Abstract
Background
The prevalence of olfactory impairment in patients with Parkinson’s disease (PD) is 50–90%, and therefore, olfactory dysfunction is one of the most prevalent non-motor symptoms (NMSs) in patients with PD. Numerous studies have evaluated the association between motor and non-motor symptoms and olfactory dysfunction in PD.
Aim
In this study, we investigated the relationship between olfactory dysfunction, which is measured using the UPSIT test, with other motor and non-motor symptoms separately in three motor subtypes of PD, including tremor dominant (TD), postural instability and gait difficulty (PIGD), and indeterminate and healthy subjects.
Methods
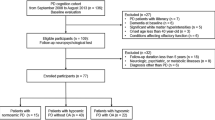
We recruited 487 early-stage PD patients (43 PIGD, 406 TD, and 38 indeterminate) and healthy controls (HCs) (n = 197) from the Parkinson Progression Markers Initiative (PPMI). All participants completed motor and non-motor tests at baseline visit and after 4 years of follow-up. Subjects underwent common PD scaling tests.
Results
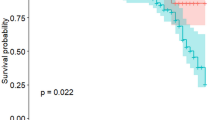
Olfactory dysfunction was significantly correlated with declined motor functions only in the TD subtype. Also, significant correlations were noticed between olfactory dysfunction and speed-attention processing and executive function in the HCs as well. Finally, no significant or meaningful association was observed in the PIGD and indeterminate subtype. Anosmia and hyposmia subjects in the TD group had the worse motor and non-motor scores compared to normosmia subjects after 4 years.
Conclusion
Olfactory dysfunction was significantly correlated with declined motor functions in the TD subtype. This is indicating that olfactory dysfunction may be an early motor and non-motor biomarker only in the TD subtype. However, it is possible that the involvement of olfactory function in other subtypes is not strong enough to make it a useful marker of diseases progression.


Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available upon request with no restriction.
References
Trentin S, Fraiman de Oliveira BS, Ferreira Felloni Borges Y, de Mello Rieder CR (2021) Systematic review and meta-analysis of Sniffin Sticks Test performance in Parkinson's disease patients in different countries. Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-021-06970-8
Dorsey ER, Sherer T, Okun MS, Bloem BR (2018) The emerging evidence of the Parkinson pandemic. J Parkinsons Dis 8(s1):S3–S8. https://doi.org/10.3233/JPD-181474
Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, Schrag A-E, Lang AE (2017) Parkinson disease. Nature Reviews Disease Primers 2017 3:1 3 (1):1–21 https://doi.org/10.1038/nrdp.2017.13
Eek T, Larsson M, Dizdar N (2021) Odor Recognition memory in Parkinson’s disease: a systematic review. Frontiers in Aging Neuroscience 13:625171–625171. https://doi.org/10.3389/FNAGI.2021.625171
Fullard ME, Morley JF, Duda JE (2017) Olfactory dysfunction as an early biomarker in Parkinson’s disease. Neurosci Bull 33(5):515–515. https://doi.org/10.1007/S12264-017-0170-X
Rietdijk CD, Perez-Pardo P, Garssen J, van Wezel RJA, Kraneveld AD (2017) Exploring Braak’s hypothesis of Parkinson’s disease. Front in Neurol 8:1–1. https://doi.org/10.3389/FNEUR.2017.00037
Morley JF, Cohen A, Silveira-Moriyama L, Lees AJ, Williams DR, Katzenschlager R, Hawkes C, Shtraks JP, Weintraub D, Doty RL, Duda JE (2018) Optimizing olfactory testing for the diagnosis of Parkinson’s disease: item analysis of the university of Pennsylvania smell identification test. npj Parkinson's Disease 2018 4:1 4 (1):1–7 https://doi.org/10.1038/s41531-017-0039-8
Wang J, You H, Liu JF, Ni DF, Zhang ZX, Guan J (2011) Association of olfactory bulb volume and olfactory sulcus depth with olfactory function in patients with Parkinson disease. Am J Neuroradiol 32(4):677–681. https://doi.org/10.3174/AJNR.A2350
