Abstract
Aim
To investigate the effects of low-level laser therapy (LLLT) as an adjunct to non-surgical periodontal treatment (NSPT) on the plasminogen-activating system.
Materials and Methods
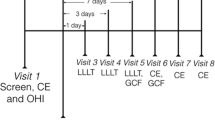
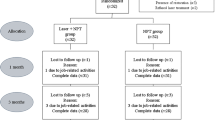
Stage 3–4 Grade C periodontitis and age-gender-matched healthy individuals participated in the split-mouth study (ClinicalTrials.gov identifier, NCT05233501). The study groups were Periodontitis/NSPT (Sham); Periodontitis/NSPT + LLLT (LLLT); Healthy (Control). Following NSPT, LLLT was applied on Days 0, 2 and 7. Clinical parameters were recorded at baseline and on Day 30. Gingival crevicular fluid (GCF) was collected at baseline, on days 7, 14, and 30; tissue-type plasminogen activator (tPA) and plasminogen activator inhibitor-1 (PAI-1) levels were measured with ELISA.
Results
Clinical parameters, total GCF tPA (tPAt) and PAI-1 (PAI-1t) levels significantly reduced in LLLT and Sham groups (< 0.001). GCF tPAt levels in LLLT were significantly lower (< 0.05) than Sham on Day 7. GCF tPAt levels in periodontitis groups were significantly higher than the Control at baseline, on Days 7 and 14 (< 0.01). By Day 30, both groups decreased to control levels (> 0.05). GCF PAI-1t levels were significantly lower in LLLT than the Sham on day 30 (< 0.01), comparable to healthy controls (> 0.05).
Conclusion
Adjunctive LLLT modulates the plasminogen activating system in severe periodontitis by altering GCF tPA and PAI-1 levels.
Clinical relevance
LLLT as an adjunct to non-surgical periodontal treatment in patients with Stage 3–4 Grade C leads to reduced plasminogen activation.


Similar content being viewed by others
Data Availability
N/A.
References
Manresa C, Sanz-Miralles EC, Twigg J, Bravo M (2018) Supportive periodontal therapy (SPT) for maintaining the dentition in adults treated for periodontitis. Cochrane Database Syst Rev 1:CD009376. https://doi.org/10.1002/14651858.CD009376.pub2
Sanz I, Alonso B, Carasol M, Herrera D, Sanz M (2012) Nonsurgical treatment of periodontitis. J Evid Based Dent Pract 12:76–86. https://doi.org/10.1016/S1532-3382(12)70019-2
Umeda M, Takeuchi Y, Noguchi K, Huang Y, Koshy G, Ishikawa I (2004) Effects of nonsurgical periodontal therapy on the microbiota. Periodontol 2000 36:98–120. https://doi.org/10.1111/j.1600-0757.2004.03675.x
Keestra JA, Grosjean I, Coucke W, Quirynen M, Teughels W (2015) Non-surgical periodontal therapy with systemic antibiotics in patients with untreated aggressive periodontitis: a systematic review and meta-analysis. J Periodontal Res 50:689–706. https://doi.org/10.1111/jre.12252
Belibasakis GN, Belstrom D, Eick S, Gursoy UK, Johansson A, Kononen E (2023) Periodontal microbiology and microbial etiology of periodontal diseases: Historical concepts and contemporary perspectives. Periodontol 2000. https://doi.org/10.1111/prd.12473
Sedghi L, DiMassa V, Harrington A, Lynch SV, Kapila YL (2021) The oral microbiome: Role of key organisms and complex networks in oral health and disease. Periodontol 2000 87:107–131. https://doi.org/10.1111/prd.12393
Joseph S, Curtis MA (2021) Microbial transitions from health to disease. Periodontol 2000 86:201–209. https://doi.org/10.1111/prd.12377
Teughels W, Dhondt R, Dekeyser C, Quirynen M (2014) Treatment of aggressive periodontitis. Periodontol 2000 65:107–133. https://doi.org/10.1111/prd.12020
Darveau RP, Curtis MA (2021) Oral biofilms revisited: A novel host tissue of bacteriological origin. Periodontol 2000 86:8–13. https://doi.org/10.1111/prd.12374
