Abstract
Objectives
Factors associated with disease activity of axial spondyloarthritis (axSpA) and switching of biologic disease-modifying anti-rheumatic drugs have not been clearly defined. We aimed to evaluate clinical characteristics of patients with axSpA, factors related to remission in treat to target era and predictive factors for biologic disease-modifying anti-rheumatic drug switching.
Method
A multicenter, observational cross-sectional study was performed between February 2019 and August 2019. We included all consecutive patients ≥ 18 years with axSpA. Demographic and clinical variables were prospectively recorded. Clinical tools included Ankylosing Spondylitis Disease Activity Score with C-reactive protein (ASDAS-CRP), Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath Ankylosing Spondylitis Metrology Index (BASMI), and Maastricht Ankylosing Spondylitis Enthesitis Score (MASES).
Results
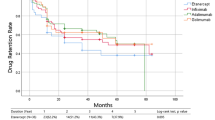
There were 969 patients with a mean age of 43.4 ± 10.8 years. There were 143 patients (14.8%) with remission and 223 (23.1%) patients with low disease activity. Male sex (p = 0.021), positive family history (p = 0.036), and human leukocyte antigen-B27 (p = 0.011) were predictors of remission by ASDAS-CRP. There were 654 patients (67.5%) who did not switch to another drug. The highest BASMI and MASES scores were calculated in patients with very high disease activity (p < 0.05). In patients with drug switching, the disease duration was significantly higher (p < 0.001) and the age at diagnosis was significantly lower (p = 0.016). There were significantly more patients with uveitis and higher scores of MASES and BASMI in patients who switch to another biologic disease-modifying anti-rheumatic drugs (p = 0.003, p = 0.009, and p = 0.004, respectively).
Conclusions
In patients with axSpA, male sex, younger age, and HLA-B27 positivity are associated with remission, while longer disease duration and accompanied uveitis appear to be related with drug switching.
Clinical trial registration number and date
NCT04139954/25.10.2019.
Key Points • Achievement of remission and/or low disease activity rates in patients with axSpA were assessed in a big registry from a real-life data. • Predictive factors for switching to another bDMARD were evaluated in axSpA patients. |
Similar content being viewed by others
References
Deodhar A, Gensler LS, Kay J, Maksymowych WP, Haroon N, Landewé R, Rudwaleit M, Hall S, Bauer L, Hoepken B, de Peyrecave N, Kilgallen B, van der Heijde D (2019) A fifty-two-week, randomized, placebo-controlled trial of certolizumab pegol in nonradiographic axial spondyloarthritis. Arthritis Rheumatol. 71:1101-1111.: https://doi.org/10.1002/art.40866
Rodrigues-Manica S, Silva J, Cruz-Machado R, Coelho C, Duarte J, Vieira-Sousa E, Tavares-Costa J, Pimentel-Santos FM (2021) Biologic disease-modifying anti-rheumatic drugs and patient-reported outcomes in axial SpA: a systematic review and a call for action. Clin Rheumatol 40:33–41. https://doi.org/10.1007/s10067-020-05209-x
Sieper J, Landewé R, Magrey M, Anderson JK, Zhong S, Wang X, Lertratanakul A (2019) Predictors of remission in patients with non-radiographic axial spondyloarthritis receiving open-label adalimumab in the ABILITY-3 study. RMD Open. 7;5:e000917.: https://doi.org/10.1136/rmdopen-2019-000917
Shimabuco AY, Gonçalves CR, Moraes JCB, Waisberg MG, Ribeiro ACM, Sampaio-Barros PD, Goldenstein-Schainberg C, Bonfa E, Saad CGS (2018) Factors associated with ASDAS remission in a long-term study of ankylosing spondylitis patients under tumor necrosis factor inhibitors. Adv Rheumatol. 4;58:40.: https://doi.org/10.1186/s42358-018-0040-x
Chen X, Zhang T, Wang W, Xue J (2018) Analysis of relapse rates and risk factors of tapering or stopping pharmacologic therapies in axial spondyloarthritis patients with sustained remission. Clin Rheumatol 37:1625–1632. https://doi.org/10.1007/s10067-018-4084-4
Pradeep DJ, Keat AC, Gaffney K, Brooksby A, Leeder J, Harris C (2008) Switching anti-TNF therapy in ankylosing spondylitis. Rheumatology (Oxford) 47:1726–1727. https://doi.org/10.1093/rheumatology/ken334
Haberhauer G, Strehblow C, Fasching P (2010) Observational study of switching anti-TNF agents in ankylosing spondylitis and psoriatic arthritis versus rheumatoid arthritis. Wien Med Wochenschr 160:220–4. https://doi.org/10.1007/s10354-010-0795-0
