Abstract
Objective
To summarize the clinical, serological, and radiological characteristics of anti-synthetase syndrome (ASS) patients with different anti-aminoacyl-tRNA synthase antibody.
Methods
Retrospective analysis was performed based on the clinical data of 88 patients diagnosed with ASS in Tianjin Medical University General Hospital from January 2015 to December 2020. The clinical data included general conditions, serological indexes, high-resolution CT (HRCT) characteristics, and pulmonary function manifestations.
Results
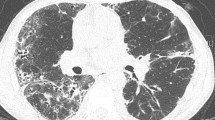
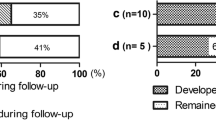
Among the 88 patients, there were 17 males and 71 females. The anti-synthetase antibodies included anti-Jo-1 (n = 42), anti-PL-7 (n = 14), anti-PL-12 (n = 9), anti-EJ (n = 20), and anti-OJ (n = 3) antibodies. The most common clinical manifestations of ASS patients were interstitial lung disease (ILD) (90%, 79/88), followed by myositis (79.5%, 70/88), arthritis (50%, 44/88), and rash (50%, 44/88). The frequency of arthritis in the anti-Jo-1 antibody–positive group was higher than that of the anti-PL-7 and anti-EJ antibody groups (P = 0.004, P = 0.002, respectively). The frequency of Gottron’s sign in the anti-PL-7 antibody positive group was higher than that of the anti-Jo-1 and anti-PL-12 antibody–positive groups (P = 0.006, P = 0.04). Isolated arthritis was the most frequent initial symptoms in anti-Jo-1 antibody–positive group (47.6%, 20/42), while isolated ILD was most frequent in patients with anti-EJ antibody (50%, 10/20), and isolated myositis in patients carrying anti-OJ (66.7%, 2/3). There were only 32 cases (36.4%) with the typical clinical triad (myositis, arthritis, ILD). In our cohort, 79 patients (90%) were complicated with ILD. Meanwhile, 7 out of 79 cases were classified into rapid progressive group with 6 cases (85.7%) carrying anti-Ro-52 antibody. The probability of reticular and honeycombing shadow in HRCT of patients with anti-EJ antibody positive was higher than that of other groups (P < 0.05).
Conclusion
ILD, myositis, and arthritis were the most common clinical manifestations in patients with ASS. Different antibody-positive patients have different initial symptoms. Patients with isolated arthritis, myositis, and ILD should be vigilant of ASS. The complication of anti-Ro-52 antibody in ASS patients was associated with rapidly progressive pulmonary interstitial disease. Patients with positive anti-EJ antibodies tend to have ILD as the first symptom, and with high occurrence of ILD, the HRCT showed more serious patterns, suggesting the correlation between anti-EJ antibodies and ILD.
Key Points • Analyzing specific clinical manifestations in ASS patients with different ARS antibodies can raise awareness of the disease and reduce misdiagnosis. • Anti-EJ antibodies were correlated with ILD. • Anti-Ro-52 antibodies may correlate with RP-ILD in ASS patients. |
Similar content being viewed by others
Data availability
The datasets used and analysed in the present research are available from the corresponding author on reasonable request.