Sgolastra F, Petrucci A, Gatto R, Monaco A (2012) Effectiveness of systemic amoxicillin/metronidazole as an adjunctive therapy to full-mouth scaling and root planing in the treatment of aggressive periodontitis: a systematic review and meta-analysis. J Periodontol 83:731–743. https://doi.org/10.1902/jop.2011.110432
Rabelo CC, Feres M, Goncalves C, Figueiredo LC, Faveri M, Tu YK, Chambrone L (2015) Systemic antibiotics in the treatment of aggressive periodontitis. A systematic review and a Bayesian Network meta-analysis. J Clin Periodontol 42:647–657. https://doi.org/10.1111/jcpe.12427
Herrera D, van Winkelhoff AJ, Matesanz P, Lauwens K, Teughels W (2023) Europe's contribution to the evaluation of the use of systemic antimicrobials in the treatment of periodontitis. Periodontol 2000. https://doi.org/10.1111/prd.12492
Calderin S, Garcia-Nunez JA, Gomez C (2013) Short-term clinical and osteoimmunological effects of scaling and root planing complemented by simple or repeated laser phototherapy in chronic periodontitis. Lasers Med Sci 28:157–166. https://doi.org/10.1007/s10103-012-1104-5
Meimandi M, TalebiArdakani MR, EsmaeilNejad A, Yousefnejad P, Saebi K, Tayeed MH (2017) The Effect of Photodynamic Therapy in the Treatment of Chronic Periodontitis: A Review of Literature. J Lasers Med Sci 8:S7–S11. https://doi.org/10.15171/jlms.2017.s2
Grzech-Lesniak K, Matys J, Dominiak M (2018) Comparison of the clinical and microbiological effects of antibiotic therapy in periodontal pockets following laser treatment: An in vivo study. Adv Clin Exp Med 27:1263–1270. https://doi.org/10.17219/acem/70413
Schwarz F, Aoki A, Becker J, Sculean A (2008) Laser application in non-surgical periodontal therapy: a systematic review. J Clin Periodontol 35:29–44. https://doi.org/10.1111/j.1600-051X.2008.01259.x
Ren C, McGrath C, Jin L, Zhang C, Yang Y (2017) The effectiveness of low-level laser therapy as an adjunct to non-surgical periodontal treatment: a meta-analysis. J Periodontal Res 52:8–20. https://doi.org/10.1111/jre.12361
Qadri T, Miranda L, Tuner J, Gustafsson A (2005) The short-term effects of low-level lasers as adjunct therapy in the treatment of periodontal inflammation. J Clin Periodontol 32:714–719. https://doi.org/10.1111/j.1600-051X.2005.00749.x
Aykol G, Baser U, Maden I, Kazak Z, Onan U, Tanrikulu-Kucuk S, Ademoglu E, Issever H, Yalcin F (2011) The effect of low-level laser therapy as an adjunct to non-surgical periodontal treatment. J Periodontol 82:481–488. https://doi.org/10.1902/jop.2010.100195
Lai SM, Zee KY, Lai MK, Corbet EF (2009) Clinical and radiographic investigation of the adjunctive effects of a low-power He-Ne laser in the treatment of moderate to advanced periodontal disease: a pilot study. Photomed Laser Surg 27:287–293. https://doi.org/10.1089/pho.2007.2206
Takasaki AA, Aoki A, Mizutani K, Schwarz F, Sculean A, Wang CY, Koshy G, Romanos G, Ishikawa I, Izumi Y (2009) Application of antimicrobial photodynamic therapy in periodontal and peri-implant diseases. Periodontol 2000 51:109–40. https://doi.org/10.1111/j.1600-0757.2009.00302.x
Kurgan S, Onder C, Balci N, Fentoglu O, Eser F, Balseven M, Serdar MA, Tatakis DN, Gunhan M (2017) Gingival crevicular fluid tissue/blood vessel-type plasminogen activator and plasminogen activator inhibitor-2 levels in patients with rheumatoid arthritis: effects of nonsurgical periodontal therapy. J Periodontal Res 52:574–581. https://doi.org/10.1111/jre.12425
