Abstract
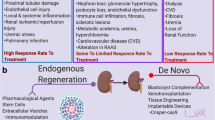
The availability of kidney and other organs from matching donors is not enough for many patients on demand for organ transplant. Unfortunately, this situation is not better despite the many of new interesting projects of promoting family, cross or domino transplants. These inexorable global statistics forced medical researchers to find a new potential therapeutic option that would guarantee safety and efficacy for the treatment of ESRD comparable to kidney transplantation. The aim of our review is to summarize the scientific literature that relating to the modern as well as innovative experimental methods and possibilities of kidney regeneration and, in addition, to find whether the regenerative medicine field will be a new hope for curing the patient with renal disease complications. The most important achievements in the field of regenerative medicine of kidney, which were mentioned and described here, are currently cumulated in 4 areas of interest: stem cell-based therapies, neo-kidneys with specially designed scaffolds or cell-seeded matrices, bioartificial kidneys and innovative nanotechnologically bioengineered solutions. Nowadays, we can add some remarks that the regenerative medicine is still insufficient to completely replace current therapy methods used in patients with chronic kidney disease especially with the end-stage renal disease where in many cases kidney transplantation is the only one chance. But we think that development of regenerative medicine especially in the last 20 years brings us more and more closer to solve many of today’s problems at the frontier of nephrology and transplantology.

Similar content being viewed by others
References
Murray JE. Ronald Lee Herrick Memorial: June 15, 1931-December 27, 2010. Am J Transplant. 2011;11:419.
Tangri N, Stevens LA, Griffith J, Tighiouart H, Djurdjev O, Naimark D, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA. 2011;305:1553–9.
Zoccali C, Kramer A, Jager KJ. Epidemiology of CKD in Europe: an uncertain scenario. Nephrol Dial Transplant. 2010;25:1731–3.
Nordio M, Limido A, Maggiore U, Nichelatti M, Postorino M, Quintaliani G. Italian dialysis and transplantation registry. Am J Kidney Dis. 2012;59:819–28.
Martínez-Mier G, Rayhilloye SC, Katz DA. Cadaveric kidney transplant using horseshoe kidney: report of two cases. Cir Cir. 2005;73:211–6.
Nowicki M, Zwiech R. Chronic renal failure in non-renal organ transplant recipients. Ann Transplant. 2005;10:54–7.
Czyżewski Ł, Wyzgał J. The adequacy of transplantation education in the ESRD population in Poland. Ann Transplant. 2012;17:62–73.
Cheng K, Rai P, Plagov A, Lan X. Transplantation of bone marrow-derived MSCs improves cisplatinum-induced renal injury through paracrine mechanisms. Exp Mol Pathol. 2013;94:466–73.
Winkelmayer WC, Glynn RJ, Levin R, Owen WF Jr, Avorn J. Determinants of delayed nephrologist referral in patients with chronic kidney disease. Am J Kidney Dis. 2001;38:1178–84.
Demoulin N, Beguin C, Labriola L, Jadoul M. Preparing renal replacement therapy in stage 4 CKD patients referred to nephrologists: a difficult balance between futility and insufficiency. A cohort study of 386 patients followed in Brussels. Nephrol Dial Transplant. 2011;26:220–6.
Roderick P, Davies R, Jones C, Feest T, Smith S, Farrington K. Simulation model of renal replacement therapy: predicting future demand in England. Nephrol Dial Transplant. 2004;19:692–701.
Saweirs WW, Goddard J. What are the best treatments for early chronic kidney disease? A background paper prepared for the UK consensus conference on early chronic kidney disease. Nephrol Dial Transplant. 2007;22:ix31–8.
Bauer C, Melamed ML, Hostetter TH. Staging of chronic kidney disease: time for a course correction. J Am Soc Nephrol. 2008;19:844–6.
Bentata Y, Haddiya I, Latrech H, Serraj K, Abouqal R. Progression of diabetic nephropathy, risk of end-stage renal disease and mortality in patients with type-1 diabetes. Saudi J Kidney Dis Transpl. 2013;24:392–402.