Yoo HS, Chung SJ, Lee YH, Ye BS, Sohn YH, Lee PH (2020) Association between olfactory deficit and motor and cognitive function in parkinsons disease. J of Mov Disord 13(2):133–141. https://doi.org/10.14802/JMD.19082
Rossi M, Escobar AM, Bril A, Vernetti PM, Palo JI, Cerquetti D, Merello M (2016) Motor features in Parkinson’s disease with normal olfactory function Movement disorders. off j of the Mov Disord Soc 31(9):1414–1417
Qian E, Huang Y (2019) Subtyping of Parkinson’s disease - where are we up to. Aging Dis 10(5):1130–1139. https://doi.org/10.14336/AD.2019.0112
Jankovic J, McDermott M, Carter J, Gauthier S, Goetz C, Golbe L, Huber S, Koller W, Olanow C, Shoulson I, Stern M, Tanner C, Weiner W, Group PS (1990) Variable expression of Parkinsons disease. Neurol 40(10):1529–1529. https://doi.org/10.1212/WNL.40.10.1529
Huang X, Ng SYE, Chia NSY, Setiawan F, Tay KY, Au WL, Tan EK, Tan LCS (2019) Non-motor symptoms in early Parkinson’s disease with different motor subtypes and their associations with quality of life. Eur J Neurol 26(3):400–406. https://doi.org/10.1111/ENE.13803
Paulus W, Jellinger K (1991) The neuropathologic basis of different clinical subgroups of Parkinson’s disease. J Neuropathol Exp Neurol 50(6):743–755. https://doi.org/10.1097/00005072-199111000-00006
Kang GA, Bronstein JM, Masterman DL, Redelings M, Crum JA, Ritz B (2005) Clinical characteristics in early Parkinson’s disease in a central California population-based study. Mov Disord 20(9):1133–1142. https://doi.org/10.1002/MDS.20513
Herman T, Weiss A, Brozgol M, Giladi N, Hausdorff JM (2014) Gait and balance in Parkinson’s disease subtypes: objective measures and classification considerations. Journal of Neurology 2014 261:12 261 (12):2401–2410. https://doi.org/10.1007/S00415-014-7513-6
Herman T, Weiss A, Brozgol M, Wilf-Yarkoni A, Giladi N, Hausdorff JM (2014) Cognitive function and other non-motor features in non-demented Parkinson’s disease motor subtypes. Journal of Neural Transmission 2014 122:8 122 (8):1115–1124 https://doi.org/10.1007/S00702-014-1349-1
Xu C, Zhuang P, Hallett M, Zhang Y, Li J, Li Y (2018) Parkinson's Disease Motor Subtypes Show Different Responses to Long-Term Subthalamic Nucleus Stimulation. Front Hum Neurosci 12:365. https://doi.org/10.3389/fnhum.2018.00365
Rezvanian S, Lockhart T, Frames C, Soangra R, Lieberman A (2018) Motor subtypes of Parkinson's disease can be identified by frequency component of postural stability. Sensors (Basel) 18(4):1102. https://doi.org/10.3390/s18041102
Rudzińska M, Marona M, Bukowczan S, Banaszkiewicz K, Mirek E, Szczudlik A (2007) Falls in different types of Parkinson’s disease. Neurol Neurochir Pol 41(5):395–403
Choi S-M, Kim BC, Cho B-H, Kang KW, Choi K-H, Kim J-T, Lee S-H, Park M-S, Kim M-K, Cho K-H (2018) Comparison of two motor subtype classifications in de novo Parkinson’s disease. Parkinsonism Relat Disord 54:74–78. https://doi.org/10.1016/J.PARKRELDIS.2018.04.021
Stebbins GT, Goetz CG, Burn DJ, Jankovic J, Khoo TK, Tilley BC (2013) How to identify tremor dominant and postural instability/gait difficulty groups with the movement disorder society unified Parkinson’s disease rating scale: comparison with the unified Parkinson’s disease rating scale. Mov disord off j of the Mov Disord Soc 28(5):668–670. https://doi.org/10.1002/mds.25383
Masala C, Solla P, Liscia A, Defazio G, Saba L, Cannas A, Cavazzana A, Hummel T, Haehner A (2018) Correlation among olfactory function, motors’ symptoms, cognitive impairment, apathy, and fatigue in patients with Parkinson’s disease. J Neurol 265(8):1764–1771. https://doi.org/10.1007/s00415-018-8913-9
