. doi:10.1016/j.jebdp.2009.11.013
Guess PC, Zavanelli RA, Silva NR, Bonfante EA, Coelho PG, Thompson VP (2010) Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns: comparison of failure modes and reliability after fatigue. Int J Prosthodont 23(5):434–442
Marchack BW, Sato S, Marchack CB, White SN (2011) Complete and partial contour zirconia designs for crowns and fixed dental prostheses: a clinical report. J Prosthet Dent 106(3):145–152. doi:10.1016/S0022-3913(11)60112-1
Siegel SC, von Fraunhofer JA (1999) Comparison of sectioning rates among carbide and diamond burs using three casting alloys. J Prosthodont 8(4):240–244
Yener ES, Ozcan M, Kazazoglu E (2011) The effect of glazing on the biaxial flexural strength of different zirconia core materials. Acta Odontol Latinoam 24(2):133–140
Tysowsky GW (2009) The science behind lithium disilicate: a metal-free alternative. Dent Today 28(3):112–113
Engelberg B (2013) An effective removal system for zirconia and lithium-disilicate restorations. Inside Dent :92–98
Keller U, Hibst R (1995) Histological findings of pulpal changes after Er:YAG laser irradiation. J Dent Res 74(1159):545
Hibst R, Keller U (1991) Removal of dental filling materials by Er:YAG laser radiation. In: O’Brien SJ, Dederich DN, Wigdor HA, Trent AM (eds), Bellingham, Washington. SPIE Proceedings of Lasers in Orthopedic, Dental and Veterinary Medicine. SPIE 1424, pp 120–126
Correa-Afonso AM, Palma-Dibb RG, Pecora JD (2010) Composite filling removal with erbium:yttrium-aluminum-garnet laser: morphological analyses. Lasers Med Sci 25(1):1–7. doi:10.1007/s10103-008-0581-z
Morford CK, Buu NC, Rechmann BM, Finzen FC, Sharma AB, Rechmann P (2011) Er:YAG laser debonding of porcelain veneers. Lasers Surg Med 43(10):965–974. doi:10.1002/lsm.21144
Buu NC, Morford CK, Finzen FC, Sharma A, Rechmann P (2010) Er:YAG laser debonding of porcelain veneers. Lasers in Dentistry XVI, SPIE Proceedings 7549, San Francisco
Rechmann P, Buu NC, Rechmann BM, Le CQ, Finzen FC, Featherstone JD (2014) Laser all-ceramic crown removal-a laboratory proof-of-principle study-phase 1 material characteristics. Lasers Surg Med 46(8):628–635. doi:10.1002/lsm.22279
Rechmann P, Buu NC, Rechmann BM, Finzen FC (2014) Laser all-ceramic crown removal—a laboratory proof-of-principle study-phase 2 crown debonding time. Lasers Surg Med 46(8):636–643. doi:10.1002/lsm.22280
Fried D, Zuerlein MJ, Featherstone DB, Seka W, Duhn C, McCormack SM (1998) IR laser ablation of dental enamel: mechanistic dependence on the primary absorber. Appl Surf Sci 127–129:852–856
Lizarelli RFZ, Moriyama LT, Pelino JEP, Bagnato VS (2005) Ablation rate of morphological aspects of composite resin exposed to Er:YAG laser. J Oral Laser Appl 3:151–160
Pich O, Franzen R, Gutknecht N, Wolfart S (2013) Laser treatment of dental ceramic/cement layers: transmitted energy, temperature effects and surface characterisation. Lasers Med Sci 30(2):591–597. doi:10.1007/s10103-013-1340-3
Chiodera G, Gastaldi G, Millar BJ (2009) Temperature change in pulp cavity in vitro during the polymerization of provisional resins. Dent Mater 25(3):321–325. doi:10.1016/j.dental.2008.08.006
Seelbach P, Finger WJ, Ferger P, Balkenhol M (2010) Temperature rise on dentin caused by temporary crown and fixed partial denture materials: influencing factors. J Dent 38(12):964–973. doi:10.1016/j.jdent.2010.08.008
Michalakis K, Pissiotis A, Hirayama H, Kang K, Kafantaris N (2006) Comparison of temperature increase in the pulp chamber during the polymerization of materials used for the direct fabrication of provisional restorations. J Prosthet Dent 96(6):418–423. doi:10.1016/j.prosdent.2006.10.005
Hansen EK, Asmussen E (1993) Correlation between depth of cure and temperature rise of a light-activated resin. Scand J Dent Res 101(3):176–179
Huang TK, Hung CC, Tsai CC (2006) Reducing, by pulse width modulation, the curing temperature of a prototype high-power LED light curing unit. Dent Mater J 25(2):309–315