Chapman RJ, Templeton M, Ashworth S, Broomhead R, McLean A, Brett SJ. Long-term survival of chronic dialysis patients following survival from an episode of multiple-organ failure. Crit Care. 2009;13:R65.
McLaughlin K, Jones B, Mactier R, Porteus C. Long-term vascular access for hemodialysis using silicon dual-lumen catheters with guidewire replacement of catheters for technique salvage. Am J Kidney Dis. 1997;29:553–9.
Himmelfarb J, Ikizler TA. Hemodialysis. N Engl J Med. 2010;363:1833–45.
Himmelfarb J. Hemodialysis complications. Am J Kidney Dis. 2005;45:1122–31.
Hiesse C, Pessione F, Cohen S. Kidney grafts from elderly donors. Presse Med. 2003;32:942–51.
de Klerk M, Zuidema WC, IJzermans JN, Weimar W. Alternatives for unsuccessful living donor kidney exchange pairs. Clin Transpl 2010;327–332.
Silkensen JR. Long-term complications in renal transplantation. J Am Soc Nephrol. 2000;11:582–8.
Lewandowska D, Pazik J, Gozdowska J, Wyzgał J, Szmidt J, Gałązka Z, et al. Medical problems with potential living kidney donors. Ann Transplant. 2009;14:69–69.
Arulkumaran N, Annear NM, Singer M. Patients with end-stage renal disease admitted to the intensive care unit: systematic review. Br J Anaesth. 2013;110:13–20.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–12.
Kellum JA, Lameire N, For the KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care. 2013;17:204.
Bläser D, Weiler N. Acute kidney injury-prevention, risk stratification and biomarkers. Anasthesiologie Intensivmedizine Notfallmedizine Schmerztherapie. 2013;48:122–8.
Endre ZH, Pickering JW. Acute kidney injury clinical trial design: old problems, new strategies. Pediatr Nephrol. 2013;28:207–17.
Himmelfarb J. Acute kidney injury in the elderly: problems and prospects. Semin Nephrol. 2009;29:658–64.
Mason C, Dunnill P. A brief definition of regenerative medicine. Regen Med. 2008;3:1–5.
Khang D, Carpenter J, Chun YW, Pareta R, Webster TJ. Nanotechnology for regenerative medicine. Biomed Microdevices. 2010;12:575–87.
Langer R, Vacanti JP. Tissue engineering. Science. 1993;260:920–6.
Kaźnica A, Joachimiak R, Drewa T, Drewa G. Application of tissue engineering in selected branches of regenerative medicine. Med Biol Sci. 2007;21:9–14.
Egli RJ, Luginbuehl R. Tissue engineering-nanomaterials in the musculoskeletal system. Swiss Med Wkly. 2012;142:w13647.
Gunatillake PA, Adhikari R. Biodegradable synthetic polymers for tissue engineering. Eur Cell Mater. 2003;20:1–16.
Bajek A, Drewa T, Joachimiak R, Marszałek A, Gagat M, Grzanka A. Stem cells for urinary tract regeneration. Cen Eur J Urol. 2012;65:7–10.
Olson JL, Atala A, Yoo JJ. Tissue engineering: current strategies and future directions. Chonnam Med J. 2011;47:1–13.
Pokrywczynska M, Krzyzanowska S, Jundzill A, Adamowicz J, Drewa T. Differentiation of stem cells into insulin-producing cells: current status and challenges. Arch Immunol Ther Exp (Warsz). 2013;61:149–58.
Czajkowski R, Pokrywczynska M, Placek W, Zegarska B, Tadrowski T, Drewa T. Transplantation of cultured autologous melanocytes: hope or danger? Cell Transplant. 2010;19:639–43.
Reza HM, Ng BY, Gimeno FL, Phan TT, Ang LP. Umbilical cord lining stem cells as a novel and promising source for ocular surface regeneration. Stem Cell Rev. 2011;7:935–47.