He R, Zhao Y, He Y, Zhou Y, Yang J, Zhou X, Zhu L, Zhou X, Liu Z, Xu Q, Sun Q, Tan J, Yan X, Tang B, Guo J (2020) Olfactory dysfunction predicts disease progression in Parkinson’s disease: a longitudinal study. Front Neurosci 14:569777. https://doi.org/10.3389/fnins.2020.569777
Braak H, Del Tredici K, Rüb U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24(2):197–211. https://doi.org/10.1016/s0197-4580(02)00065-9
Li W, Lao-Kaim NP, Roussakis AA, Martín-Bastida A, Valle-Guzman N, Paul G, Loane C, Widner H, Politis M, Foltynie T, Barker RA, Piccini P (2018) (11) C-PE2I and (18) F-Dopa PET for assessing progression rate in Parkinson’s: a longitudinal study. Mov Disord 33(1):117–127. https://doi.org/10.1002/mds.27183
Roos DS, Twisk JWR, Raijmakers P, Doty RL, Berendse HW (2019) Hyposmia as a marker of (non-)motor disease severity in Parkinson’s disease. J Neural Transm (Vienna) 126(11):1471–1478. https://doi.org/10.1007/s00702-019-02074-0
Elhassanien MEM, Bahnasy WS, El-Heneedy YAE, Kishk AM, Tomoum MO, Ramadan KM, Allah Ragab OA (2021) Olfactory dysfunction in essential tremor versus tremor dominant Parkinson disease. Clin Neurol Neurosurg 200:106352. https://doi.org/10.1016/j.clineuro.2020.106352
Ondo WG, Lai D (2005) Olfaction testing in patients with tremor-dominant Parkinson’s disease: is this a distinct condition? Mov Disord 20(4):471–475. https://doi.org/10.1002/mds.20365
Kang P, Kloke J, Jain S (2012) Olfactory dysfunction and parasympathetic dysautonomia in Parkinson’s disease. Clin Auton Res 22(4):161–166. https://doi.org/10.1007/s10286-012-0158-6
Zhao Y, He Y, He R, Zhou Y, Pan H, Zhou X, Zhu L, Zhou X, Liu Z, Xu Q, Sun Q, Tan J, Yan X, Tang B, Guo J (2020) The discriminative power of different olfactory domains in Parkinson’s disease. Front Neurol 11:420–420. https://doi.org/10.3389/fneur.2020.00420
Healy DG, Falchi M, O’Sullivan SS, Bonifati V, Durr A, Bressman S, Brice A, Aasly J, Zabetian CP, Goldwurm S, Ferreira JJ, Tolosa E, Kay DM, Klein C, Williams DR, Marras C, Lang AE, Wszolek ZK, Berciano J, Schapira AH, Lynch T, Bhatia KP, Gasser T, Lees AJ, Wood NW (2008) Phenotype, genotype, and worldwide genetic penetrance of LRRK2-associated Parkinson’s disease: a case-control study. The Lancet Neurol 7(7):583–590. https://doi.org/10.1016/s1474-4422(08)70117-0
Ferreira JJ, Guedes LC, Rosa MM, Coelho M, van Doeselaar M, Schweiger D, Di Fonzo A, Oostra BA, Sampaio C, Bonifati V (2007) High prevalence of LRRK2 mutations in familial and sporadic Parkinson’s disease in Portugal. Mov Disord 22(8):1194–1201. https://doi.org/10.1002/mds.21525
Latourelle JC, Sun M, Lew MF, Suchowersky O, Klein C, Golbe LI, Mark MH, Growdon JH, Wooten GF, Watts RL, Guttman M, Racette BA, Perlmutter JS, Ahmed A, Shill HA, Singer C, Goldwurm S, Pezzoli G, Zini M, Saint-Hilaire MH, Hendricks AE, Williamson S, Nagle MW, Wilk JB, Massood T, Huskey KW, Laramie JM, DeStefano AL, Baker KB, Itin I, Litvan I, Nicholson G, Corbett A, Nance M, Drasby E, Isaacson S, Burn DJ, Chinnery PF, Pramstaller PP, Al-hinti J, Moller AT, Ostergaard K, Sherman SJ, Roxburgh R, Snow B, Slevin JT, Cambi F, Gusella JF, Myers RH (2008) The Gly2019Ser mutation in LRRK2 is not fully penetrant in familial Parkinson’s disease: the GenePD study. BMC Med 6:32. https://doi.org/10.1186/1741-7015-6-32
Khan NL, Jain S, Lynch JM, Pavese N, Abou-Sleiman P, Holton JL, Healy DG, Gilks WP, Sweeney MG, Ganguly M, Gibbons V, Gandhi S, Vaughan J, Eunson LH, Katzenschlager R, Gayton J, Lennox G, Revesz T, Nicholl D, Bhatia KP, Quinn N, Brooks D, Lees AJ, Davis MB, Piccini P, Singleton AB, Wood NW (2005) Mutations in the gene LRRK2 encoding dardarin (PARK8) cause familial Parkinson’s disease: clinical, pathological, olfactory and functional imaging and genetic data. Brain : a j of neurol 128(Pt 12):2786–2796. https://doi.org/10.1093/brain/awh667