Toyman U, Tuter G, Kurtis B, Kivrak E, Bozkurt S, Yucel AA, Serdar M (2015) Evaluation of gingival crevicular fluid levels of tissue plasminogen activator, plasminogen activator inhibitor 2, matrix metalloproteinase-3 and interleukin 1-beta in patients with different periodontal diseases. J Periodontal Res 50:44–51. https://doi.org/10.1111/jre.12179
Sarajlic J, Agis H, Kandler B, Watzek G, Gruber R (2007) Plasminogen activation by fibroblasts from periodontal ligament and gingiva is not directly affected by chemokines in vitro. Arch Oral Biol 52:663–668. https://doi.org/10.1016/j.archoralbio.2006.12.020
Schmid J, Cohen RL, Chambers DA (1991) Plasminogen activator in human periodontal health and disease. Arch Oral Biol 36:245–250. https://doi.org/10.1016/0003-9969(91)90093-a
Wyganowska-Swiatkowska M, Surdacka A, Skrzypczak-Jankun E, Jankun J (2014) The plasminogen activation system in periodontal tissue (Review). Int J Mol Med 33:763–768. https://doi.org/10.3892/ijmm.2014.1653
Kinnby B (2002) The plasminogen activating system in periodontal health and disease. Biol Chem 383:85–92. https://doi.org/10.1515/BC.2002.008
Armitage GC (1999) Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4:1–6. https://doi.org/10.1902/annals.1999.4.1.1
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS (2018) Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol 89(Suppl 1):S173–S182. https://doi.org/10.1002/JPER.17-0721
Kanmaz B, Lappin DF, Nile CJ, Buduneli N (2020) Effects of smoking on non-surgical periodontal therapy in patients with periodontitis Stage III or IV, and Grade C. J Periodontol 91:442–453. https://doi.org/10.1002/JPER.19-0141
Aoki A, Mizutani K, Schwarz F, Sculean A, Yukna RA, Takasaki AA, Romanos GE, Taniguchi Y, Sasaki KM, Zeredo JL, Koshy G, Coluzzi DJ, White JM, Abiko Y, Ishikawa I, Izumi Y (2015) Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000 68:217–69. https://doi.org/10.1111/prd.12080
Silness J, Loe H (1964) Periodontal disease in pregnancy. Ii. correlation between oral hygiene and periodontal condtion. Acta Odontol Scand 22:121–135. https://doi.org/10.3109/00016356408993968
Loe H, Silness J (1963) Periodontal disease in pregnancy. I prevalence and severity. Acta Odontol Scand 21:533–551. https://doi.org/10.3109/00016356309011240
Curtis MA, Griffiths GS, Price SJ, Coulthurst SK, Johnson NW (1988) The total protein concentration of gingival crevicular fluid. Variation with sampling time and gingival inflammation. J Clin Periodontol 15:628–632. https://doi.org/10.1111/j.1600-051x.1988.tb02263.x
Saglam M, Kantarci A, Dundar N, Hakki SS (2014) Clinical and biochemical effects of diode laser as an adjunct to nonsurgical treatment of chronic periodontitis: a randomized, controlled clinical trial. Lasers Med Sci 29:37–46. https://doi.org/10.1007/s10103-012-1230-0
Slot DE, Jorritsma KH, Cobb CM, Van der Weijden FA (2014) The effect of the thermal diode laser (wavelength 808–980 nm) in non-surgical periodontal therapy: a systematic review and meta-analysis. J Clin Periodontol 41:681–692. https://doi.org/10.1111/jcpe.12233
Dederich DN (2015) Little evidence for the use of diode lasers as an adjunct to non-surgical periodontal therapy. Evid Based Dent 16:16. https://doi.org/10.1038/sj.ebd.6401078
Mokeem S (2018) Efficacy of adjunctive low-level laser therapy in the treatment of aggressive periodontitis: A systematic review. J Investig Clin Dent 9:e12361. https://doi.org/10.1111/jicd.12361