Proffen B, von Keudell A, Vavken P. Evidence-based therapy for cartilage lesions in the knee—regenerative treatment options. Z Orthop Unfall. 2012;150:280–9.
Atala A, Kasper FK, Mikos AG. Engineering complex tissues. Sci Transl Med. 2012;4:160rv12.
Drewa T, Joachimiak R, Kaznica A, Sarafian V, Pokrywczynska M. Hair stem cells for bladder regeneration in rats: preliminary results. Transplant Proc. 2009;41:4345–51.
Pokrywczyńska M, Jundziłł A, Bodnar M, Adamowicz J, Tworkiewicz J, Szylberg L, et al. Do mesenchymal stem cells modulate the milieu of reconstructed bladder wall? Arch Ther Exp 2013;61:483–93.
Koziak A, Kania P, Marcheluk A, Dmowski T, Szcześniewski R, Dorobek A. Reconstruction of long ureteral obstructions using xenogenic acellular collagen membranes. Ann Transplant. 2004;9:18–20.
Kloskowski T, Kowalczyk T, Nowacki M, Drewa T. Tissue engineering and ureter regeneration: is it possible. Int J Artif Organs. 2013;36:392–405.
Orlando G, Di Cocco P, D’Angelo M, Clemente K, Famulari A, Pisani F. Regenerative medicine applied to solid organ transplantation: where do we stand? Transplant Proc. 2010;42:1011–3.
Dubernard JM. The kidney. Bull Acad Natl Med. 2011;195:1661–7.
Witzgall R, Brown D, Schwarz C, Bonventre JV. Localization of proliferating cell nuclear antigen, vimentin, c-Fos, and clusterin in the postischemic kidney. Evidence for a heterogenous genetic response among nephron segments, and a large pool of mitotically active and dedifferentiated cells. J Clin Invest. 1994;93:2175–88.
Kitamura S, Yamasaki Y, Kinomura M, Sugaya T, Sugiyama H, Maeshima Y, et al. Establishment and characterization of renal progenitor like cells from S3 segment of nephron in rat adult kidney. FASEB J. 2005;19:1789–97.
Bussolati B, Bruno S, Grange C, Buttiglieri S, Deregibus MC, Cantino D, et al. Isolation of renal progenitor cells from adult human kidney. Am J Pathol. 2005;166:545–55.
da Silva Meirelles L, Chagastelles PC, Nardi NB. Mesenchymal stem cells reside in virtually all post-natal organs and tissues. J Cell Sci. 2006;119:2204–13.
Gupta S, Verfaillie C, Chmielewski D, Kren S, Eidman K, Connaire J, et al. Isolation and characterization of kidney-derived stem cells. J Am Soc Nephrol. 2006;17:3028–40.
Sagrinati C, Netti GS, Mazzinghi B, Lazzeri E, Liotta F, Frosali F, et al. Isolation and characterization of multipotent progenitor cells from the Bowman’s capsule of adult human kidneys. J Am Soc Nephrol. 2006;17:2443–56.
Bruno S, Bussolati B, Grange C, Collino F, di Cantogno LV, Herrera MB, et al. Isolation and characterization of resident mesenchymal stem cells in human glomeruli. Stem Cells Dev. 2009;18:867–80.
Ward HH, Romero E, Welford A, Pickett G, Bacallao R, Gattone VH 2nd, et al. Adult human CD133/1(+) kidney cells isolated from papilla integrate into developing kidney tubules. Biochim Biophys Acta. 2011;1812:1344–57.
De Broe ME. Tubular regeneration and the role of bone marrow cells: ‘stem cell therapy’-a panacea? Nephrol Dial Transplant. 2005;20:2318–20.
Tögel F, Hu Z, Weiss K, Isaac J, Lange C, Westenfelder C. Administered mesenchymal stem cells protect against ischemic acute renal failure through differentiation-independent mechanisms. Am J Physiol Renal Physiol. 2005;289:F31–42.
