Abstract
Purpose
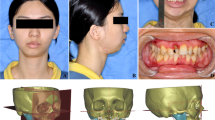
Temporomandibular joint ankylosis (TMJA) in children is associated with retrognathia, reduction in pharyngeal airway volume (PAV), and obstructive sleep apnea (OSA). Distraction-osteogenesis (DO) is the proven method in the management of OSA. There is paucity in literature about the effect of distraction vector on PAV. It can be expected that an oblique vector would improve PAV and relieve OSA. Thus, the study was designed to explore the feasibility, advantages, and disadvantages of this modified technique for managing TMJA and OSA simultaneously.
Materials and method
The investigators designed a prospective study on patients of TMJA with retrognathia. Ethical approval was obtained (IECPG-547/14.11.2018). In all patients, simultaneous ankylosis release and mandibular distraction were performed. Primary outcome variables were improvement in 3-dimensional (3D) PAV and maximal interincisal opening (MIO). Secondary outcome variables were changed mandibular length, distraction relapse, and re-ankylosis. Paired t-test and multivariate ANOVA were used to assess all the parameters.
Result
The study included 13 joints in 8 patients of TMJA with retrognathia (2 unilateral and 6 bilateral ankylosis) with mean age of 14.25 ± 7.37 years. Mean distraction performed was 19 ± 4.0 mm. There was a statistically significant improvement of PAV by 225% (p = 0.002), a reduction in Epworth’s scale (p = 0.017), an increase in MIO (p = 0.001), and an increase in mandibular length. Three patients had re-ankylosis at the 25-month follow-up.
Conclusion
The results of the present study conclude that modification of distraction vector improves 3D PAV and MIO in TMJA patients, with the added advantage of a reduction in overall treatment time and improved patient compliance.
Graphical Abstract







Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Andrade NN, Mathai PC, Ganapathy S et al (2018) Pre-arthroplastic mandibular distraction osteogenesis for the correction of OSA in TMJ ankylosis: a prospective observational study of 25 cases. Oral Maxillofac Surg 22:409–418. https://doi.org/10.1007/s10006-018-0722-x
Anantanarayanan P, Narayanan V, Manikandhan R, Kumar D (2008) Primary mandibular distraction for management of nocturnal desaturations secondary to temporomandibular joint (TMJ) ankylosis. Int J Pediat Otorhinolaryngol 72:385–389. https://doi.org/10.1016/j.ijporl.2007.11.015
Andrade NN, Raikwar KR (2009) Management of patients with obstructive sleep apnoea induced by temporomandibular joint ankylosis: a novel 2-stage surgical protocol and report of 5 cases. Asian J Oral Maxillofac Surg 21:27–32. https://doi.org/10.1016/S0915-6992(09)80017-4
Kwon T-G, Park H-S, Kim J-B, Shin H-I (2006) Staged surgical treatment for temporomandibular joint ankylosis: intraoral distraction after temporalis muscle flap reconstruction. J Oral Maxillofac Surg 64:1680–1683. https://doi.org/10.1016/j.joms.2006.03.029
Andrade NN, Kalra R, Shetye SP (2012) New protocol to prevent TMJ reankylosis and potentially life-threatening complications in triad patients. Int J Oral Maxillofac Surg 41:1495–1500. https://doi.org/10.1016/j.ijom.2012.06.012
Ma Y, Huang Y, Zhu S, Li Y (2019) Simultaneous arthroplasty and distraction osteogenesis for the treatment of ankylosis of the temporomandibular joint and secondary mandibular deformities in children. Br J Oral Maxillofac Surg 57:135–139. https://doi.org/10.1016/j.bjoms.2018.11.016
Dean A, Alamillos F (1999) Mandibular distraction in temporomandibular joint ankylosis. Plast Reconstr Surg 104:2021–2031. https://doi.org/10.1097/00006534-199912000-00012
Papageorge MB, Apostolidis C (1999) Simultaneous mandibular distraction and arthroplasty in a patient with temporomandibular joint ankylosis and mandibular hypoplasia. J Oral Maxillofac Surg 57:328–333. https://doi.org/10.1016/S0278-2391(99)90683-3
Riley R, Guilleminault C, Powell N, Simmons FB (1985) Palatopharyngoplasty failure, cephalometric roentgenograms, and obstructive sleep apnea. Otolaryngol Head Neck Surg 93:240–244. https://doi.org/10.1177/019459988509300222
Pirila-Parkkinen K, Lopponen H, Nieminen P et al (2010) Cephalometric evaluation of children with nocturnal sleep-disordered breathing. Eur J Orthod 32:662–671. https://doi.org/10.1093/ejo/cjp162
Aksu M, Gorucu-Coskuner H, Taner T (2017) Assessment of upper airway size after orthopedic treatment for maxillary protrusion or mandibular retrusion. Am J Orthod Dentofac Orthop 152:364–370. https://doi.org/10.1016/j.ajodo.2016.12.027
Kaban LB, Bouchard C, Troulis MJ (2009) A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg 67:1966–1978. https://doi.org/10.1016/j.joms.2009.03.071
Roychoudhury A, Parkash H, Trikha A (1999) Functional restoration by gap arthroplasty in temporomandibular joint ankylosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87:166–169. https://doi.org/10.1016/S1079-2104(99)70267-2
Bi RY, Luo XT, Jiang N et al (2018) Change in the posterior airway after mandibular distraction osteogenesis in patients with ankylosis of the temporomandibular joint: a retrospective study. Br J Oral Maxillofac Surg 56:525–530. https://doi.org/10.1016/j.bjoms.2018.05.010
