Abstract
Objective
Socioeconomic and health inequalities persist in multicultural western countries. Here, we compared outcomes following an acute stroke amongst ethnic minorities with Caucasian patients.
Methods
Data were prospectively collected (2014–2016) from the Sentinel Stroke National Audit Programme for 3309 patients who were admitted with an acute stroke in four UK hyperacute stroke units. Associations between variables were examined by chi-squared tests and multivariable logistic regression, adjusted for age, sex, prestroke functional limitations and co-morbidities, presented as odds ratios (OR) with 95% CI.
Results
There were 3046 Caucasian patients, 95 from ethnic minorities (mostly South Asians, Blacks, mixed race and a few in other ethnic groups) and 168 not stated. Compared with Caucasian patients, those from ethnic minorities had a proportionately higher history of diabetes (33.7% vs 15.4%, P < 0.001), but did not differ in other chronic conditions, functional limitations or sex distribution. Their age of stroke onset was younger both in women (76.8 year vs 83.2 year, P < 0.001) and in men (69.5 year vs 75.9 year, P = 0.002). They had greater risk for having a stroke before the median age of 79.5 year: OR = 2.15 (1.36–3.40) or in the first age quartile (< 69 year): OR = 2.91 (1.86–4.54), requiring palliative care within the first 72 h: OR = 3.88 (1.92–7.83), nosocomial pneumonia or urinary tract infection within the first 7 days of admission: OR = 1.86 (1.06–3.28), and in-hospital mortality: OR = 2.50 (1.41–4.44).
Conclusions
Compared with Caucasian patients, those from ethnic minorities had earlier onset of an acute stroke by about 5 years and a 2- to fourfold increase in many stroke-related adverse outcomes and death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-income countries such as the UK and USA, as well as many western European countries are multicultural societies that are in constant dynamic change in population profile due to immigration and emigration [1]. In the UK, there is a progressive increase in people with ethnic minority backgrounds. The 2021 UK population census of 67 million found that the largest ethnic group was Caucasian (85.4%), followed by Asian or Asian British (7.8%), Black (3.5%), mixed race (2.3%) and others (1%) [2]. The Sentinel Stroke National Audit Programme (SSNAP) data showed that amongst all patients admitted with an acute stroke in England, Wales and Northern Ireland in 2015–2016 and in 2016–2017, there were 88.4% Caucasian, 5.6% ethnic minorities and 6.1% unknown [3]. Several studies have demonstrated that many people from ethnic minorities living in western countries endure racial discrimination, as well as socio-economic inequalities that include reduced access to quality housing, education, employment, healthcare services and the judicial system [4,5,6]. These disparities often coexist with many chronic health conditions such as diabetes and cardiovascular disease [7], poor mental health [8] greater incidence of stillbirth and infant deaths and a shorter life expectancy [7, 9].
National initiatives have promoted improvement in healthcare for individuals from ethnic minorities through scientific and clinical research [4, 10, 11]. However, progress to identify and reduce health inequalities has been hampered by a lack of detailed documentation of ethnicity [12], especially when examining mortality [7]. Furthermore, clinical quality-care outcomes for ethnic minority groups admitted to hospital have not been well-documented. In this study of ethnic differences in health amongst patients who presented with an acute stroke, we sought to examine three broad areas: firstly, their characteristics including sex, co-morbidities and pre-stroke disability; secondly, management of their stroke, including swallow screening, thrombolysis and its complications and supportive care during admission; and thirdly clinical outcomes including severity of stroke, nosocomial infections, malnutrition, prolonged hospital length of stay (LOS), post-stroke disability, in-hospital mortality and supportive care at discharge.
Methods
Study design, participants and setting
This study was part of the SSNAP [3]. We prospectively collected data from 3309 patients who were consecutively admitted with an acute stroke to four UK hyperacute stroke units (HASU) in the south of England, from January 2014 to February 2016 [13]. There were 3046 (92.1%) patients from a Caucasian background and 95 (2.9%) from an ethnic minority background. The remaining 168 (5.1%) were patients whose ethnicity was not stated (Supplementary material 1).