Lin F, Cordes K, Li L, Hood L, Couser WG, Shankland SJ, et al. Hematopoietic stem cells contribute to the regeneration of renal tubules after renal ischemia-reperfusion injury in mice. J Am Soc Nephrol. 2003;14:1188–99.
Stroo I, Stokman G, Teske GJ, Florquin S, Leemans JC. Haematopoietic stem cell migration to the ischemic damaged kidney is not altered by manipulating the SDF-1/CXCR4-axis. Nephrol Dial Transplant. 2009;24:2082–8.
Gupta S, Verfaillie C, Chmielewski D, Kim Y, Rosenberg ME. A role for extrarenal cells in the regeneration following acute renal failure. Kidney Int. 2002;62:1285–90.
Humphreys BD, Valerius MT, Kobayashi A, Mugford JW, Soeung S, Duffield JS, et al. Intrinsic epithelial cells repair the kidney after injury. Cell Stem Cell. 2008;2:284–91.
Imasawa T, Utsunomiya Y, Kawamura T, Zhong Y, Nagasawa R, Okabe M, et al. The potential of bone marrow-derived cells to differentiate to glomerular mesangial cells. J Am Soc Nephrol. 2001;12:1401–9.
Ito T, Suzuki A, Imai E, Okabe M, Hori M. Bone marrow is a reservoir of repopulating mesangial cells during glomerular remodeling. J Am Soc Nephrol. 2001;12:2625–35.
Li J, Deane JA, Campanale NV, Bertram JF, Ricardo SD. The contribution of bone marrow-derived cells to the development of renal interstitial fibrosis. Stem Cells. 2007;25:697–706.
Poulsom R, Forbes SJ, Hodivala-Dilke K, Ryan E, Wyles S, Navaratnarasah S, et al. Bone marrow contributes to renal parenchymal turnover and regeneration. J Pathol. 2001;195:229–35.
Lin F, Moran A, Igarashi P. Intrarenal cells, not bone marrow-derived cells, are the major source for regeneration in postischemic kidney. J Clin Invest. 2005;115:1756–64.
Fang TC, Alison MR, Cook HT, Jeffery R, Wright NA, Poulsom R. Proliferation of bone marrow-derived cells contributes to regeneration after folic acid-induced acute tubular injury. J Am Soc Nephrol. 2005;16:1723–32.
Iwasaki M, Adachi Y, Minamino K, Suzuki Y, Zhang Y, Okigaki M, et al. Mobilization of bone marrow cells by G-CSF rescues mice from cisplatin-induced renal failure, and M-CSF enhances the effects of G-CSF. J Am Soc Nephrol. 2005;16:658–66.
Zhang H, Bai H, Yi Z, He X, Mo S. Effect of stem cell factor and granulocyte-macrophage colony-stimulating factor-induced bone marrow stem cell mobilization on recovery from acute tubular necrosis in rats. Ren Fail. 2012;34:350–7.
Tögel F, Isaac J, Hu Z, Weiss K, Westenfelder C. Renal SDF-1 signals mobilization and homing of CXCR4-positive cells to the kidney after ischemic injury. Kidney Int. 2005;67:1772–84.
Burst V, Pütsch F, Kubacki T, Völker LA, Bartram MP, Müller RU, et al. Survival and distribution of injected haematopoietic stem cells in acute kidney injury. Nephrol Dial Transplant. 2013;28:1131–9.
Morigi M, Imberti B, Zoja C, Corna D, Tomasoni S, Abbate M, et al. Mesenchymal stem cells are renotropic, helping to repair the kidney and improve function in acute renal failure. J Am Soc Nephrol. 2004;15:1794–804.
Herrera MB, Bussolati B, Bruno S, Fonsato V, Romanazzi GM, Camussi G. Mesenchymal stem cells contribute to the renal repair of acute tubular epithelial injury. Int J Mol Med. 2004;14:1035–41.