Choi S, Roulet J, Heintze S, Park S (2014) Influence of cavity preparation, light-curing units, and composite filling on intrapulpal temperature increase in an in vitro tooth model. Oper Dent 39(5):E195–205. doi:10.2341/13-068-L
Karaarslan ES, Secilmis A, Bulbul M, Yildirim C, Usumez A (2011) Temperature increase beneath etched dentin discs during composite polymerization. Photomed Laser Surg 29(1):47–52. doi:10.1089/pho.2009.2713
Hahn P, Schondelmaier N, Wolkewitz M, Altenburger MJ, Polydorou O (2013) Efficacy of tooth bleaching with and without light activation and its effect on the pulp temperature: an in vitro study. Odontology / Soc Nippon Dent Univ 101(1):67–74. doi:10.1007/s10266-012-0063-4
Klaric E, Rakic M, Sever I, Tarle Z (2013) Temperature rise during experimental light-activated bleaching. Lasers Med Sci 30(2):567–576. doi:10.1007/s10103-013-1366-6
Eldeniz AU, Usumez A, Usumez S, Ozturk N (2005) Pulpal temperature rise during light-activated bleaching. J Biomed Mater Res B Appl Biomater 72(2):254–259. doi:10.1002/jbm.b.30144
Sulieman M, Addy M, Rees JS (2005) Surface and intra-pulpal temperature rises during tooth bleaching: an in vitro study. Br Dent J 199(1):37–40. doi:10.1038/sj.bdj.4812558, discussion 32
Knappe V, Frank F, Rohde E (2004) Principles of lasers and biophotonic effects. Photomed Laser Surg 22(5):411–417. doi:10.1089/pho.2004.22.411
Joffe SN (2003) Lasers in medicine, vol 2: Las-Pho. Encyclopedia of optical engineering, vol 3. Marcel Dekker, New York
Zach L, Cohen G (1965) Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 19:515–530
Lloyd CH, Joshi A, McGlynn E (1986) Temperature rises produced by light sources and composites during curing. Dent Mater J 2(4):170–174
Baldissara P, Catapano S, Scotti R (1997) Clinical and histological evaluation of thermal injury thresholds in human teeth: a preliminary study. J Oral Rehabil 24(11):791–801
Henriques FC Jr (1947) Studies of thermal injury; the predictability and the significance of thermally induced rate processes leading to irreversible epidermal injury. Arch Pathol 43(5):489–502
Denton ML, Clark CD, Foltz MS, Schuster KJ, Noojin GD, Estlack LE, Thomas RJ (2010) In-vitro retinal model reveals a sharp transition between laser damage mechanisms. J Biomed Opt 15(3):030512. doi:10.1117/1.3449107
Hennig T, Rechmann P, Abel M (1994) Caries selective ablation: effects of water cooling. In: Bown SG, Escourrou J, Frank F et al (eds), Bellingham, Washington, 1994. SPIE Proceedings of Medical Applications of Lasers II. SPIE, pp 70–75
Hennig T, Rechmann P, Holtermann A (1994) Caries selective ablation: temperature in the pulp chamber. In: Anderson R, Katzir A (eds), Bellingham, Washington, 1994. SPIE Proceedings of Laser Surgery: Advanced, Characterization, Therapeutics, and Systems IV. SPIE, pp 397–402
Hennig T, Rechmann P, Holtermann A, Dramburg R (1994) Caries selective ablation—temperature in the pulp chamber. P Soc Photo-Opt Ins 2128:397–402. doi:10.1117/12.184923
Secilmis A, Bulbul M, Sari T, Usumez A (2013) Effects of different dentin thicknesses and air cooling on pulpal temperature rise during laser welding. Lasers Med Sci 28(1):167–170. doi:10.1007/s10103-012-1108-1
Raab WH (1992) Temperature related changes in pulpal microcirculation. Proc Finn Dent Soc 88(Suppl 1):469–479
Kodonas K, Gogos C, Tziafas D (2009) Effect of simulated pulpal microcirculation on intrapulpal temperature changes following application of heat on tooth surfaces. Int Endod J 42(3):247–252. doi:10.1111/j.1365-2591.2008.01508.x
Compliance with ethical standards
Conflict of interest
The authors declare that there is no conflict of interest that should be reported regarding this manuscript.
Funding
This is a PI-initiated study partially sponsored by Department Discretionary Funds and partially sponsored by Ivoclar Vivadent AG.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rechmann, P., Buu, N.C.H., Rechmann, B.M.T. et al. Laser all-ceramic crown removal and pulpal temperature—a laboratory proof-of-principle study. Lasers Med Sci 30, 2087–2093 (2015). https://doi.org/10.1007/s10103-015-1738-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-015-1738-1