Socio-demographic factors and medical history
Details of socio-demographic factors were documented by the stroke team including age at diagnosis, sex, history of previous stroke, hypertension, diabetes mellitus congestive heart failure and atrial fibrillation [3, 13].
Stroke diagnosis and severity
Diagnosis was based on clinical presentation and neuroimaging [3, 13]. The National Institutes of Health for Stroke Scale (NIHSS) was used to assess the severity of stroke symptoms at arrival, with a score range from no symptoms (minimum score = 0) to severe stroke symptoms (maximum score = 42) [13].
Swallow screening and nutrition status
Swallow screening was carried out within target of 4 h of stroke diagnosis. Oral fluid, food or medication was allowed if there was no risk of aspiration [14]. The risk of malnutrition was assessed by the Malnutrition Universal Screening Test (MUST) protocol [15].
Disability, mortality, palliative care and nosocomial infections
Disability or dependence on daily activities prior to the occurrence of stroke and also at discharge was assessed by the modified Rankin scale (mRS). The mRS scores range from 0 to 6, with a higher the score indicating a greater severity (mRS score = 6 indicates death) [16]. Palliative care within 72 h of admission was recorded to reflect a patient’s poor outcome [3]. Pneumonia and urinary tract infections (UTI) requiring antibiotic treatment acquired within 7 days of admission were documented [3, 13].
Thrombolysis and immediate thrombolysis-related complications
Thrombolysis was carried out in patients according to current guidelines (intravenous recombinant tissue plasminogen activator agent alteplase) including confirmed diagnosis of acute ischaemic stroke (AIS), onset to arrival time of less than 4.5 h and without contra-indications [3, 13]. Immediate thrombolysis-related complications, including symptomatic intracranial haemorrhage, were examined by imaging evidence of intracerebral haemorrhage in conjunction with a significant decline in neurological function [3, 17], whilst severe hypertension, acute orolingual angioedema, anaphylaxis and acute systemic haemorrhage were assessed by clinical examination.
Level of care support planned at discharge
The level of care-support was planned for patients on discharge included the frequency of home visits per week, help for activity of daily living and joint-care planning between health and social care. Information was also documented on discharge to a new temporary or permanent care home [3, 13].
Categorisation of variables
All patients from ethnic minority backgrounds were combined into a single category in this study due to their relatively small numbers for comparison with Caucasian patients. For clarity of presentation, the term “ethnic differences” indicates comparisons of outcomes in Caucasians against all patients from ethnic minorities. Moderately severe to severe disability was defined as an mRS score ≥ 4, and moderately severe to severe stroke was defined as an NIHSS score ≥ 16. Prolonged LOS was defined as those who spent longer than 3 weeks (top quartile) in HASU. Swallow screening status was categorised into groups: screening performed within 4 h, 4–72 h and > 72 h of stroke diagnosis [3, 14]. Nutrition status was classified as well-nourished (MUST score = 0) and at risk of malnutrition (MUST score ≥ 1). Age stratification was based on group median value (79.5 years) or interquartile groups (< 68.9, 70–79.4, 79.5–86.9 and ≥ 87 years).
Statistical analysis
The associations of subject characteristics, management care and outcomes in relation to ethnicity were explored by chi-squared tests. Mann–Whitney U tests were conducted to test ethnic differences in non-parametric data (age of stroke onset). Multivariable logistic regression was conducted to estimate the risk of primary clinical outcomes including early onset of stroke (before the median or first quartile of group age), severe stroke, nosocomial infections (urinary tract infection or pneumonia) within 7 days of admission, malnutrition, prolonged LOS on HASU, disability at discharge, palliative care within the first 72 h of admission and mortality during hospital admission (dependent variables) for patients from ethnic minorities; patients from a Caucasian background were used as a reference group (independent variable). The results are presented as two models, adjusted for confounding factors: model 1, adjusted for age, and model 2, adjusted for age (except for analysis of age of stroke onset), sex, co-morbidities, pre-stroke disability (mRS) and type of stroke (ICH). The selection of these potential confounding factors was determined a priori, i.e., on the basis of pre-existing knowledge of their clinical risk associated with individuals from ethnic minority backgrounds and also with outcome measures [3, 7]. The results were expressed as odds ratios (OR) and 95% confidence intervals (CI). The goodness-of-fit for logistic regression was assessed by the Hosmer–Lemeshow test. Analyses were performed using SPSS Statistics for Windows, v.28.0 (IBM Corp., Armonk, NY, USA).