Bruce SJ, Rea RW, Steptoe AL, Busslinger M, Bertram JF, Perkins AC. In vitro differentiation of murine embryonic stem cells toward a renal lineage. Differentiation. 2007;75:337–49.
Nishikawa M, Yanagawa N, Kojima N, Yuri S, Hauser PV, Jo OD, et al. Stepwise renal lineage differentiation of mouse embryonic stem cells tracing in vivo development. Biochem Biophys Res Commun. 2012;417:897–902.
Ren X, Zhang J, Gong X, Niu X, Zhang X, Chen P, et al. Differentiation of murine embryonic stem cells toward renal lineages by conditioned medium from ureteric bud cells in vitro. Acta Biochim Biophys Sin (Shanghai). 2010;42:464–71.
Kim D, Dressler GR. Nephrogenic factors promote differentiation of mouse embryonic stem cells into renal epithelia. J Am Soc Nephrol. 2005;16:3527–34.
Morizane R, Monkawa T, Itoh H. Differentiation of murine embryonic stem and induced pluripotent stem cells to renal lineage in vitro. Biochem Biophys Res Commun. 2009;390:1334–9.
Rosines E, Johkura K, Zhang X, Schmidt HJ, Decambre M, Bush KT, et al. Constructing kidney-like tissues from cells based on programs for organ development: toward a method of in vitro tissue engineering of the kidney. Tissue Eng Part A. 2010;16:2441–55.
Rosines E, Sampogna RV, Johkura K, Vaughn DA, Choi Y, Sakurai H, et al. Staged in vitro reconstitution and implantation of engineered rat kidney tissue. Proc Natl Acad Sci USA. 2007;104:20938–43.
Joraku A, Stern KA, Atala A, Yoo JJ. In vitro generation of three-dimensional renal structures. Methods. 2009;47:129–33.
Osafune K, Takasato M, Kispert A, Asashima M, Nishinakamura R. Identification of multipotent progenitors in the embryonic mouse kidney by a novel colony-forming assay. Development. 2006;133:151–61.
Mae S, Shono A, Shiota F, Yasuno T, Kajiwara M, Gotoda-Nishimura N, Arai S, Sato-Otubo A, Toyoda T, Takahashi K, Nakayama N, Cowan CA, Aoi T, Ogawa S, McMahon AP, Yamanaka S, Osafune K. Monitoring and robust induction of nephrogenic intermediate mesoderm from human pluripotent stem cells. Nat Commun. 2013;4:1367.
Usui JI, Kobayashi T, Yamaguchi T, Knisely AS, Nishinakamura R, Nakauchi H. Generation of kidney from pluripotent stem cells via blastocyst complementation. Am J Pathol. 2012;180:2417–26.
Rogers SA, Talcott M, Hammerman MR. Transplantation of pig metanephroi. ASAIO J. 2003;49:48–52.
Dekel B, Burakova T, Arditti FD, Reich-Zeliger S, Milstein O, Aviel-Ronen S, et al. Human and porcine early kidney precursors as a new source for transplantation. Nat Med. 2003;9:53–60.
Hammerman MR. Renal organogenesis from transplanted metanephric primordial. J Am Soc Nephrol. 2004;15:1126–32.
Matsumoto K, Yokoo T, Yokote S, Utsunomiya Y, Ohashi T, Hosoya T. Functional development of a transplanted embryonic kidney: effect of transplantation site. J Nephrol. 2012;25:50–5.
Kooreman NG, Wu JC. Tumorigenicity of pluripotent stem cells: biological insights from molecular imaging. J R Soc Interface. 2010;7:S753–63.
Tang C, Weissman IL, Drukker M. The safety of embryonic stem cell therapy relies on teratoma removal. Oncotarget. 2012;3:7–8.
Singaravelu K, Padanilam BJ. In vitro differentiation of MSC into cells with a renal tubular epithelial-like phenotype. Ren Fail. 2009;31:492–502.
