Abstract
Background
In the last years, laser interstitial thermal therapy (LITT) has started to be used also in neurosurgical setting. Its efficacy for intracranial pathologies, namely, tumors and epilepsy, has been widely demonstrated. However, the literature evidences about the use of LITT for spinal lesions are recent, and it is still a topic of discussion regarding its efficacy. Here, the authors sought to present a systematic review of the literature investigating the utility of LITT for spinal lesions.
Methods
Using PubMed, Scopus, and the Cochrane Library, the authors performed a systematic review of the literature focused on the use of spinal laser interstitial thermal therapy (sLITT). Included in the search were randomized controlled trials, cohort studies, and clinical series. Two independent reviewers conducted the study appraisal, data abstraction, and quality assessments of the studies.
Results
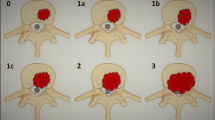
Out of the initial 134 studies, 6 met the inclusion criteria for the systematic review, resulting in a total of 206 patients. All the patients have been treated with sLITT for compressive spinal metastases. Most of the lesions were thoracic (88.8%). All the studies reported an effective local control of the disease with a reduction of epidural compression at 30 days. Complication rate was 12.6%, but most of them were transient conditions, and only 3.4% patients needed a revision surgery.
Conclusion
sLITT is safe and provides effective local control for epidural compression from metastases, particularly in the thoracic spine. The authors propose considering sLITT as an alternative to open surgery in selected patients with spinal metastases.

Similar content being viewed by others
References
Barzilai O, Fisher CG, Bilsky MH (2018) State of the art treatment of spinal metastatic disease. Neurosurgery 82(6):757–769. https://doi.org/10.1093/neuros/nyx567
Payer S, Mende KC, Westphal M, Eicker SO (2015) Intramedullary spinal cord metastases: an increasingly common diagnosis. Neurosurg Focus 39(2):E15. https://doi.org/10.3171/2015.5.FOCUS15149
Laufer I, Rubin DG, Lis E, Cox BW, Stubblefield MD, Yamada Y, Bilsky MH (2013) The NOMS framework: approach to the treatment of spinal metastatic tumors. Oncologist 18(6):744–51. https://doi.org/10.1634/theoncologist.2012-0293
Tatsui CE, Belsuzarri TA, Oro M, Rhines LD, Li J, Ghia AJ, Amini B, Espinoza H, Brown PD, Rao G (2016) Percutaneous surgery for treatment of epidural spinal cord compression and spinal instability: technical note. Neurosurg Focus 41(4):E2. https://doi.org/10.3171/2016.8.FOCUS16175
Pennington Z, Ahmed AK, Molina CA, Ehresman J, Laufer I, Sciubba DM (2018) Minimally invasive versus conventional spine surgery for vertebral metastases: a systematic review of the evidence. Ann Transl Med 6(6):103. https://doi.org/10.21037/atm.2018.01.28
Tatsui CE, Stafford RJ, Li J, Sellin JN, Amini B, Rao G, Suki D, Ghia AJ, Brown P, Lee SH, Cowles CE, Weinberg JS, Rhines LD (2015) Utilization of laser interstitial thermotherapy guided by real-time thermal MRI as an alternative to separation surgery in the management of spinal metastasis. J Neurosurg Spine 23(4):400–411. https://doi.org/10.3171/2015.2.SPINE141185
Missios S, Bekelis K, Barnett GH (2015) Renaissance of laser interstitial thermal ablation. Neurosurg Focus 38(3):E13. https://doi.org/10.3171/2014.12.FOCUS14762
Bastos DCA, Vega RA, Traylor JI, Ghia AJ, Li J, Oro M, Bishop AJ, Yeboa DN, Amini B, Kumar VA, Rao G, Rhines LD, Tatsui CE (2020) Spinal laser interstitial thermal therapy: single-center experience and outcomes in the first 120 cases. J Neurosurg Spine 1–10. https://doi.org/10.3171/2020.7.SPINE20661