Results
The sex distribution was similar in Caucasian and ethnic minority groups. At presentation, there were no ethnic differences in the occurrence of intracranial haemorrhagic stroke and underlying co-morbidities, except a high proportion of diabetes amongst the ethnic minority group, which was observed across all age groups (Fig. 1). Amongst stroke patients with coexisting atrial fibrillation, the proportions without treatment by either an anticoagulant or antiplatelet did not differ between Caucasian and ethnic minority patients (Table 1).
Compared to the reference group, there were proportionally more patients in the ethnic minority group with stroke onset before the median age of 79.5 years (66.3% vs 49.5%, P < 0.001), or before 69 years (44.2% vs 24.4%, P < 0.001) (Table 1). The median age of onset of stroke was about 5 years earlier both in women (76.8 years vs 83.2 years, P < 0.001) and in men (69.5 years vs 75.9 years, P = 0.002). Thus, men from ethnic minorities had almost 14 years earlier onset of stroke than Caucasian women (Fig. 2). There were no ethnic differences in all care quality measures (Table 1). Unadjusted analysis showed higher proportions amongst the ethnic minority group for pneumonia within 7 days of admission (18.3% vs 11.0%, P = 0.020) and those requiring palliative care within the first 72 h of admission (12.6 vs 5.6, P = 0.009); mortality and moderately-severe to severe stroke were also higher but did not achieve significance. The remaining outcomes, including prolonged LOS on HASU, UTI, risk of malnutrition or disability on discharge, did not differ between Caucasians and the ethnic minority group. There were also no ethnic differences in provision of discharge support.
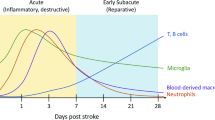
Further analysis, using age stratification at the group median value (79.5 years), revealed that the ethnic minority group had a higher proportion of moderately severe to severe stroke only in the younger age group (Fig. 3A), whilst palliative care in the first 72 h (Fig. 3B), nosocomial infections (Fig. 3C) and mortality (Fig. 3D) were higher in all age groups, more markedly in older age (Fig. 4). Although there were no ethnic differences in severity and type of stroke in younger age, moderately severe to severe stroke occurred more frequently in ethnic minority groups than in Caucasians both for ischaemic (11.5% vs 6.0%) and haemorrhagic stroke (12.5% vs 9.7%).
Rates of moderately-severe to severe stroke (A), palliative care within the first 72 h (B) and nosocomial infections within 7 days of admission (C), and in-hospital mortality (D) classified by median of age amongst Caucasians and ethnic minority individuals admitted with a stroke to hyperacute stroke units
Multivariable logistic regression (Caucasian background as reference), adjusted for age, sex, prestroke functional limitations and co-morbidities, showed that patients from ethnic minority backgrounds had greater risk for having a stroke < 79.5 years: OR = 2.15 (1.36–3.40) or < 69 years: OR = 2.91 (1.86–4.54), requiring palliative care within the first 72 h: OR = 3.88 (95% CI = 1.92–7.83), nosocomial pneumonia within 7 days: OR = 2.34 (1.30–4.23), nosocomial pneumonia or urinary tract infections within 7 days of admission: OR = 1.86 (1.06–3.28), and in-hospital mortality: OR = 2.50 (1.41–4.44) (Table 2).
Additional analysis was conducted for the group of patients whose ethnic backgrounds were unknown. In general, their characteristics (Supplementary material Table 2) and outcomes (Supplementary material Table 3) lay between those of Caucasians and ethnic minorities.