Monti S, Todoerti M, Codullo V, Favalli EG, Biggioggero M, Becciolini A, Montecucco C, Caporali R (2018) Prevalence of Ankylosing Spondylitis Disease Activity Score (ASDAS) inactive disease in a cohort of patients treated with TNF-alpha inhibitors. Mod Rheumatol 28:542–549. https://doi.org/10.1080/14397595.2017.1367076
Landewé R, van Tubergen A (2015) Clinical tools to assess and monitor spondyloarthritis. Curr Rheumatol Rep. 17:47.:https://doi.org/10.1007/s11926-015-0522-3
Machado PM, Deodhar A (2019). Treat-to-target in axial spondyloarthritis: gold standard or fools’ gold? Curr Opin Rheumatol. 31:344–348.:https://doi.org/10.1097/BOR.0000000000000625
Deodhar A, Reveille JD, van den Bosch F, Braun J, Burgos-Vargas R, Caplan L, Clegg DO, Colbert RA, Gensler LS, van der Heijde D, van der Horst-Bruinsma IE, Inman RD, Maksymowych WP, Mease PJ, Raychaudhuri S, Reimold A, Rudwaleit M, Sieper J, Weisman MH, Landewé RB (2014) The concept of axial spondyloarthritis: joint statement of the spondyloarthritis research and treatment network and the Assessment of SpondyloArthritis international Society in response to the US Food and Drug Administration’s comments and concerns. Arthritis Rheumatol. 66:2649–2656.:https://doi.org/10.1002/art.38776
Poddubnyy D, Gensler LS (2014) Spontaneous, drug-induced, and drug-free remission in peripheral and axial spondyloarthritis. Best Pract Res Clin Rheumatol 28:807–818. https://doi.org/10.1016/j.berh.2014.10.005
Hernández-Breijo B, Plasencia-Rodríguez C, Navarro-Compán V, Martínez-Feito A, Jochems A, Kneepkens EL, Wolbink GJ, Rispens T, Diego C, Pascual-Salcedo D, Balsa A (2019) Association between concomitant csDMARDs and clinical response to TNF inhibitors in overweight patients with axial spondyloarthritis. Arthritis Res Ther. 211:66.:https://doi.org/10.1186/s13075-019-1849-3
Carvalho PD, Ruyssen-Witrand A, Fonseca J, Marreiros A, Machado PM (2020) Determining factors related to impaired spinal and hip mobility in patients with axial spondyloarthritis: longitudinal results from the DESIR cohort. RMD Open. 6:e001356.:https://doi.org/10.1136/rmdopen-2020-001356
Akgul O, Bodur H, Ataman S, Yurdakul FG, Capkin E, Gurer G, Sezer I, Duruoz MT, Melikoglu MA, Cay HF, Rezvani A, Yagci I, Gogus F, Kamanli A, Cevik R (2020) Clinical performance of ASAS Health Index in patients with ankylosing spondylitis and non-radiographic axial spondyloarthritis: real-world evidence from Multicenter Nationwide Registry. Rheumatol Int. 40:1793–1801.:https://doi.org/10.1007/s00296-020-04680-8
Landewé RB, van der Heijde D, Dougados M, Baraliakos X, Van den Bosch FE, Gaffney K, Bauer L, Hoepken B, Davies OR, de Peyrecave N, Thomas K, Gensler LS (2020) Maintenance of clinical remission in early axial spondyloarthritis following certolizumab pegol dose reduction. Ann Rheum Dis. 79:920–928.:https://doi.org/10.1136/annrheumdis-2019-216839
Landewé R, van der Heijde D, Dougados M, Baraliakos X, Van den Bosch F, Gaffney K, Bauer L, Hoepken B, de Peyrecave N, Thomas K, Gensler LS (2020) Induction of sustained clinical remission in early axial spondyloarthritis following certolizumabpegol treatment: 48-week outcomes from C-OPTIMISE. Rheumatol Ther. 7:581–599.: https://doi.org/10.1007/s40744-020-00214-7.
Lubrano E, Perrotta FM, Marchesoni A, D’Angelo S, Ramonda R, Addimanda O et al (2015) Remission in nonradiographic axial spondyloarthritis treated with anti-tumor necrosis factor-a drugs: an Italian multicenter study. J Rheumatol 42:258–263
van der Heijde D, Deodhar A, Braun J, Mack M, Hsu B, Gathany TA et al (2014) The effect of golimumab therapy on disease activity and health-related quality of life in patients with ankylosing spondylitis: 2-year results of the GO-RAISE trial. J Rheumatol 41:1095–1103
Zochling J, Braun J (2006) Remission in ankylosing spondylitis. Clin Exp Rheumatol. 24:S-88–92.
Ziade N, Abi Karam G, Merheb G, Mallak I, Irani L, Alam E, Messaykeh J, Menassa J, Mroue’ K, Uthman I, Masri AF, Ghorra P, Witte T, Baraliakos X (2019) HLA-B27 prevalence in axial spondyloarthritis patients and in blood donors in a Lebanese population: Results from a nationwide study. Int J Rheum Dis. 22:708–714.:https://doi.org/10.1111/1756-185X.13487.
