Abstract
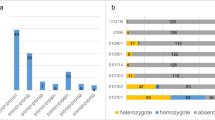
Persistent high-risk human papillomavirus (HR-HPV) infection is the key event in the progression of HPV lesions, and more data are urgently needed on asymptomatic oral HPV infections in men. Asymptomatic fathers-to-be (n = 131, mean age 28.9 years) were enrolled in the cohort, sampled by serial oral scrapings at baseline and at 2-month, 6-month, 12-month, 24-month, 36-month, and 7-year follow-up visits to accomplish persistent and cleared HPV infections. HPV genotyping was performed using nested PCR and Multimetrix® assay. Covariates of persistent and cleared oral HPV infections were analysed using generalised estimating equation (GEE) and Poisson regression. Altogether, 17 HPV genotypes were detected in male oral mucosa point prevalence, varying from 15.1 % to 31.1 %. Genotype-specific HPV persistence was detected in 18/129 men the mean persistence time ranging from 6.0 to 30.7 months. History of genital warts decreased (p = 0.0001; OR = 0.41, 95 % CI 0.33−0.51) and smoking increased (p = 0.033, OR = 1.92, 95 % CI 1.05−3.50) the risk of persistent species 7/9 HPV infections. Of the 74 HPV-positive men, 71.6 % cleared their infection actuarial and crude clearance times, varying between 1.4 and 79.6 months. No independent predictors were identified for species 7/9 clearance. At the last follow-up-visit, 50.1 % of the fathers had oral mucosal changes, correlating only with smoking (p = 0.046). To conclude, most of the persisting oral infections in males were caused by HPV16. Smoking increased while previous genital warts decreased oral HR-HPV persistence. No predictors of HR-HPV clearance were disclosed.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Syrjänen S (2007) Human papillomaviruses in head and neck carcinomas. N Engl J Med 356:1993–1995. doi:10.1056/NEJMe078004
Kreimer AR, Clifford GM, Boyle P, Francecschi S (2005) Human papillomavirus types in head and neck squamous cell carcinomas worldwide: A systematic review. Cancer Biomarkers Prev 14:467–475. doi:10.1158/1055-9965
Rautava J, Syrjänen S (2012) Biology of human papillomavirus infection in head and neck carcinogenesis. Head and Neck Pathol 6:S3–S15. doi:10.1007/s12105-012-0367-2
Gillison ML (2004) Human papillomavirus-associated head and neck cancer is a distinct epidemiologic, clinical, and molecular entity. Semin Oncol 31:744–754
Kero K, Rautava J, Syrjänen K, Grenman S, Syrjänen S (2012) Oral mucosa as a reservoir of human papillomavirus: Point prevalence, genotype distribution, and incident infections among males in a 7-year prospective study. Eur Urol 62:1063–1070. doi:10.1016/j.eururo.2012.06.045
Kero K, Rautava J, Syrjänen K, Grenman S, Syrjänen S (2012) Reply from authors re: Guido Barbagli, Salvatore Sansalone, Massimo Lazzeri. Oral mucosa and urethroplasty: it’s time to change. Oral mucosa as a reservoir of human papillomavirus: implications for the use of oral transplants in urethroplasty. Eur Urol 62:1073–1075
Kreimer AR, Villa A, Nyitray AG, Abrahamsen M, Papenfuss M et al (2011) The epidemiology of oral HPV infection among a multinational sample of healthy men. Cancer Epidemiol Biomarkers Prev 20:172–182. doi:10.1158/1055-9965.EPI-10-0682
D’Souza G, Agrawal Y, Halpern J, Bodison S, Gillison ML (2009) Oral sexual behaviors associated with prevalent oral human papillomavirus infection. J Infect Dis 199:1263–1269. doi:10.1086/597755
Gillison ML, Broutian T, Pickard RK, Tong ZY, Xiao W et al (2012) Prevalence of oral HPV infection in the United States, 2009–2010. JAMA 15:693–703. doi:10.1001/jama.2012.101
Terai M, Hashimoto K, Yoda K, Sata T (1999) High prevalence of human papillomavirus in normal oral cavity of adults. Oral Microbiol Immunol 14:201–205
Rintala M, Grenman S, Puranen M, Syrjänen S (2006) Natural history of oral papillomavirus infections in spouses: A prospective Finnish HPV family study. J Clin Virol 35:89–94. doi:10.1016/j.jcv.2005.05.012
Rintala M, Grenman S, Puranen M, Isolauri E, Ekblad U et al (2005) Transmission of high-risk human papillomavirus (HPV) between parents and infant: A prospective study of HPV in families in Finland. J Clin Microbiol 43:376–381. doi:10.1128/JCM.43.1.376-381.2005
Louvanto K, Rintala MA, Syrjänen KJ, Grenman SE, Syrjänen SM (2011) Incident cervical infections with high- and low-risk human papillomavirus (HPV) infections among mothers in the prospective Finnish family HPV study. BMC Infect Dis 22(11):179. doi:10.1186/1471-2334-11-179