Jia X, Xie X, Feng G, Lű H, Zhao Q, Che Y, et al. Bone marrow-derived cells can acquire renal stem cells properties and ameliorate ischemia-reperfusion induced acute renal injury. BMC Nephrol. 2012;13:105.
Baer PC, Bereiter-Hahn J, Missler C, Brzoska M, Schubert R, Gauer S, et al. Conditioned medium from renal tubular epithelial cells initiates differentiation of human mesenchymal stem cells. Cell Prolif. 2009;42:29–37.
Baer PC, Döring C, Hansmann ML, Schubert R, Geiger H. New insights into epithelial differentiation of human adipose-derived stem cells. J Tissue Eng Regen Med. 2011;7:271–8.
Perin L, Giuliani S, Jin D, Sedrakyan S, Carraro G, Habibian R, et al. Renal differentiation of amniotic fluid stem cells. Cell Prolif. 2007;40:936–48.
Siegel N, Valli A, Fuchs C, Rosner M, Hengstschläger M. Induction of mesenchymal/epithelial marker expression in human amniotic fluid stem cells. Reprod Biomed Online. 2009;19:838–46.
Siegel N, Rosner M, Unbekandt M, Fuchs C, Slabina N, Dolznig H, et al. Contribution of human amniotic fluid stem cells to renal tissue formation depends on mTOR. Hum Mol Genet. 2010;19:3320–31.
Hauser PV, De Fazio R, Bruno S, Sdei S, Grange C, Bussolati B, et al. Stem Cells derived from human amniotic fluid contribute to acute kidney injury recovery. Am J Pathol. 2010;177:2011–21.
Rosner M, Schipany K, Gundacker C, Shanmugasundaram B, Li K, Fuchs C, et al. Renal differentiation of amniotic fluid stem cells: perspectives for clinical application and for studies on specific human genetic diseases. Eur J Clin Invest. 2011;42:677–84.
Lensch MW, Rao M. Induced pluripotent stem cells: opportunities and challenges. Regen Med. 2010;5:483–4.
Okita K, Yamanaka S. Induced pluripotent stem cells: opportunities and challenges. Philos Trans R Soc Lond B Biol Sci. 2011;366:2198–207.
Sullivan DC, Mirmalek-Sani SH, Deegan DB, Baptista PM, Aboushwareb T, Atala A, et al. Decellularization methods of porcine kidneys for whole organ engineering using a high-throughput system. Biomaterials. 2012;33:7756–64.
Orlando G, Farney AC, Iskandar SS, Mirmalek-Sani SH, Sullivan DC, Moran E, et al. Production and implantation of renal extracellular matrix scaffolds from porcine kidneys as a platform for renal bioengineering investigations. Ann Surg. 2012;256:363–70.
Park KM, Woo HM. Porcine bioengineered scaffolds as new frontiers in regenerative medicine. Transplant Proc. 2012;44:1146–50.
Nakayama KH, Batchelder CA, Lee CI, Tarantal AF. Decellularized rhesus monkey kidney as three-dimensional scaffold for renal tissue engineering. Tissue Eng Part A. 2010;16:2207–16.
Song JJ, Guyette JP, Gilpin SE, Gonzalez G, Vacanti JP, Ott HC. Regeneration and experimental orthotopic transplantation of a bioengineered kidney. Nat Med. 2013;19:646–51.
Bonandrini B, Figliuzzi M, Papadimou E, Morigi M, Perico N, Casiraghi F et al. Recellularization of well preserved acellular kidney scaffold using embryonic stem cells. Tissue Eng Part A 2014. doi:10.1089/ten.tea.2013.0269.
Wang PC, Takezawa T. Reconstruction of renal glomerular tissue using collagen vitrigel scaffold. J Biosci Bioeng. 2005;99:529–40.
Rosines E, Schmidt HJ, Nigam SK. The effect hyaluronic acid size and concentration on branching morphogenesis and tubule differentiation in developing kidney culture systems: potential applications to engineering of renal tissue. Biomaterials. 2007;28:4806–17.