Discussion
Summary of findings
In this study of ethnic differences in health amongst patients admitted with an acute stroke, a number of important findings emerged. The onset of stroke both in men and women from ethnic minorities was approximately 5 years earlier than their Caucasian counterparts, whilst men from ethnic minorities had nearly 14 years earlier of onset than Caucasian women. After adjustments for potential confounding factors, despite their younger age at presentation, patients from ethnic minorities had 2- to fourfold greater risk of many adverse outcomes including severe stroke, requirement for palliative care within the first 72 h, nosocomial infection within the first 7 days and mortality in hospital. Other than a higher proportion of diabetes in patients from ethnic minorities, which is similarly observed in previous studies [18], the two ethnic groups were well-matched for the remaining major co-morbidities and prestroke disability. The two study groups had equal management for stroke care from the time of admission to discharge. Our findings suggest that more research is needed to identify the aetiology of these disparities to reduce their differences.
It has been long recognised that social inequalities are major determinants of poor health. These gaps appear to have widened in many parts of the UK in the twenty-first century [19]. Ethnic minorities disproportionately represent the lower levels of socioeconomic strata in the UK [20, 21] and in the USA [22]. Although some ethnic groups, such as Asians of Indian or Chinese origin, have moved up the socioeconomic ladder, with relatively high proportions attaining high level of education and occupying certain managerial level, they continue to encounter barriers to their potential because of racial discrimination [23]. These factors are thought to exert profound adverse effects on their physical and mental health (see below).
The observation of an earlier onset of stroke amongst ethnic minorities, which is consistent with previous studies [18], has several important implications. The younger age of onset results in longer years of disability amongst survivors, with greater chance of recurrent strokes and death. This would impose great social, healthcare service and financial burdens to the patient and carers, as well as their dependent relatives. The underlying reason for this early stroke onset is not clear, but certain factors such as poorer lifestyle (diet, smoking and exercise) and obesity may contribute. Those from ethnic minorities may also be less willing to seek timely medical advice and health checks which may delay preventative treatment such as cardiometabolic control. A recent review of ethnic studies amongst patients with multiple chronic conditions showed that Black people were least likely to be prescribed statins and to reach set targets for blood pressure, glycated haemoglobin A1c (HbA1c) and total cholesterol levels, whilst South Asian patients were least likely to meet targets for HbA1c levels [24]. We observed that the proportion of untreated atrial fibrillation either by an anticoagulant or antiplatelet in ethnic minority group was similar to that in Caucasian group. Studies in the USA [25] and the UK [26] revealed that patients from ethnic minority groups were more likely to report perceived provider racial discrimination, which is associated with poorer health compared to Caucasian individuals and is thought to lead to a delay in seeking clinical assessment and treatment. Similar findings have been reported amongst ethnic minorities in the use of mental health services in the UK [27], whilst such services may not even be legally available to immigrants in some European countries [28]. We found nearly all patients were admitted to HASU within 72 h of hospital admission and the proportion of Caucasians (93.5%) did not differ significantly from that of ethnic minorities (94.4%). This observation, and the similarity in other care quality measures between ethnic groups, indicates that the level of care for stroke was unlikely to contribute to ethnic differences in outcome.
Representation of ethnic minorities has only been documented sporadically in SSNAP annual reports. In 2016, there was a total of 4661 stroke patients recorded by participating HASUs in the UK (excluding Scotland which does not participate in SSNAP). This figure rose slightly to 4706 in 2017 [3]. In both years, there were 5.6% of patients from ethnic minorities. Surprisingly, quality-care outcomes in patients from ethnic minority background have never been presented in these national reports. Our findings, as part of this national audit programme, provide crucial evidence of health inequalities endured by ethnic minority groups and should serve as a stimulus for detailed analysis of clinical outcomes amongst ethnic minorities at a national level. Studies of ethnic differences in health commonly use data derived from health records. When information on ethnicity is not available, e.g., death registration, country of birth of migrants has been used as a proxy for ethnicity, but this does not take second-generation migrants into account leading to substantial number of missing cases [7]. Because of this omission, names have been suggested as a proxy for ethnicity, but this method yields a wide range of sensitivity (0.67–0.95) and specificity (0.8–1.0) [29]. Currently, many national audits do not include ethnicity and are exemplified by one of the largest and most important national audits of patients admitted with hip fractures, the National Hip Fracture Database [30]. The distribution of ethnic groups in our study is representative of the UK figures reported in 2016 and 2017 by SSNAP [3]. Importantly, the proportions of unknown ethnicity of 5.1% in our study and 6.1% in the UK national SSNAP data [3] reflect the poor documentation of ethnicity in the National Health Service (NHS) [12].