Bown SG (1983) Phototherapy in tumors. World J Surg 7(6):700–709. https://doi.org/10.1007/BF01655209
Schwarzmaier HJ, Eickmeyer F, von Tempelhoff W, Fiedler VU, Niehoff H, Ulrich SD, Yang Q, Ulrich F (2006) MR-guided laser-induced interstitial thermotherapy of recurrent glioblastoma multiforme: preliminary results in 16 patients. Eur J Radiol 59(2):208–215. https://doi.org/10.1016/j.ejrad.2006.05.010
Kang JY, Wu C, Tracy J, Lorenzo M, Evans J, Nei M, Skidmore C, Mintzer S, Sharan AD, Sperling MR (2016) Laser interstitial thermal therapy for medically intractable mesial temporal lobe epilepsy. Epilepsia 57(2):325–334. https://doi.org/10.1111/epi.13284
Silva D, Sharma M, Juthani R, Meola A, Barnett GH (2017) Magnetic resonance thermometry and laser interstitial thermal therapy for brain tumors. Neurosurg Clin N Am 28(4):525–533. https://doi.org/10.1016/j.nec.2017.05.015
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 21(339):b2700. https://doi.org/10.1136/bmj.b2700
de Almeida Bastos DC, Everson RG, de Oliveira Santos BF, Habib A, Vega RA, Oro M, Rao G, Li J, Ghia AJ, Bishop AJ, Yeboa DN, Amini B, Rhines LD, Tatsui CE (2020) A comparison of spinal laser interstitial thermotherapy with open surgery for metastatic thoracic epidural spinal cord compression. J Neurosurg Spine 1–9. https://doi.org/10.3171/2019.10.SPINE19998
Moses ZB, Lee TC, Huang KT, Guenette JP, Chi JH (2020) MRI-guided cryoablation for metastatic spine disease: intermediate-term clinical outcomes in 14 consecutive patients. J Neurosurg Spine 1–6. https://doi.org/10.3171/2019.11.SPINE19808
Tatsui CE, Nascimento CNG, Suki D, Amini B, Li J, Ghia AJ, Thomas JG, Stafford RJ, Rhines LD, Cata JP, Kumar AJ, Rao G (2017) Image guidance based on MRI for spinal interstitial laser thermotherapy: technical aspects and accuracy. J Neurosurg Spine 26(5):605–612. https://doi.org/10.3171/2016.9.SPINE16475
Tokuhashi Y, Uei H, Oshima M, Ajiro Y (2014) Scoring system for prediction of metastatic spine tumor prognosis. World J Orthop 5(3):262–271. https://doi.org/10.5312/wjo.v5.i3.262
Akeyson EW, McCutcheon IE (1996) Single-stage posterior vertebrectomy and replacement combined with posterior instrumentation for spinal metastasis. J Neurosurg 85(2):211–220. https://doi.org/10.3171/jns.1996.85.2.0211
Young RF, Post EM, King GA (1980) Treatment of spinal epidural metastases. Randomized prospective comparison of laminectomy and radiotherapy. J Neurosurg 53(6):741–8. https://doi.org/10.3171/jns.1980.53.6.0741
Molina CA, Gokaslan ZL, Sciubba DM (2012) Diagnosis and management of metastatic cervical spine tumors. Orthop Clin N Am 43(1):75–87. https://doi.org/10.1016/j.ocl.2011.08.004 (viii-ix)
Vogl TJ, Dommermuth A, Heinle B, Nour-Eldin NE, Lehnert T, Eichler K, Zangos S, Bechstein WO, Naguib NN (2014) Colorectal cancer liver metastases: long-term survival and progression-free survival after thermal ablation using magnetic resonance-guided laser-induced interstitial thermotherapy in 594 patients: analysis of prognostic factors. Invest Radiol 49(1):48–56. https://doi.org/10.1097/RLI.0b013e3182a6094e
Ahrar K, Stafford RJ (2011) Magnetic resonance imaging-guided laser ablation of bone tumors. Tech Vasc Interv Radiol 14(3):177–182. https://doi.org/10.1053/j.tvir.2011.02.010
McNichols RJ, Gowda A, Kangasniemi M, Bankson JA, Price RE, Hazle JD (2004) MR thermometry-based feedback control of laser interstitial thermal therapy at 980 nm. Lasers Surg Med 34(1):48–55. https://doi.org/10.1002/lsm.10243