Caldas HC, Fernandes IM, Kawasaki-Oyama RS, Baptista MA, Plepis AM, Martins VA, et al. Effect of stem cells seeded onto biomaterial on the progression of experimental kidney disease. Exp Biol Med (Maywood). 2011;236:746–54.
Lanza RP, Chung HY, Yoo JJ, Wettstein PJ, Blackwell C, Borson N, et al. Generation of histocompatible tissues using nuclear transplantation. Nat Biotechnol. 2002;20:689–96.
Lü SH, Lin Q, Liu YN, Gao Q, Hao T, Wang Y, et al. Self-assembly of renal cells into engineered renal tissue in collagen/matrigel scaffold in vitro. J Tissue Eng Regen Med. 2012;10:786–92.
Kim SS, Park HJ, Han J, Choi CY, Kim BS. Renal tissue reconstruction by the implantation of renal segments on biodegradable polymer scaffold. Biotechnol Lett. 2003;25:1505–8.
Palmer RA, Price JDE, English ET, Newell T. Clinical trials with the Kolff Twin Coil artificial kidney. Can Med Assoc J. 1957;77:850–5.
Tasnim F, Deng R, Hu M, Liour S, Li Y, Ni M, et al. Achievements and challenges in bioartificial kidney development. Fibrogenesis Tissue Repair. 2010;3:14.
Oo ZY, Deng R, Hu M, Ni M, Kandasamy K, Ibrahim MSB. The performance of primary human renal cells in hollow fiber bioreactors for bioartificial kidneys. Biomaterials. 2011;32:8806–15.
Humes HD, MacKay SM, Funke AJ, Buffington DA. Tissue engineering of a bioartificial renal tubule assist device: in vitro transport and metabolic characteristics. Kidney Int. 1999;55:2502–14.
Wüstenberg PW, Bräunlich H, Hagemann I. Modern study methods in experimental nephrology. Z Urol Nephrol. 1986;79:411–28.
Chang TM. Applications of artificial cells in medicine and biotechnology. Biomater Artif Cells Artif Organs. 1987;15:1–20.
Aebischer P, Ip TK, Panol G, Galletti PM. The bioartificial kidney: progress towards an ultrafiltration device with renal epithelial cells processing. Life Support Syst. 1987;5:159–68.
Humes HD, Fissell WH, Weitzel WF, Buffington DA, Westover AJ, MacKay SM, et al. Metabolic replacement of renal function in uremic animals with a bioartificial kidney containing human cells. Am J Kidney Dis. 2002;39:1078–87.
Sun J, Wang C, Zhu B, Larsen S, Wu J, Zhao W. Construction of an erythropoietin-expressing bioartificial renal tubule assist device. Ren Fail. 2011;33:54–60.
Narayanan K, Schumacher KM, Tasnim F, Kandasamy K, Schumacher A, Ni M, et al. Human embryonic stem cells differentiate into functional renal proximal tubular-like cells. Kidney Int. 2013;83:593–603.
Pollock CA. Toward a bioartificial kidney: will embryonic stem cells be the answer? Kidney Int. 2013;83:543–5.
Ng CP, Zhuang Y, Lin AWH, Teo JCM. Fibrin-based tissue-engineered renal proximal tubule for bioartificial kidney devices: development, characterization and in vitro transport study. Int J Tissue Eng. 2013;. doi:10.1155/2013/319476.
Sanechika N, Sawada K, Usui Y, Hanai K, Kakuta T, Suzuki H, et al. Development of bioartificial renal tubule devices with lifespan-extended human renal proximal tubular epithelial cells. Nephrol Dial Transplant. 2011;26:2761–9.
Saito A, Sawada K, Fujimura S, Suzuki H, Hirukawa T, Tatsumi R, et al. Evaluation of bioartificial renal tubule device prepared with lifespan-extended human renal proximal tubular epithelial cells. Nephrol Dial Transplant. 2012;27:3091–9.