Akassou A, Yacoubi H, Jamil A, Dakka N, Amzazi S, Sadki K, Niamane R, Elhassani S, Bakri Y (2015) Prevalence of HLA-B27 in Moroccan healthy subjects and patients with ankylosing spondylitis and mapping construction of several factors influencing AS diagnosis by using multiple correspondence analysis. Rheumatol Int 35:1889–94. https://doi.org/10.1007/s00296-015-3342-x
Arévalo M, López-Medina C, Moreno Martinez-Losa M, Moltó A, Font P, Collantes-Estevez E, Gratacós J (2020) Role of HLA-B27 in the comorbidities observed in axial spondyloarthritis: data from COMOSPA. Joint Bone Spine 87:445–448. https://doi.org/10.1016/j.jbspin.2020.03.012
Kısaarslan AP, Sözeri B, Gündüz Z, Zararsız G, Poyrazoğlu H, Düşünsel R (2019) Evaluation of factors affecting the duration of disease-modifying anti-rheumatic drugs application in patients with enthesitis-related arthritis. Eur J Rheumatol 6:130–35. https://doi.org/10.5152/eurjrheum.2019.18180
Soubrier M, Pereira B, Fan A, Frayssac T, Couderc M, Malochet-Guinamand S, Mathieu S, Tatar Z, Tournadre A, Dubost JJ (2018) Retention rates of adalimumab, etanercept, and infliximab as first- or second-line biotherapies for spondyloarthritis patients in daily practice in Auvergne (France). Int J Rheum Dis 21:1986–1992. https://doi.org/10.1111/1756-185X.13375
Sebastian A, Wojtala P, Lubiński Ł, Mimier M, Chlebicki A, Wiland P (2017) Disease activity in axial spondyloarthritis after discontinuation of TNF inhibitors therapy. Reumatologia 55:157–162. https://doi.org/10.5114/reum.2017.69775
Landewé R, Sieper J, Mease P, Inman RD, Lambert RG, Deodhar A, Marzo-Ortega H, Magrey M, Kiltz U, Wang X, Li M, Zhong S, Mostafa NM, Lertratanakul A, Pangan AL, Anderson JK (2018) Efficacy and safety of continuing versus withdrawing adalimumab therapy in maintaining remission in patients with non-radiographic axial spondyloarthritis (ABILITY-3): a multicentre, randomised, double-blind study. Lancet. 392:134–144.: https://doi.org/10.1016/S0140-6736(18)31362-X.
Deodhar A, Sandoval D, Holdsworth E, Booth N, Hunter T (2020) Use and switching of biologic therapy in patients with non-radiographic axial spondyloarthritis: a patient and provider survey in the United States. Rheumatol Ther 7:415–423. https://doi.org/10.1007/s40744-020-00208-5
Glintborg B, Østergaard M, Krogh NS, Tarp U, Manilo N, Loft AG, Hansen A, Schlemmer A, Fana V, Lindegaard HM, Nordin H, Rasmussen C, Ejstrup L, Jensen DV, Petersen PM, Hetland ML (2013) Clinical response, drug survival and predictors thereof in 432 ankylosing spondylitis patients after switching tumour necrosis factor α inhibitor therapy: results from the Danish nationwide DANBIO registry. Ann Rheum Dis 72:1149–1155. https://doi.org/10.1136/annrheumdis-2012-201933
Hartung W, Nigg A, Strunk J, Wolff B (2018) Clinical assessment and ultrasonography in the follow-up of enthesitis in patients with spondyloarthritis: a multicenter ultrasound study in daily clinical practice Open Access. Rheumatol 10(161):169. https://doi.org/10.2147/OARRR.S179472
Palominos PE, de Campos APB, Ribeiro SLE, Xavier RM, Xavier JW, de Oliveira FB, Guerra B, Saldanha C, Mancuso ACB, Kohem CL, Gasparin AA, Sampaio-Barros PD (2019) Correlation of enthesitis indices with disease activity and function in axial and peripheral spondyloarthritis: a cross-sectional study comparing MASES, SPARCC and LEI. Adv Rheumatol. 59:23.:https://doi.org/10.1186/s42358-019-0066-8.
Berg KH, Rohde G, Pripp A, Prøven A, Pirelli Benestad EE, Østensen M, Haugeberg G (2021) Increased proportion of comorbidities but no deterioration of sexual QOL during a 5-year follow-up in patients with axSpA in the biologic treatment era. Rheumatology (Oxford). 7: keaa887.:https://doi.org/10.1093/rheumatology/keaa887
Deodhar A, Yu D (2017) Switching tumor necrosis factor inhibitors in the treatment of axial spondyloarthritis. Semin Arthritis Rheum 47:343–350. https://doi.org/10.1016/j.semarthrit.2017.04.005
Lee S, Park YJ, Lee JY (2019) The effect of tumor necrosis factor-alpha inhibitors on uveitis in patients with ankylosing spondylitis. J Korean Med Sci. 4:e278.:https://doi.org/10.3346/jkms.2019.34.e278.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bodur, H., Yurdakul, F.G., Ataman, S. et al. Where we are in treat to target era? Predictive factors for remission and drug switching in patients with axial spondyloarthritis: a real-life evidence from BioStaR nationwide registry. Clin Rheumatol 41, 2053–2063 (2022). https://doi.org/10.1007/s10067-022-06145-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06145-8