Gilbert RW, Kim JH, Posner JB (1978) Epidural spinal cord compression from metastatic tumor: diagnosis and treatment. Ann Neurol 3(1):40–51. https://doi.org/10.1002/ana.410030107
Maranzano E, Latini P, Checcaglini F, Ricci S, Panizza BM, Aristei C, Perrucci E, Beneventi S, Corgna E, Tonato M (1991) Radiation therapy in metastatic spinal cord compression. A prospective analysis of 105 consecutive patients. Cancer 67(5):1311–1317. https://doi.org/10.1002/1097-0142(19910301)67:5<1311::aid-cncr2820670507>3.0.co;2-r
Yamada Y, Bilsky MH, Lovelock DM, Venkatraman ES, Toner S, Johnson J, Zatcky J, Zelefsky MJ, Fuks Z (2008) High-dose, single-fraction image-guided intensity-modulated radiotherapy for metastatic spinal lesions. Int J Radiat Oncol Biol Phys 71(2):484–490. https://doi.org/10.1016/j.ijrobp.2007.11.046
Sahgal A, Bilsky M, Chang EL, Ma L, Yamada Y, Rhines LD, Létourneau D, Foote M, Yu E, Larson DA, Fehlings MG (2011) Stereotactic body radiotherapy for spinal metastases: current status, with a focus on its application in the postoperative patient. J Neurosurg Spine 14(2):151–166. https://doi.org/10.3171/2010.9.SPINE091005
Nguyen QN, Shiu AS, Rhines LD, Wang H, Allen PK, Wang XS, Chang EL (2010) Management of spinal metastases from renal cell carcinoma using stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 76(4):1185–1192. https://doi.org/10.1016/j.ijrobp.2009.03.062
Clohisy DR, Perkins SL, Ramnaraine ML (2000) Review of cellular mechanisms of tumor osteolysis. Clin Orthop Relat Res 373:104–114. https://doi.org/10.1097/00003086-200004000-00013
Sacino M, Huang SS, Alexander H, Fayed I, Keating RF, Oluigbo CO (2020) An initial cost-effectiveness analysis of magnetic resonance-guided laser interstitial thermal therapy in pediatric epilepsy surgery. Pediatr Neurosurg 55(3):141–148. https://doi.org/10.1159/000509329
Hong CS, Kundishora AJ, Elsamadicy AA, Chiang VL (2020) Laser interstitial thermal therapy in neuro-oncology applications. Surg Neurol Int 8(11):231. https://doi.org/10.25259/SNI_496_2019
Zaed I, Bossi B, Ganau M, Tinterri B, Giordano M, Chibbaro S (2022) Current state of benefits of enhanced recovery after surgery (ERAS) in spinal surgeries: a systematic review of the literature. Neurochirurgie 68(1):61–68. https://doi.org/10.1016/j.neuchi.2021.04.007
Srinivasan ES, Grabowski MM, Nahed BV, Barnett GH, Fecci PE (2021) Laser interstitial thermal therapy for brain metastases. Neurooncol Adv 3(Suppl 5):v16–v25. https://doi.org/10.1093/noajnl/vdab128
Srinivasan ES, Sankey EW, Grabowski MM, Chongsathidkiet P, Fecci PE (2020) The intersection between immunotherapy and laser interstitial thermal therapy: a multipronged future of neuro-oncology. Int J Hyperthermia 37(2):27–34. https://doi.org/10.1080/02656736.2020.1746413
University of Florida (2021) Recurrent brain metastasis immune effects and response to laser interstitial thermotherapy (LITT) and pembrolizumab in combination (TORCH). clinicaltrials.gov. https://clinicaltrials.gov/ct2/show/NCT04187872. Accessed July 29, 2021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None.
Informed consent
No consent was needed for this type of study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cardia, A., Cannizzaro, D., Stefini, R. et al. The efficacy of laser interstitial thermal therapy in the management of spinal metastases: a systematic review of the literature. Neurol Sci 44, 519–528 (2023). https://doi.org/10.1007/s10072-022-06432-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06432-x