Abstract
Purpose
Increasingly, radiologic imaging is obtained as part of the pathway in diagnosing ventral hernias. Often, radiologists receive incomplete or incorrect clinical information from clinicians. Objective: The aim of the study is to determine if clinical exam findings alter radiological interpretation of ventral hernias on CT.
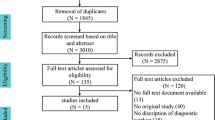
Methods
This is a single-institution double-blind, randomized trial. All patients with a recent abdominal/pelvic CT scan seen in various surgical clinics were enrolled. A surgeon blinded to the CT scan findings performed a standardized physical examination and assessed for the presence of a ventral hernia. Seven independent radiologists blinded to the study design reviewed the scans. Each radiologist received one of three types of clinical exam data per CT: accurate (correct), inaccurate (purposely incorrect), or none. Allocation was random and stratified by the presence of clinical hernia. The primary outcome was the proportion of radiologic hernias detected, analyzed by chi square.
Results
115 patients were enrolled for a total of 805 CT scan reads. The proportion of hernias detected differed by up to 25% depending on if accurate, no, or inaccurate clinical information was provided. Inaccurate clinical data in patients with no hernia on physical exam led to a significant difference in the radiologic hernia detection rate (54.3% versus 35.7%, p = 0.007). No clinical data in patients with a hernia on physical exam led to a lower radiologic hernia detection rate (75.0% versus 93.8%, p = 0.001).
Conclusions
The presence and accuracy of clinical information provided to radiologists impacts the diagnosis of abdominal wall hernias in up to 25% of cases. Standardization of both clinical and radiologic examinations for hernias and their reporting are needed.
Trial registration
Clinicaltrials.gov, Number NCT03121131, https://clinicaltrials.gov/ct2/show/NCT03121131.

Similar content being viewed by others
References
Berdahl CT, Vermeulen MJ, Larson DB, Schull MJ (2013) Emergency department computed tomography utilization in the United States and Canada. Ann Emerg Med 62(5):486–496
Chin JY, Goldstraw E, Lunniss P, Patel K (2012) Evaluation of the utility of abdominal CT scans in the diagnosis, management, outcome and information given at discharge of patients with non-traumatic acute abdominal pain. Br J Radiol 85(1017):e596–e602
Khalilzadeh O, Rahimian M, Batchu V, Vadvala HV, Novelline RA, Choy G (2015) Effectiveness of second-opinion radiology consultations to reassess the cervical spine CT scans: a study on trauma patients referred to a tertiary-care hospital. Diagn Interv Radiol 21(5):423–427
Zen E, Yousem DM, Carone M, Lewin JS (2010) Second-opinion consultations in neuroradiology. Radiology 255(1):135–141
Cheng T, Dumire R, Golden S, Gregory J (2013) Impact on patient care of discordance in radiology readings between external overnight radiology services and staff radiology readings at a level 1 trauma center. Am J Surg 205(3):280–282
Eakins C, Ellis WD, Pruthi S et al (2012) Second opinion interpretations by specialty radiologists at a pediatric hospital: rate of disagreement and clinical implications. AJR Am J Roentgenol 199(4):916–920
CNN (2008) Radiologists read scans better if they have patient’s photo. http://www.cnn.com/2008/HEALTH/12/02/healthmag.scan.photo/index.html?iref=newssearch. Accessed Feb 2017
Grady AT, Sosa JA, Tanpitukpongse TP, Choudhury KR, Gupta RT, Hoang JK (2015) Radiology reports for incidental thyroid nodules on CT and MRI: high variability across subspecialties. AJNR Am J Neuroradiol 36(2):397–402
Alexander K (2010) Reducing error in radiographic interpretation. Can Vet J 51(5):533–536
Doubilet P, Herman PG (1981) Interpretation of radiographs: effect of clinical history. AJR Am J Roentgenol 137(5):1055–1058
ClinicalTrials.gov. (2017) https://clinicaltrials.gov/. Accessed Jan 2017
Enhancing the Quality and Transparency of Health Research (2010) Equator network. http://www.equator-network.org/reporting-guidelines/consort/. Accessed Mar 2017
Holihan JL, Flores-Gonzalez JR, Mo J, Ko TC, Kao LS, Liang MK (2017) A prospective assessment of clinical and patient-reported outcomes of initial non-operative management of ventral hernias. World J Surg 41(5):1267–1273
Holihan JL, Karanjawala B, Ko A et al (2016) Use of computed tomography in diagnosing ventral hernia recurrence: a blinded, prospective, multispecialty evaluation. JAMA Surg 151(1):7–13
Kohavi R, Provost F (1998) Glossary of terms. Mach Learn 30(2/3):271–274
Brady A, Laoide RO, McCarthy P, McDermott R (2012) Discrepancy and error in radiology: concepts, causes and consequences. Ulster Med J 81(1):3–9
Tillack AA, Borgstede JP (2013) An evaluation of the impact of clinically embedded reading rooms on radiologist-referring clinician communication. J Am Colloid Radiol 10(5):368–372
Welch HG, Prorok PC, O’Malley AJ, Kramer BS (2016) Breast-cancer tumor size, overdiagnosis, and mammography screening effectiveness. N Engl J Med 375(15):1438–1447
Renfrew DL, Franken EA, Berbaum KS et al (1992) Error in radiology: classification and lessons in 182 cases presented at a problem case conference. Radiology 183(1):145–150
Goodenough CJ, Ko TC, Kao LS et al (2015) Development and validation of a risk stratification score for ventral incisional hernia after abdominal surgery: hernia expectation rates in intra-abdominal surgery (the HERNIA Project). J AM Colloid Surg 220(4):405–413 (Epub 2015 Jan 2)
Nardi M Jr., Millo P, Brachet Contul R et al (2017) Laparoscopic ventral hernia repair with composite mesh: analysis of risk factors for recurrence in 185 patients with 5 years follow-up. Int J Surg 40:38–44 (Epub ahead of print)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest or anything to disclose. DC: declares no conflict of interest. KB: declares no conflict of interest. KB: declares no conflict of interest. SC: declares no conflict of interest. JH: declares no conflict of interest. LK: declares no conflict of interest. TK: declares no conflict of interest. EM: declares no conflict of interest. MM: declares no conflict of interest. KS: declares no conflict of interest. VS: declares no conflict of interest. VT: declares no conflict of interest. CV: declares no conflict of interest. ML: declares no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This experiments complies with the current laws of the United States on medical research.
Informed consent
With institutional review board oversight and approval, all patients received a written consent of participation, however, for participating radiologists a written consent was waived. Radiologist received a letter of information explaining the broadscope of the project, voluntary nature of participation, risks and benefits, and contact information in the event of questions or to withdraw from the study.
Additional information
Meeting presentations
The associated manuscript was presented at the American College of Surgeons 2017 Clinical Congress (San Diego, California; October, 2017).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cherla, D.V., Bernardi, K., Blair, K.J. et al. Importance of the physical exam: double-blind randomized controlled trial of radiologic interpretation of ventral hernias after selective clinical information. Hernia 23, 987–994 (2019). https://doi.org/10.1007/s10029-018-1856-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1856-3