Abstract
Purpose
The aim of this study was to examine the postoperative outcomes and follow-up QOL of patients after AWR at a level-1 trauma centre in India.
Methods
The study cohort included AWR patients treated between January 2011 and July 2022. The Activities Assessment Scale (AAS) was used to measure QOL, and the Ventral Hernia Recurrence Inventory (VHRI) was used to determine the occurrence of recurrence. In patients suspected of having recurrence, thorough clinical examination and relevant imaging were performed to confirm or rule out recurrence.
Results
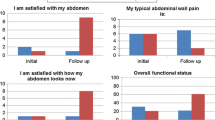
Out of 89 patients, 35 patients whose complete perioperative and follow-up data were available were enrolled. The mean age of the patients was 28 (SD, 9) years. The mean defect size was 14. 9 (SD, 7) cm. The mean time from laparotomy to AWR surgery was 21 months. During the postoperative course, 37% of patients developed complications, such as SSI and seroma. The mean follow-up time was 53 (SD, 43) months.
Upon comparing procedures involving the mesh placed in the sublay position with procedures involving the mesh placed in other positions, no statistically significant difference in the recurrence rate (one in each group, p = 0.99), surgical complication rate (33% v/s 66%, p = 0.6), or mean AAS QOL score (94.7 v/s 98, p = 0.4) was observed. The specificity of the VHRI for diagnosing recurrence was 79%.
Conclusion
Overall, the recurrence rate was low in these patients despite the presence of large hernia defects. Long-term QOL was not affected by the specific procedure used. Timely planning and execution are more important than the specific repair approach for post-trauma laparotomy ventral hernia.

Similar content being viewed by others
References
Coccolini F, Roberts D, Ansaloni L, Ivatury R, Gamberini E, Kluger Y, Moore EE, Coimbra R, Kirkpatrick AW, Pereira BM, Montori G (2018) The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Emerg Surg 13(1):1–6
Boele van Hensbroek P, Wind J, Dijkgraaf MG, Busch OR, Carel Goslings J (2009) Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg 33:199–207
Agarwal H, Bagaria D, Sagar S, Kumar S, Mishra B, Kumar V, Banerjee N, Gupta A (2022) Factors associated with inability to perform delayed primary fascial closure of open abdomen in trauma patients: a retrospective observational study. Indian J Surg 84:983–989
Tremblay LN, Feliciano DV, Schmidt J, Cava RA, Tchorz KM, Ingram WL, Salomone JP, Nicholas JM, Rozycki GS (2001) Skin only or silo closure in the critically ill patient with an open abdomen. Am J Surg 182(6):670–675
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571
Codner PA, Brasel KJ, deRoon-Cassini TA (2012) Staged abdominal repairs reduce long-term quality of life. Injury 43(9):1513–1516
Heniford BT, Ross SW, Wormer BA, Walters AL, Lincourt AE, Colavita PD, Kercher KW, Augenstein VA (2020) Preperitoneal ventral hernia repair: a decade long prospective observational study with analysis of 1023 patient outcomes. Ann Surg 271(2):364–374
de VriesReilingh TS, van Goor H, Rosman C, Bemelmans MH, de Jong D, van Nieuwenhoven EJ, van Engeland MI, Bleichrodt RP (2003) “Components separation technique” for the repair of large abdominal wall hernias. J Am Coll Surg 196(1):32–37
Holihan JL, Askenasy EP, Greenberg JA, Keith JN, Martindale RG, Roth JS, Mo J, Ko TC, Kao LS, Liang MK, Ventral Hernia Outcome Collaboration Writing Group (2016) Component separation vs bridged repair for large ventral hernias: a multi-institutional risk-adjusted comparison, systematic review, and meta-analysis. Surg Infect 17(1):17–26
Zosa BM, Como JJ, Kelly KB, He JC, Claridge JA (2016) Planned ventral hernia following damage control laparotomy in trauma: an added year of recovery but equal long-term outcome. Hernia 20:231–238
Rodriguez ED, Bluebond-Langner R, Silverman RP, Bochicchio G, Yao A, Manson PN, Scalea T (2007) Abdominal wall reconstruction following severe loss of domain: the R Adams Cowley Shock Trauma Center algorithm. Plast Reconstr Surg 120(3):669–680
DiCocco JM, Magnotti LJ, Emmett KP, Zarzaur BL, Croce MA, Sharpe JP, Shahan CP, Jiao H, Goldberg SP, Fabian TC (2010) Long-term follow-up of abdominal wall reconstruction after planned ventral hernia: a 15-year experience. J Am Coll Surg 210(5):686–695
Baucom RB, Ousley J, Feurer ID, Beveridge GB, Pierce RA, Holzman MD, Sharp KW, Poulose BK (2016) Patient reported outcomes after incisional hernia repair—establishing the ventral hernia recurrence inventory. Am J Surg 212(1):81–88
McCarthy M Jr, Jonasson O, Chang CH, Pickard AS, Giobbie-Hurder A, Gibbs J, Edelman P, Fitzgibbons R, Neumayer L (2005) Assessment of patient functional status after surgery. J Am Coll Surg 201(2):171–178
Chevrel JP, Rath AM (2000) Classification of incisional hernias of the abdominal wall. Hernia 4:7–11
Memon AA, Khan A, Zafar H, Murtaza G, Zaidi M (2013) Repair of large and giant incisional hernia with onlay mesh: perspective of a tertiary care hospital of a developing country. Int J Surg 11(1):41–45
Timmermans L, de Goede B, van Dijk SM, Kleinrensink GJ, Jeekel J, Lange JF (2014) Meta-analysis of sublay versus onlay mesh repair in incisional hernia surgery. Am J Surg 207(6):980–988
Luijendijk R, Hop W, van den Top M et al (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343:392–398
den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW (1996) Open surgical procedures for incisional hernias. Cochrane database systematic reviews: protocols. Wiley, Chichester
van Ramshorst GH, Eker HH, Hop WC, Jeekel J, Lange JF (2012) Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg 204(2):144–150
Liang MK, Clapp M, Li LT, Berger RL, Hicks SC, Awad S (2013) Patient satisfaction, chronic pain, and functional status following laparoscopic ventral hernia repair. World J Surg 37:530–537
Klima DA, Tsirline VB, Belyansky I, Dacey KT, Lincourt AE, Kercher KW, Heniford BT (2014) Quality of life following component separation versus standard open ventral hernia repair for large hernias. Surg innov 21(2):147–154
Funding
No funding was received for the study.
Author information
Authors and Affiliations
Contributions
DB, SG, AG, JA, NC, and AK: contributed in data collection. DB, SP, BM, and SK: did data analysis. DB, SS, PP, NC, and AG: prepared the manuscript. All authors analyses the final draft and approved before submission.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest.
Ethical approval, Human and animal rights and Informed consent
Ethical approval was granted fron Institute Ethics Committee vide ref. no. iec-80/03.03.2023, RP-09/2023 with waiver of informed consent in view of retrospective nature of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bagaria, D.K., Gupta, S., Pandey, S. et al. Abdominal wall reconstruction (AWR) for post-trauma laparotomy ventral hernia and follow-up assessment of functional quality of life (QOL): experience of a level-1 trauma centre in India. Hernia (2024). https://doi.org/10.1007/s10029-024-02978-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10029-024-02978-1