The proportion of patients with unknown ethnicity in this study was comparable to that of national data [3]. This particular group appears to be a common phenomenon in NHS medical records. It is uncertain whether this is because patients were voluntarily unwilling to disclose or unable to define their ethnicity or because of the lack documentation by healthcare professionals. Greater effort should be made to encourage both patients and health professionals to complete recording of the ethnicity of all patients in order to identify at-risk individuals. Mandatory documentation of ethnicity for all patients attending healthcare services is therefore a necessity. This particular group of unknown ethnicity is likely to represent a mix of ethnic backgrounds, as reflected in their intermediate characteristics and outcome values in relation to those of Caucasians and ethnic minorities.
Despite decades of health inequalities experienced by individuals from ethnic minority backgrounds, there has been little progress in reducing these gaps [31, 32]. The evidence for health inequality was ultimately divulged by the coronavirus (COVID-19) pandemic, revealing disproportionate numbers of severely affected cases amongst Asian and black populations. The aetiology is complex, involving socio-economic and biological factors. A recent review commissioned by the NHS Race and Health Observatory identified many areas of ethnic inequality were due to less accessibility to health services. Within maternity services, Asian and black women had higher rates of maternal mortality than white women, and intrauterine growth retardation were also more common, predisposing their offspring to greater risk of cardiometabolic disorders in later life. Culturally insensitive and poor communication has also been documented as an important contributing factor to health inequalities [32].
The lack of both research and policy focussing on health inequalities in ethnic minorities have frequently been highlighted [31,32,33]. Findings from our study, albeit from a relatively small sample, are likely to reflect a wider picture nationally. Large-scale high-quality research and national audits with comprehensive data collection and analyses are required. These should establish the areas of greatest need, such as socio-economic and lifestyle factors, as well as healthcare service factors, in order to direct policy makers and healthcare professionals to provide new strategies to reduce health inequality. This can only be achieved by redistribution of financial resources and healthcare services.
Strengths and limitations
The present study consisted of a cohort of patients recruited consecutively from one of the largest NHS regions in the UK. There were certain limitations to this study including the relatively small number of patients from an ethnic minority background, but the proportional representation of ethnic groups matched that of the rest of the stroke population in the UK [3]. Most of patients from ethnic minority group in this study were of South Asian background. It is possible that there may also be differences between ethnic minority groups (e.g., South Asians and Blacks) or even within each ethnic group, e.g., South Asians (Indians, Pakistanis, and Bangladeshis) or Blacks (Afro-Caribbeans and Africans) [34]. Generation of immigrants, cultural or religious practice may also contribute to health outcomes. However, these factors are beyond the scope of our study. Future studies, at national level, are necessary to gather comprehensive data on risk factors including healthy lifestyle promotion and primary prevention for cardiovascular disease such as glycaemic, lipid and blood pressure control, healthcare accessibility and monitoring for adherence to treatment and health outcomes in each specific ethnicity. The data were examined using multiple logistic regression technique, allowing robust adjustment for potential confounders including age, sex and co-morbidities and also pre-stroke disability (a marker of functional limitations). Additional adjustments for care-quality factors, such as swallow screen or review by a stroke physician within 72 h, did not change the results. This is likely to be due to equal standards of care received by all patients at this hospital. All data were collected in accordance with the national SSNAP protocol, using standardised scales such as NIHSS and mRS and other measures commonly used in national stroke surveys including hospital acquired infections in the first 7 days [3], and nutritional screen and MUST protocol [15].
In conclusion, patients from ethnic minorities with an acute stroke had 2- to fourfold greater likelihoods of stroke-related adverse outcomes and death. Further research is necessary to identify the aetiology of these ethnic differences to improve healthcare inequalities through strategic planning including preventative measures and intervention, including better diversity inclusion and routine documentation of ethnicity. Furthermore, clear guidelines should now be made available, advising mandatory record keeping of ethnicities for all patients on a routine basis.
