Abstract
The ruptured anterior cruciate ligament (ACL) does not heal spontaneously. Therefore, the development of new healing techniques employing tissue engineering is vital. One of the aspects related to tissue-engineered artificial ligaments is the type of cell to be used for the artificial ligament. In this study, ligament cells from the ACL and periodontal ligament (PDL) were evaluated. In addition, we prepared highly oriented extracellular matrix (ECM) fiber scaffolds that mimicked the structure of the ligament and examined the cellular responses to these scaffolds. Elastin-A and collagen were used as the ECM proteins. Although the cells from the PDL (PDL fibroblasts [PDLFs]) showed approximately 2.1-fold higher expression of alkaline phosphatase (ALP; marker of osteogenic differentiation) than the ACL cells, the expression of ligament-related genes (for type I collagen, type III collagen, and tenomodulin) did not differ between PDLFs and ACL cells. Furthermore, the cellular responses (expression pattern of ligament-related genes and ALP activity) to the ECM were similar between ACL cells and PDLFs. In particular, elastin-A upregulated ALP and downregulated tenomodulin (TeM; a ligament marker) in ligament cells. In contrast, collagen maintained TeM expression in ligament cells. These results suggest that elastin-A promotes the osteogenic differentiation of ligament cells and that collagen maintains the phenotype of ligament cells.





Similar content being viewed by others
References
Hadjicostas PT, Soucacos PN, Koleganova N, Krohmer G, Berger I. Comparative and morphological analysis of commonly used autografts for anterior cruciate ligament reconstruction with the native ACL: an electron, microscopic and morphologic study. Knee Surg Sports Traumatol Arthrosc. 2008;16:1099–107.
Duthon VB, Barea C, Abrassart S, Fasel JH, Fritschy D, Menetrey J. Anatomy of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14:204–13.
Laurencin CT, Freeman JW. Ligament tissue engineering: an evolutionary materials science approach. Biomaterials. 2005;26:7530–6.
Somerman MJ, Archer SY, Imm GR, Foster RA. A comparative study of human periodontal ligament cells and gingival fibroblasts in vitro. J Dent Res. 1988;67:66–70.
Lekic P, McCulloch CA. Periodontal ligament cell population: the central role of fibroblasts in creating a unique tissue. Anat Rec. 1996;245:327–41.
Ramakrishnan PR, Lin WL, Sodek J, Cho MI. Synthesis of noncollagenous extracellular matrix proteins during development of mineralized nodules by rat periodontal ligament cells in vitro. Calcif Tissue Int. 1995;57:52–9.
Cheng MT, Yang HW, Chen TH, Lee OK. Isolation and characterization of multipotent stem cells from human cruciate ligaments. Cell Prolif. 2009;42:448–60.
Steinert AF, Kunz M, Prager P, Barthel T, Jakob F, Noth U, Murray MM, Evans CH, Porter RM. Mesenchymal stem cell characteristics of human anterior cruciate ligament outgrowth cells. Tissue Eng Part A. 2011;17:1375–88.
Zhang J, Pan T, Im HJ, Fu FH, Wang JH. Differential properties of human ACL and MCL stem cells may be responsible for their differential healing capacity. BMC Med. 2011;9:68.
Tanaka K, Iwasaki K, Feghali KE, Komaki M, Ishikawa I, Izumi Y. Comparison of characteristics of periodontal ligament cells obtained from outgrowth and enzyme-digested culture methods. Arch Oral Biol. 2011;56:380–8.
Wu LP, Wei X, Ling JQ, Liu L. The surface antigen expression of periodontal ligament cells and dental pulp cells in vitro. Hua Xi Kou Qiang Yi Xue Za Zhi. 2009;27:20–3.
Zhao Y, Wang C, Li S, Song H, Wei F, Pan K, Zhu K, Yang P, Tu Q, Chen J. Expression of Osterix in mechanical stress-induced osteogenic differentiation of periodontal ligament cells in vitro. Eur J Oral Sci. 2008;116:199–206.
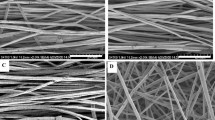
Mizutani N, Kawato H, Maeda Y, Takebayashi T, Miyamoto K, Horiuchi T. Multiple-type dynamic culture of highly oriented fiber scaffold for ligament regeneration. J Artif Organs. 2013;16:49–58.
Miyamoto K. Crosslinked elastin and process for producing the same. US Patent 7,125,960 B2 2006-10-24.
Miyamoto K, Atarashi M, Kadozono H, Shibata M, Koyama Y, Okai M, Inakuma A, Kitazono E, Kaneko H, Takebayashi T, Horiuchi T. Creation of cross-linked electrospun isotypic-elastin fibers controlled cell-differentiation with new cross-linker. Int J Biol Macromol. 2009;45:33–41.
Stylianou E, Jenner LA, Davies M, Coles GA, Williams JD. Isolation, culture and characterization of human peritoneal mesothelial cells. Kidney Int. 1990;37:1563–70.
Haddad-Weber M, Prager P, Kunz M, Seefried L, Jakob F, Murray MM, Evans CH, Noth U, Steinert AF. BMP12 and BMP13 gene transfer induce ligamentogenic differentiation in mesenchymal progenitor and anterior cruciate ligament cells. Cytotherapy. 2010;12:505–13.
Itaya T, Kagami H, Okada K, Yamawaki A, Narita Y, Inoue M, Sumita Y, Ueda M. Characteristic changes of periodontal ligament-derived cells during passage. J Periodontal Res. 2009;44:425–33.
Kimura N, Shukunami C, Hakuno D, Yoshioka M, Miura S, Docheva D, Kimura T, Okada Y, Matsumura G, Shin’oka T, Yozu R, Kobayashi J, Ishibashi-Ueda H, Hiraki Y, Fukuda K. Local tenomodulin absence, angiogenesis, and matrix metalloproteinase activation are associated with the rupture of the chordae tendineae cordis. Circulation. 2008;118:1737–47.
Shukunami C, Takimoto A, Miura S, Nishizaki Y, Hiraki Y. Chondromodulin-I and tenomodulin are differentially expressed in the avascular mesenchyme during mouse and chick development. Cell Tissue Res. 2008;332:111–22.
Shukunami C, Hiraki Y. Chondromodulin-I and tenomodulin: the negative control of angiogenesis in connective tissue. Curr Pharm Des. 2007;13:2101–12.
Burgess R, Cserjesi P, Ligon KL, Olson EN. Paraxis: a basic helix-loop-helix protein expressed in paraxial mesoderm and developing somites. Dev Biol. 1995;168:296–306.
Wlodarski KH, Reddi AH. Alkaline phosphatase as a marker of osteoinductive cells. Calcif Tissue Int. 1986;39:382–5.
Acknowledgments
This study was supported by a research grant (Yoshimi Memorial TMP Grant, 2010) from the Japanese Society for Artificial Organs (JSAO).
Conflict of interest
The authors have declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Mizutani, N., Kageyama, S., Yamada, M. et al. The behavior of ligament cells cultured on elastin and collagen scaffolds. J Artif Organs 17, 50–59 (2014). https://doi.org/10.1007/s10047-013-0736-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-013-0736-y