Goker-Alpan O, Lopez G, Vithayathil J, Davis J, Hallett M, Sidransky E (2008) The spectrum of parkinsonian manifestations associated with glucocerebrosidase mutations. Arch Neurol 65(10):1353–1357. https://doi.org/10.1001/archneur.65.10.1353
Saunders-Pullman R, Hagenah J, Dhawan V, Stanley K, Pastores G, Sathe S, Tagliati M, Condefer K, Palmese C, Brüggemann N, Klein C, Roe A, Kornreich R, Ozelius L, Bressman S (2010) Gaucher disease ascertained through a Parkinson’s center: imaging and clinical characterization. Mov Disord 25(10):1364–1372. https://doi.org/10.1002/mds.23046
Saunders-Pullman R, Stanley K, Wang C, San Luciano M, Shanker V, Hunt A, Severt L, Raymond D, Ozelius LJ, Lipton RB, Bressman SB (2011) Olfactory dysfunction in LRRK2 G2019S mutation carriers. Neurol 77(4):319–324. https://doi.org/10.1212/WNL.0b013e318227041c
von Coelln R, Shulman LM (2016) Clinical subtypes and genetic heterogeneity: of lumping and splitting in Parkinson disease. Curr Opin Neurol 29(6):727–734. https://doi.org/10.1097/wco.0000000000000384
Lee DH, Oh JS, Ham JH, Lee JJ, Lee I, Lee PH, Kim JS, Sohn YH (2015) Is normosmic Parkinson disease a unique clinical phenotype? Neurol 85(15):1270–1275. https://doi.org/10.1212/wnl.0000000000001999
Rossi M, Escobar AM, Bril A, Millar Vernetti P, De Palo JI, Cerquetti D, Merello M (2016) Motor features in Parkinson’s disease with normal olfactory function. Mov Disord 31(9):1414–1417. https://doi.org/10.1002/mds.26687
Fullard ME, Tran B, Xie SX, Toledo JB, Scordia C, Linder C, Purri R, Weintraub D, Duda JE, Chahine LM, Morley JF (2016) Olfactory impairment predicts cognitive decline in early Parkinson’s disease. Parkinsonism Relat Disord 25:45–51. https://doi.org/10.1016/j.parkreldis.2016.02.013
Soudry Y, Lemogne C, Malinvaud D, Consoli SM, Bonfils P (2011) Olfactory system and emotion: common substrates. Eur Ann Otorhinolaryngol Head Neck Dis 128(1):18–23. https://doi.org/10.1016/j.anorl.2010.09.007
Hong JY, Sunwoo MK, Ham JH, Lee JJ, Lee PH, Sohn YH (2015) Apathy and olfactory dysfunction in early Parkinson’s disease. J Mov Disord 8(1):21–25. https://doi.org/10.14802/jmd.14029
Morley JF, Weintraub D, Mamikonyan E, Moberg PJ, Siderowf AD, Duda JE (2011) Olfactory dysfunction is associated with neuropsychiatric manifestations in Parkinson’s disease. Mov Disord 26(11):2051–2057. https://doi.org/10.1002/mds.23792
Acknowledgements
Parkinson’s Progression Markers Initiative (PPMI) database (www.ppmi-info.org/data) was our primary source of data in this research. For up-to-date information on the study, see www.ppmiinfo.org. We gratefully thank all sponsors and funders of PPMI including the Michael J. Fox Foundation for Parkinson’s Research, AbbVie, Avid Radiopharmaceuticals, Biogen, Bristol-Myers Squibb, Covance, GE Healthcare, Genentech, GlaxoSmithKline (GSK), Eli Lilly and Company, Lundbeck, Merck, Meso Scale Discovery (MSD), Pfizer, Piramal Imaging, Roche, Servier, and UCB (www.ppmi-info.org/fundingpartners).
Author information
Authors and Affiliations
Contributions
FN and KP designed the study, analyzed the data, and wrote the paper; FN, EKH, and KP collected the data, analyzed and interpreted the data, and wrote the draft version of the manuscript. The manuscript was revised and approved by all authors.
Corresponding author
Ethics declarations
Ethical approval
Since the data in this paper were obtained from the PPMI database (ppmi.loni.usc.edu), it does not include any research involving human or animal subjects.
Consent for publication
This manuscript has been approved for publication by all authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nabizadeh, F., Pirahesh, K. & Khalili, E. Olfactory dysfunction is associated with motor function only in tremor-dominant Parkinson’s disease. Neurol Sci 43, 4193–4201 (2022). https://doi.org/10.1007/s10072-022-05952-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-05952-w