References
Rex J, Singh G (2003) Multiculturalism and political integration in modern nation-states: thematic introduction. Int J Multicult Soc 5:3–19
Office for National Statistics. Change over time in admin-based ethnicity statistics, England: 2016 to 2020 Change over time in admin-based ethnicity statistics, England: 2016 to 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/articles/changeovertimeinadminbasedethnicitystatisticsengland2016to2020/2022-05-23 (Accessed 20 Sept 2022)
Royal College of Physicians. Clinical effectiveness and evaluation unit on behalf of the intercollegiate stroke working party. SSNAP April–July 2017. Public Report. https://www.strokeaudit.org/Documents/National/Clinical/AprJul2017/AprJul2017-PublicReport.aspx (Accessed 20 Sept 2022)
Nelson A (2002) Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc 94:666–668
Heath AF, Di Stasio V (2019) Racial discrimination in Britain, 1969–2017: a meta-analysis of field experiments on racial discrimination in the British labour market. The Br J Sociol 70:1774–1798
Han TS, Gabe J, Sharma P, Lean ME (2020) Life expectancy of white and non-white elite heavyweight boxers. J Racial Ethn Health Disparities 7:281–289
The King’s Fund. The health of people from ethnic minority groups in England. https://www.kingsfund.org.uk/publications/health-people-ethnic-minority-groups-england (Accessed 20 Sept 2022)
Mangalore R, Knapp M (2012) Income-related inequalities in common mental disorders among ethnic minorities in England. Soc Psychiatry Psychiatr Epidemiol 47:351–359
Bleich SN, Jarlenski MP, Bell CN, LaVeist TA (2012) Health inequalities: trends, progress, and policy. Annu Rev Public Health 33:7–40
US Department of Health and Human Services (2008) The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: recommendations for the framework and format of healthy people 2020. Section IV. Advisory Committee findings and recommendations. https://health.gov/sites/default/files/2021-11/Secretary%27s%20Advisory%20Committee%20Recommendations%20for%20HP2020%20Framework%20and%20Format.pdf. Accessed 20 Sept 2022
Department of Health. Tackling Health Inequalities: 10 Years On. A review of developments in tackling health inequalities in England over the last 10 years. http://www.bris.ac.uk/poverty/downloads/keyofficialdocuments/Tackling%20HE%2010%20years%20on.pdf (Accessed 20 Sept 2022)
Nuffield Trust. Flawed NHS records distort our view of ethnic health gaps, study shows. Published: 07/06/2021. https://www.nuffieldtrust.org.uk/news-item/flawed-nhs-records-distort-our-view-of-ethnic-health-gaps-study-shows (Accessed 20 Sept 2022)
Han TS, Gulli G, Affley B, Fluck D, Fry CH, Barrett C, Kakar P, Sharma S, Sharma P (2019) New evidence-based A1, A2, A3 alarm time zones for transferring thrombolysed patients to hyper-acute stroke units: faster is better. Neurol Sci 40:1659–1665
Han TS, Lean ME, Fluck D, Affley B, Gulli G, Patel T, Barrett C, Kakar P, Sharma S, Sharma P (2018) Impact of delay in early swallow screening on pneumonia, length of stay in hospital, disability and mortality in acute stroke patients. Eur J Clin Nutr 72:1548–1554
Kondrup JE, Allison SP, Elia M, Vellas B, Plauth M (2003) ESPEN guidelines for nutrition screening 2002. Clin Nutr 22:415–421
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, Van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Han TS, Gulli G, Fry CH, Affley B, Robin J, Fluck D, Kakar P, Sharma P (2022) Adverse consequences of immediate thrombolysis-related complications: a multi-centre registry-based cohort study of acute stroke. J Thromb Thrombolysis 53:218–227
Gulli G, Rutten-Jacobs LC, Kalra L, Rudd AG, Wolfe CD, Markus HS (2016) Differences in the distribution of stroke subtypes in a UK black stroke population - final results from the South London Ethnicity and Stroke Study. BMC Med 14:77
Marmot M (2020) Health equity in England: the Marmot review 10 years on. BMJ 25:368
