Abstract
Purpose
Currently, there are no reliable preoperative methods for predicting component separation (CS) during incisional hernia repair. By quantitatively measuring preoperative computed tomography (CT) imaging, we aimed to assess the value of hernia defect size, abdominal wall muscle quality, and hernia volume in predicting CS.
Methods
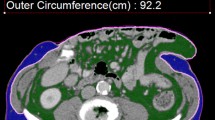
The data of 102 patients who underwent open Rives-Stoppa retro-muscular mesh repair for midline incisional hernia between January 2019 and March 2022 were retrospectively analyzed. The patients were divided into two groups: ‘‘CS group’’ patients who required CS to attempt fascial closure, and ‘‘non-CS’’ group patients who required only Rives-Stoppa retro-muscular release to achieve fascial closure. Hernia defect width, hernia defect angle, rectus width, abdominal wall muscle area and CT attenuation, hernia volume (HV), and abdominal cavity volume (ACV) were measured on CT images. The rectus width to defect width ratio (RDR), HV/ACV, and HV/peritoneal volume (PV; i.e., HV + ACV) were calculated. Differences between the indices of the two groups were compared. Logistic regression models were applied to analyze the relationships between the above CT parameters and CS. Receiver operator characteristic (ROC) curves were generated to evaluate the potential utility of CT parameters in predicting CS.
Results
Of the102 patients, 69 were in the non-CS group and 33 were in the CS group. Compared with the non-CS group, hernia defect width (P < 0.001), hernia defect angle (P < 0.001), and hernia volume (P < 0.001) were larger in the CS group, while RDR (P < 0.001) was smaller. The abdominal wall muscle area in the CS group was slightly greater than that in the non-CS group (P = 0.046), and there was no significant difference in the CT attenuation of the abdominal wall muscle between the two groups (P = 0.089). Multivariate logistic regression identified hernia defect width (OR 1.815, 95% CI 1.428–2.308, P < 0.001), RDR (OR 0.018, 95% CI 0.003–0.106, P < 0.001), hernia defect angle (OR 1.077, 95% CI 1.042–1.114, P < 0.001), hernia volume (OR 1.002, 95% CI 1.001–1.003, P < 0.001), and CT attenuation of abdominal wall muscle (OR 0.962, 95% CI 0.927–0.998, P = 0.037) as independent predictors of CS. Hernia defect width was the best predictor for CS, with a cut-off point of 9.2 cm and an area under the curve (AUC) of 0.890. The AUCs of RDR, hernia defect angle, hernia volume, and abdominal wall muscle CT attenuation were 0.843, 0.812, 0.747, and 0.572, respectively.
Conclusion
Quantitative CT measurements are of great value for preoperative prediction of CS. Hernia defect size, hernia volume, and the CT attenuation of abdominal wall muscle are all preoperative predictive indicators of CS.



Similar content being viewed by others
References
Ramirez OM, Ruas E, Dellon AL (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86(3):519–526. https://doi.org/10.1097/00006534-199009000-00023
Parikh RS, Faulkner J, Hooks WB 3rd, Hope WW (2020) An evaluation of tension measurements during myofascial release for hernia repair. Am Surg 86(9):1159–1162. https://doi.org/10.1177/0003134820945243
Pauli EM, Rosen MJ (2013) Open ventral hernia repair with component separation. Surg Clin N Am 93(5):1111–1133. https://doi.org/10.1016/j.suc.2013.06.010
Wegdam JA, Thoolen JMM, Nienhuijs SW, de Bouvy N, de VriesReilingh TS (2019) Systematic review of transversus abdominis release in complex abdominal wall reconstruction. Hernia 23(1):5–15. https://doi.org/10.1007/s10029-018-1870-5
Hope WW, Williams ZF, Rawles JW 3rd, Hooks WB 3rd, Clancy TV, Eckhauser FE (2018) Rationale and technique for measuring abdominal wall tension in hernia repair. Am Surg 84(9):1446–1449
Eriksson A, Rosenberg J, Bisgaard T (2014) Surgical treatment for giant incisional hernia: a qualitative systematic review. Hernia 18(1):31–38. https://doi.org/10.1007/s10029-013-1066-y
Blair LJ, Ross SW, Huntington CR et al (2015) Computed tomographic measurements predict component separation in ventral hernia repair. J Surg Res 199(2):420–427. https://doi.org/10.1016/j.jss.2015.06.033
Sabbagh C, Dumont F, Robert B, Badaoui R, Verhaeghe P, Regimbeau JM (2011) Peritoneal volume is predictive of tension-free fascia closure of large incisional hernias with loss of domain: a prospective study. Hernia 15(5):559–565. https://doi.org/10.1007/s10029-011-0832-y