References
Mahler M, Miller F, Fritzler M (2014) Idiopathic inflammatory myopathies and the anti-synthetase syndrome: a comprehensive review [J]. Autoimmunity Rev 13(0):367–371
Imbert-Masseau A, Hamidou M, Agard C et al (2003) Antisynthetase syndrome [J]. Joint Bone Spine 70(3):161–168
Satoh M, Tanaka S, Ceribelli A et al (2017) A comprehensive overview on myositis-specific antibodies: new and old biomarkers in idiopathic inflammatory myopathy [J]. Clin Rev Allergy Immunol 52(1):11–19
McHugh N, Tansley S (2018) Autoantibodies in myositis [J]. Nat Rev Rheumatol 14(5):290–302
Witt L, Curran J, Strek M (2016) The diagnosis and treatment of antisynthetase syndrome [J]. Clin Pulm Med 23(5):218–226
Travis W, Costabel U, Hansell D et al (2013) An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias [J]. Am J Respir Crit Care Med 188(6):733–748
Gono T, Kawaguchi Y, Satoh T et al (2010) Clinical manifestation and prognostic factor in anti-melanoma differentiation-associated gene 5 antibody-associated interstitial lung disease as a complication of dermatomyositis [J]. Rheumatology (Oxford) 49(9):1713–1719
Zhan X, Yan W, Wang Y et al (2021) Clinical features of anti-synthetase syndrome associated interstitial lung disease: a retrospective cohort in China [J]. BMC Pulm Med 21(1):57–61
Shi J, Li S, Yang H et al (2017) Clinical profiles and prognosis of patients with distinct antisynthetase autoantibodies [J]. J Rheumatol 44(7):1051–1057
La Corte R, Lo Mo naco A, Locaputo A et al (2006) In patients with antisynthetase syndrome the occurrence of anti-Ro/SSA antibodies causes a more severe interstitial lung disease [J]. Autoimmunity 39(3):249–253
Váncsa A, Csípo I, Németh J et al (2009) Characteristics of interstitial lung disease in SS-A positive/Jo-1 positive inflammatory myopathy patients [J]. Rheumatol Int 29(9):989–994
Cavagna L, Trallero-Araguás E, Meloni F et al (2019) Influence of antisynthetase antibodies specificities on antisynthetase syndrome clinical spectrum time course [J]. J Clin Med 8(11)
Aggarwal R, Cassidy E, Fertig N et al (2014) Patients with non-Jo-1 anti-tRNA-synthetase autoantibodies have worse survival than Jo-1 positive patients [J]. Ann Rheum Dis 73(1):227–232
Kumar R, Jha S, Dhooria A et al (2021) Anti-Jo-1 syndrome often misdiagnosed as rheumatoid arthritis (for many years): a single-center experience [J]. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis 27(4):150–155
Andersson H, Aaløkken T, Günther A et al (2016) Pulmonary involvement in the antisynthetase syndrome: a comparative cross-sectional Study [J]. J Rheumatol 43(6):1107–1113
Johnson C, Connors G, Oaks J et al (2014) Clinical and pathologic differences in interstitial lung disease based on antisynthetase antibody type [J]. Respir Med 108(10):1542–1548
Gasparotto M, Gatto M, Saccon F et al (2019) Pulmonary involvement in antisynthetase syndrome [J]. Curr Opin Rheumatol 31(6):603–610
Chen F, Zuo Y, Li S et al (2019) Clinical characteristics of dermatomyositis patients with isolated anti-Ro-52 antibody associated rapid progressive interstitial lung disease: data from the largest single Chinese center [J]. Respir Med 155:127–132
Pinal-Fernandez I, Casal-Dominguez M, Huapaya J et al (2017) A longitudinal cohort study of the anti-synthetase syndrome: increased severity of interstitial lung disease in black patients and patients with anti-PL7 and anti-PL12 autoantibodies [J]. Rheumatology (Oxford) 56(6):999–1007
Zhang Y, Ge Y, Yang H et al (2020) Clinical features and outcomes of the patients with anti-glycyl tRNA synthetase syndrome [J]. Clin Rheumatol 39(8):2417–2419
Marie I, Hatron P, Dominique S et al (2012) Short-term and long-term outcome of anti-Jo1-positive patients with anti-Ro52 antibody [J]. Semin Arthritis Rheum 41(6):890–899
Shao C, Sun Y, Huang H et al (2021) Myositis specific antibodies are associated with isolated anti-Ro-52 associated interstitial lung disease [J]. Rheumatology (Oxford, England) 61(3):1083–1091
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
Ethics approval was waived by the IRB (Institutional Review Board) of Tianjin Medical University General Hospital.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, R., Zhao, Y., Qi, F. et al. Analysis of the clinical features of antisynthetase syndrome: a retrospective cohort study in China. Clin Rheumatol 42, 703–709 (2023). https://doi.org/10.1007/s10067-022-06404-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06404-8