www.Gov.UK. Socioeconomic status. https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/demographics/socioeconomic-status/latest#:~:text=Summary%20of%20Socioeconomic%20status%20Socio,Other%20ethnic%20group%20(1.0%25) (Accessed 20 Sept 2022)
UK Parliament. Insight: which ethnic groups are most affected by income inequality? Published Monday, 10 August, 2020. https://commonslibrary.parliament.uk/income-inequality-by-ethnic-group/ (Accessed 20 Sept 2022)
American Psychological Association. Ethnic and racial minorities & socioeconomic status. American Psychological Association. http://www.apa.org/pi/ses/resources/publications/factsheet-erm. aspx https://www.apa.org/pi/ses/resources/publications/minorities (Accessed 20 Sept 2022)
Li Y (2017) Persisting disadvantages: barriers to ethnic social mobility in the UK. Minority Report 1:7
Hayanga B, Stafford M, Bécares L (2021) Ethnic inequalities in healthcare use and care quality among people with multiple long-term health conditions living in the united kingdom: a systematic review and narrative synthesis. Int J Environ Res Public Health 18:12599
Lee C, Ayers SL, Kronenfeld JJ (2009) The association between perceived provider discrimination, health care utilization, and health status in racial and ethnic minorities. Ethn Dis 19:330–337
Hackett RA, Ronaldson A, Bhui K, Steptoe A, Jackson SE (2020) Racial discrimination and health: a prospective study of ethnic minorities in the United Kingdom. BMC Public Health 20:1–3
Nwokorocku SC, Neil B, Dlamini C, Osuchukwu VC (2022) A systematic review of the role of culture in the mental health service utilisation among ethnic minority groups in the United Kingdom. Global Mental Health 1–10. https://doi.org/10.1017/gmh.2022
Lindert J, Schouler-Ocak M, Heinz A, Priebe S (2008) Mental health, health care utilisation of migrants in Europe. Eur Psychiatry 23(S1):s114-120
Mateos P (2007) A review of name-based ethnicity classification methods and their potential in population studies. Popul Space Place 13:243–263
Fluck B, Yeong K, Lisk R, Watters H, Robin J, Fluck D, Fry CH, Han TS (2022) Changes in characteristics and outcomes of patients undergoing surgery for hip fractures following the initiation of orthogeriatric service: temporal trend analysis. Calcif Tissue Int 110:185–195
Graham H, Kelly MP (2004) Health inequalities: concepts, frameworks and policy. Health Development Agency, London
Kapadia D, Zhang J, Salway S, Nazroo J, Booth A, Villarroel-Williams N, Becares L, Esmail A (2022). Ethnic inequalities in healthcare: a rapid evidence review. Race and Health Observatory. https://www.nhsrho.org/wp-content/uploads/2022/02/RHO-Rapid-Review-Final-Report_v.7.pdf (Accessed 07 Nov 2022)
Sassi F, Le Grand J, Archard L (2001) Equity versus efficiency: a dilemma for the NHS: If the NHS is serious about equity it must offer guidance when principles conflict. BMJ 323:762–763
Kakar P, Gunarathne A, Lip GY (2006) Stroke: ethnic differences do exist. Expert Rev Neurother 6:1769–1771
Acknowledgements
The authors wish to thank patients and all those who were involved in the surveys.
Author information
Authors and Affiliations
Contributions
TSH and DF reviewed the topic related literature and performed the study concept and analysis design. GG, BA and PK performed the study coordination and data collection. TSH wrote the first draft, analysed, interpreted the data, and revised the manuscript. CHF edited the manuscript. GG, BA, JR, DF and PK checked and interpreted results and commented on the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Ethical approval
None.
Conflict of interest
The authors declared no competing interests.
Provenance and peer review
Not commissioned; externally peer reviewed.
Data sharing
No additional data are available.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fluck, D., Fry, C.H., Gulli, G. et al. Adverse stroke outcomes amongst UK ethnic minorities: a multi-centre registry-based cohort study of acute stroke. Neurol Sci 44, 2071–2080 (2023). https://doi.org/10.1007/s10072-023-06640-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06640-z