Love MW, Warren JA, Davis S et al (2021) Computed tomography imaging in ventral hernia repair: can we predict the need for myofascial release? Hernia 25(2):471–477. https://doi.org/10.1007/s10029-020-02181-y
Novak J, Jacisko J, Busch A et al (2021) Intra-abdominal pressure correlates with abdominal wall tension during clinical evaluation tests. Clin Biomech (Bristol, Avon) 88:105426. https://doi.org/10.1016/j.clinbiomech.2021.105426
Liang Y, Xu L, Tang W (2014) Interpretation of the international guidelines for definition and clinical management of intra-abdominal hypertension and abdominal compartment syndrome in children, 2013. Zhonghua wei zhong bing ji jiu yi xue 26(7):454–457. https://doi.org/10.3760/cma.j.issn.2095-4352.2014.07.002
Biltz NK, Collins KH, Shen KC, Schwartz K, Harris CA, Meyer GA (2020) Infiltration of intramuscular adipose tissue impairs skeletal muscle contraction. J Physiol 598(13):2669–2683. https://doi.org/10.1113/JP279595
Lee MJ, Kim HK, Kim EH et al (2021) Association between muscle quality measured by abdominal computed tomography and subclinical coronary atherosclerosis. Arterioscler Thromb Vasc Biol 41(2):e128–e140. https://doi.org/10.1161/ATVBAHA.120.315054
Muysoms FE, Miserez M, Berrevoet F et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414. https://doi.org/10.1007/s10029-009-0518-x
Young CS, Lyo V, Harris HW (2020) Fasical defect size predicts recurrence following incisional hernia repair: a 7-year, single-surgeon experience. Int J Abdom Wall Hernia Surg 3:11–17
Franklin BR, Patel KM, Nahabedian MY, Baldassari LE, Cohen EI, Bhanot P (2013) Predicting abdominal closure after component separation for complex ventral hernias: maximizing the use of preoperative computed tomography. Ann Plast Surg 71(3):261–265. https://doi.org/10.1097/SAP.0b013e3182773915
Smith JR, Kyriakakis R, Pressler MP et al (2022) BMI: does it predict the need for component separation? Hernia. https://doi.org/10.1007/s10029-022-02596-9
Christy MR, Apostolides J, Rodriguez ED, Manson PN, Gens D, Scalea T (2012) The component separation index: a standardized biometric identity in abdominal wall reconstruction. Eplasty 12:e17
Blaser AR, Björck M, De Keulenaer B, Regli A (2015) Abdominal compliance: a bench-to-bedside review. J Trauma Acute Care Surg 78(5):1044–1053. https://doi.org/10.1097/TA.0000000000000616
Tanaka EY, Yoo JH, Rodrigues AJ Jr, Utiyama EM, Birolini D, Rasslan S (2010) A computerized tomography scan method for calculating the hernia sac and abdominal cavity volume in complex large incisional hernia with loss of domain. Hernia 14(1):63–69. https://doi.org/10.1007/s10029-009-0560-8
DuBay DA, Choi W, Urbanchek MG et al (2007) Incisional herniation induces decreased abdominal wall compliance via oblique muscle atrophy and fibrosis. Ann Surg 245(1):140–146. https://doi.org/10.1097/01.sla.0000251267.11012.85
Zullo A, Fleckenstein J, Schleip R, Hoppe K, Wearing S, Klingler W (2020) Structural and functional changes in the coupling of fascial tissue, skeletal muscle, and nerves during aging. Front Physiol 11:592. https://doi.org/10.3389/fphys.2020.00592
Shahait AD, Alghanem L, Cmorej P et al (2021) Postoperative outcomes of ventral hernia repair in veterans. Surgery 169(3):603–609. https://doi.org/10.1016/j.surg.2020.09.003
Nieto EP, Ponz CB, Ananin SF, Vazquez EB (2020) Obesity as a risk factor for complications and recurrences after ventral hernia repair. Int J Abdom Wall Hernia Surg 3:1–3
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All the authors (Xuechao Du, Cuihong Jin, Yuchang Yan, Pengtao Sun, Yingmo Shen, Zhenyu Pan, Tao Jiang) report no conflicts of interest.
Ethical approval
This study was approved by the Ethics Committee of Beijing Chaoyang Hospital, Capital Medical University.
Human and animal rights
No animal experiments were performed in this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of our institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
This retrospective study only involved analysis of de-identified data, so informed consent was waived by the Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Du, X., Jin, C., Yan, Y. et al. CT-measured hernia parameters can predict component separation: a cross-sectional study from China. Hernia 27, 979–986 (2023). https://doi.org/10.1007/s10029-023-02761-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02761-8