Louvanto K, Rintala MA, Syrjänen KJ, Grenman SE, Syrjänen SM (2010) Genotype-specific persistence of genital human papillomavirus (HPV) infections in women followed for 6 years in the Finnish family HPV study. J Infect Dis 202:436–444. doi:10.1086/653826
Louvanto K, Syrjänen K, Rintala M, Grenman S, Syrjänen S (2010) Genotype-specific clearance of genital human papillomavirus (HPV) infections among mothers in the Finnish family HPV study. J Clin Microbiol 48:2665–2671. doi:10.1128/JCM.00783-10
Rautava J, Willberg J, Louvanto K, Wideman L, Syrjänen K et al (2012) Prevalence, genotype distribution and persistence of human papillomavirus in oral mucosa of women: A Six-year follow-up study. PLOS One 7:e42171. doi:10.1371/journal.pone.0042171
Rintala MA, Louvanto K, Rantanen V, Grénman SE, Syrjänen KJ, Syrjänen SM (2012) High-risk human papillomavirus associated with incident cervical intraepithelial neoplasia developing in mothers in the Finnish family HPV study cohort. Scand J Infect Dis 44:115–125. doi:10.3109/00365548.2011.619999
Parisi SG, Cruciani M, Scaggiante R, Boldrin C, Andreis S et al (2011) Anal and oral human papillomavirus (HPV) infection in HIV-infected subjects in northern Italy: A longitudinal cohort study among men who have sex with men. BMC Infect Dis 11:150. doi:10.1186/1471-2334-11-150
D'Souza G, Fakfry C, Sugar EA, Seaberg EC, Weber K et al (2007) Six-month natural history of oral versus cervical human papillomavirus infection. Int J Cancer 121:143–150. doi:10.1002/ijc.22667
Kurose K, Terai M, Soedarsono N, Rabello D, Nakajima Y et al (2004) Low prevalence of HPV infection and its natural history in normal oral mucosa among volunteers on Miyako Island, Japan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98:91–96
Beachler DC, Weber KM, Margolick JB, Strickler HD, Cranston RD et al (2012) Risk factors for oral HPV infection among a high prevalence population of HIV-positive and at-risk HIV-negative adults. Cancer Epidemiol Biomarkers Prev21:122–133.. doi: 10.1158/1055-9965.EPI-11-0734
Miller S, Dykes D, Polesky H (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16:1215
Schmitt M, Bravo IG, Snijders PJ, Gissman L, Pawlita M et al (2006) Bead-based multiplex genotyping of human papillomaviruses. J Clin Microbiol 44:504–12. doi:10.1128/JCM.44.2.504-512.2006
Diggle PJ, Liang K-Y, Zeger SL (1994) Analysis of longitudinal data, 1st edn. Oxford University Press, Oxford
Hardin J, Hilbe JM (2003) Generalized estimating equations. Chapman and Hall, Boca Raton
Zur Hausen H (1989) Papillomaviruses in anogenital cancer as a model to understand the role of viruses in human cancers. Cancer Res 49:4677–4681
Kero K, Rautava J, Syrjänen K, Grenman S, Syrjänen S (2011) Human papillomavirus genotypes in male genitalia and their concordance among pregnant spouses participating in the Finnish family HPV study. J Sex Med 8:2522–31. doi:10.1111/j.1743-6109.2011.02378.x
Labriola A, Needleman I, Moles DR (2000) Systematic review of the effect of smoking on non-surgical periodontal therapy. Peridontology 37:124–137
Stanley MA (2012) Epithelial cell responses to infection with human papillomavirus. Clin Microbiol Rev 25:215–222. doi:10.1128/CMR.05028-11
Syrjänen K, Syrjänen S (2000) Papillomavirus infections in human diseases. J. Wiley & Sons, New York, pp 1–615
Pickard RK, Xiao W, Broutian TR, He X, Gillison ML (2012) The prevalence and incidence of human papillomavirus infection among young men and women, aged 18–30 years. Sex Transm Dis 39:559–566. doi:10.1097/OLQ.0b013e31824f1c65
Louvanto K, Rautava J, Willberg J, Wideman L, Syrjänen K, Syrjänen S (2013) Genotype-specific incidence and clearance of human papillomavirus in oral mucosa of women: a six-year-follow-up-study. PLoS ONE 8(1):e53413. doi:10.1371/journal.pone.0053413
Acknowledgements
The authors thank Dr. Marjut Rintala, Dr. Virpi Rantanen and midwife Elisa Hovimäki for the enrolment and follow-up of the study. The skilful technical assistance of Mrs. Tatjana Peskova, Mariia Henttinen and Keitlin Adel is gratefully acknowledged.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kero, K., Rautava, J., Syrjänen, K. et al. Smoking increases oral HPV persistence among men: 7-year follow-up study. Eur J Clin Microbiol Infect Dis 33, 123–133 (2014). https://doi.org/10.1007/s10096-013-1938-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-013-1938-1
Keywords
Profiles
- K. Kero View author profile