Kaur K, Roychoudhury A, Bhutia O et al (2020) Evaluation of success of transport disc distraction osteogenesis and costochondral graft for ramus condyle unit reconstruction in pediatric temporomandibular joint ankylosis. J Oral Maxillofac Surg 78:1018.e1-1018.e16. https://doi.org/10.1016/j.joms.2020.01.029
Yadav R, Bhutia O, Shukla G, Roychoudhury A (2014) Distraction osteogenesis for management of obstructive sleep apnoea in temporomandibular joint ankylosis patients before the release of joint. J Craniomaxillofac Surg 42:588–594. https://doi.org/10.1016/j.jcms.2013.07.031
Rachmiel A, Aizenbud D, Pillar G et al (2005) Bilateral mandibular distraction for patients with compromised airway analyzed by three-dimensional CT. Int J Oral Maxillofac Surg 34:9–18. https://doi.org/10.1016/j.ijom.2004.05.010
Zellner EG, Mhlaba JM, Reid RR, Steinbacher DM (2017) Does mandibular distraction vector influence airway volumes and outcome? J Oral Maxillofac Surg 75:167–177. https://doi.org/10.1016/j.joms.2016.07.034
Rao K, Kumar S, Kumar V et al (2004) The role of simultaneous gap arthroplasty and distraction osteogenesis in the management of temporo-mandibular joint ankylosis with mandibular deformity in children. J Craniomaxillofac Surg 32:38–42. https://doi.org/10.1016/j.jcms.2003.07.003
Chellappa AL, Mehrotra D, Vishwakarma K et al (2015) Pre-arthroplastic and simultaneous mandibular distraction for correction of facial deformity in temporomandibular joint ankylosis. J Oral Biol Craniofac Res 5:153–160. https://doi.org/10.1016/j.jobcr.2015.06.003
Pogrel MA, Kaban LB (1990) The role of a temporalis fascia and muscle flap in temporomandibular joint surgery. J Oral Maxillofac Surg 48:14–19. https://doi.org/10.1016/0278-2391(90)90173-Y
Umeda H, Kaban LB, Anthony Pogrel M, Stern M (1993) Long-term viability of the temporalis muscle/fascia flap used for temporomandibular joint reconstruction. J Oral Maxillofac Surg 51:530–533. https://doi.org/10.1016/S0278-2391(10)80509-9
Kohli S, Mohanty S, Singh S et al (2017) The autogenous graft versus transport distraction osteogenesis for reconstruction of the ramus–condyle unit: a prospective comparative study. Int J Oral Maxillofac Surg 46:1106–1117. https://doi.org/10.1016/j.ijom.2017.03.022
Xia L, Zhang Y, An J et al (2020) Evaluating the remodeling of condyles reconstructed by transport distraction osteogenesis in the treatment of temporomandibular joint ankylosis. J Craniomaxillofac Surg 48:494–500. https://doi.org/10.1016/j.jcms.2020.03.004
Zhang C, Li Y, Ye B et al (2017) Application of bidirectional distraction osteogenesis for the treatment of mandibular micriognathia caused by temporomandibular joint ankylosis. J Craniofac Surg 28:1502–1507. https://doi.org/10.1097/SCS.0000000000003750
Chen J, Liu Y, Ping F et al (2010) Two-step transport-disk distraction osteogenesis in reconstruction of mandibular defect involving body and ramus. Int J Oral Maxillofac Surg 39:573–579. https://doi.org/10.1016/j.ijom.2010.03.021
Sharma A, Paeng J-Y, Yamada T, Kwon T-G (2016) Simultaneous gap arthroplasty and intraoral distraction and secondary contouring surgery for unilateral temporomandibular joint ankylosis. Maxillofac Plast Reconstr Surg 38:12. https://doi.org/10.1186/s40902-016-0058-0
Bansal V, Singh S, Garg N, Dubey P (2014) Transport distraction osteogenesis as a method of reconstruction of the temporomandibular joint following gap arthroplasty for post-traumatic ankylosis in children: a clinical and radiological prospective assessment of outcome. Int J Oral Maxillofac Surg 43:227–236. https://doi.org/10.1016/j.ijom.2013.07.745
Liang C, Wang X, Yi B et al (2007) Clinical study of simultaneous correction of unilateral temporomandibular joint ankylosis and mandibular micrognathia with internal distraction osteogenesis. Beijing Da Xue Xue Bao Yi Xue Ban 39:33–36
Giraddi G, Arora K, Sai Anusha A (2016) Distraction osteogenesis in the treatment of temporomandibular joint ankylosis with mandibular micrognathia. Ann Maxillofac Surg 6:68. https://doi.org/10.4103/2231-0746.186125
Xu J, Long X, Cheng AH et al (2015) Modified condylar distraction osteogenesis via single preauricular incision for treatment of temporomandibular joint ankylosis: The. J Craniofac Surg 26:509–511. https://doi.org/10.1097/SCS.0000000000001291
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Hetal Amipara. The first draft of the manuscript was written by Hetal Amipara and Jithin Sasikumar Puthukkudiyil. All authors Ongkila Bhutia, Ajoy Roychoudhury, Rahul Yadav, and Devalina Goswami commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institute Ethics committee (Ref no: IECPG-547/14.11.2018).
Consent to participate
Informed written consent was obtained from all patients before the procedure.
Consent for publication
Informed written consent was obtained from the patient.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Amipara, H., Puthukkudiyil, J.S., Bhutia, O. et al. How does changing the vector of transport disc distraction affect the outcomes of surgery in patients of temporomandibular joint ankylosis with obstructive sleep apnea?. Oral Maxillofac Surg 28, 235–244 (2024). https://doi.org/10.1007/s10006-022-01133-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-022-01133-3