Fujita Y, Terashima M, Kakuta T, Itoh J, Tokimasa T, Brown D, et al. Transcellular water transport and stability of expression in aquaporin 1-transfected LLC-PK1 cells in the development of a portable bioartificial renal tubule device. Tissue Eng. 2004;10:711–22.
Humes HD. Tissue engineering of a bioartificial kidney: a universal donor organ. Transplant Proc. 1996;28:2032–5.
de Francisco AL, Piñera C. Challenges and future of renal replacement therapy. Hemodial Int. 2006;10:S19–23.
Zhang H, Tasnim F, Ying JY, Zink D. The impact of extracellular matrix coatings on the performance of human renal cells applied in bioartificial kidneys. Biomaterials. 2009;30:2899–911.
Cieslinski DA, Humes DH. Bioartificial kidney devices coated with cells suitable for use in vivo or ex vivo. Patent number EP 0746343 B1. 2 Jan 2004.
Cieslinski DA, Humes DH. Tissue engineering of a bioartificial kidney. Biotechnol Bioeng. 1994;43:678–81.
Tumlin J, Wali R, Williams W, Murray P, Tolwani AJ, Vinnikova AK, et al. Efficacy and safety of renal tubule cell therapy for acute renal failure. J Am Soc Nephrol. 2008;19:1034–40.
Humes HD, Weitzel WF, Bartlett RH, Swaniker FC, Paganini EP, Luderer JR, et al. Initial clinical results of the bioartificial kidney containing human cells in ICU patients with acute renal failure. Kidney Int. 2004;66:1578–88.
Nowacki M, Jundziłł A, Bieniek M, Kowalczyk T, Kloskowski T, Drewa T. Modern biomaterials as hemostatic dressings in kidney nephron sparing surgery (NSS)-murine model. A preliminary report. Polim Med. 2012;42:35–43.
Oo ZY, Kandasamy K, Tasnim F, Zink D. A novel design of bioartificial kidneys with improved cell performance and haemocompatibility. J Cell Mol Med. 2013;17:497–507.
Teo JC, Ng RR, Ng CP, Lin AW. Surface characteristics of acrylic modified polysulfone membranes improves renal proximal tubule cell adhesion and spreading. Acta Biomater. 2011;7:2060–9.
Zhang H, Lau SF, Heng BF, Teo PY, Alahakoon PK, Ni M, et al. Generation of easily accessible human kidney tubules on two-dimensional surfaces in vitro. J Cell Mol Med. 2011;15:1287–98.
Rastogi A, Nissenson AR. Technological advances in renal replacement therapy: five years and beyond. Clin J Am Soc Nephrol. 2009;4:S132–6.
Dankers PY, Boomker JM, Huizinga-van der Vlag A, Smedts FM, Harmsen MC, van Luyn MJ. The use of fibrous, supramolecular membranes and human tubular cells for renal epithelial tissue engineering: towards a suitable membrane for a bioartificial kidney. Macromol Biosci. 2010;10:1345–54.
Slater SC, Beachley V, Hayes T, Zhang D, Welsh GI, Saleem MA, et al. An in vitro model of the glomerular capillary wall using electrospun collagen nanofibres in a bioartificial composite basement membrane. PLoS One. 2011;6:e20802.
Ding F, Humes HD. The bioartificial kidney and bioengineered membranes in acute kidney injury. Nephron Exp Nephrol. 2008;109:e118–22.
Fissell WH, Manley S, Westover A, Humes HD, Fleischman AJ, Roy S. Differentiated growth of human renal tubule cells on thin-film and nanostructured materials. ASAIO J. 2006;52:221–7.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Nowacki, M., Kloskowski, T., Pokrywczyńska, M. et al. Is regenerative medicine a new hope for kidney replacement?. J Artif Organs 17, 123–134 (2014). https://doi.org/10.1007/s10047-014-0767-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-014-0767-z