Annaji S, Sarkar I, Rajan P, Pai J, Malagi S, Bharmappa R, Kamath V (2016) Efficacy of photodynamic therapy and lasers as an adjunct to scaling and root planing in the treatment of aggressive periodontitis - a clinical and microbiologic short term study. J Clin Diagn Res 10:ZC08-12. https://doi.org/10.7860/JCDR/2016/13844.7165
Kamma JJ, Vasdekis VG, Romanos GE (2009) The effect of diode laser (980 nm) treatment on aggressive periodontitis: evaluation of microbial and clinical parameters. Photomed Laser Surg 27:11–19. https://doi.org/10.1089/pho.2007.2233
Ertugrul AS, Tekin Y, Talmac AC (2017) Comparing the efficiency of Er, Cr:YSGG laser and diode laser on human beta-defensin-1 and IL-1beta levels during the treatment of generalized aggressive periodontitis and chronic periodontitis. J Cosmet Laser Ther 19:409–417. https://doi.org/10.1080/14764172.2017.1334923
Matarese G, Ramaglia L, Cicciu M, Cordasco G, Isola G (2017) The effects of diode laser therapy as an adjunct to scaling and root planing in the treatment of aggressive periodontitis: a 1-year randomized controlled clinical trial. Photomed Laser Surg 35:702–709. https://doi.org/10.1089/pho.2017.4288
Moreira AL, Novaes AB Jr, Grisi MF, Taba M Jr, Souza SL, Palioto DB, de Oliveira PG, Casati MZ, Casarin RC, Messora MR (2015) Antimicrobial photodynamic therapy as an adjunct to non-surgical treatment of aggressive periodontitis: a split-mouth randomized controlled trial. J Periodontol 86:376–386. https://doi.org/10.1902/jop.2014.140392
Borrajo JL, Varela LG, Castro GL, Rodriguez-Nunez I, Torreira MG (2004) Diode laser (980 nm) as adjunct to scaling and root planing. Photomed Laser Surg 22:509–512. https://doi.org/10.1089/pho.2004.22.509
Uitto VJ, Overall CM, McCulloch C (2003) Proteolytic host cell enzymes in gingival crevice fluid. Periodontol 2000 31:77–104. https://doi.org/10.1034/j.1600-0757.2003.03106.x
Olofsson A, Lindberg P, Lanke J, Matsson L, Kinnby B (2003) Relationship between fibrinolytic activity and gingival inflammatory reaction in young individuals. J Periodontal Res 38:104–108. https://doi.org/10.1034/j.1600-0765.2003.01370.x
Buduneli N, Buduneli E, Kardesler L, Lappin D, Kinane DF (2005) Plasminogen activator system in smokers and non-smokers with and without periodontal disease. J Clin Periodontol 32:417–424. https://doi.org/10.1111/j.1600-051X.2005.00694.x
Tuter G, Ozdemir B, Kurtis B, Serdar M, Yucel AA, Ayhan E (2013) Short term effects of non-surgical periodontal treatment on gingival crevicular fluid levels of tissue plasminogen activator (t-PA) and plasminogen activator inhibitor 2 (PAI-2) in patients with chronic and aggressive periodontitis. Arch Oral Biol 58:391–396. https://doi.org/10.1016/j.archoralbio.2012.08.008
Deppe H, Hohlweg-Majert B, Holzle F, Kesting MR, Wagenpfeil S, Wolff KD, Schmitt M (2010) Content of urokinase-type plasminogen activator (uPA) and its inhibitor PAI-1 in oral mucosa and inflamed periodontal tissue. Quintessence Int 41:165–171
Buduneli N, Buduneli E, Kutukculer N (2009) Interleukin-17, RANKL, and osteoprotegerin levels in gingival crevicular fluid from smoking and non-smoking patients with chronic periodontitis during initial periodontal treatment. J Periodontol 80:1274–1280. https://doi.org/10.1902/jop.2009.090106
Pamuk F, Lutfioglu M, Aydogdu A, Koyuncuoglu CZ, Cifcibasi E, Badur OS (2017) The effect of low-level laser therapy as an adjunct to non-surgical periodontal treatment on gingival crevicular fluid levels of transforming growth factor-beta 1, tissue plasminogen activator and plasminogen activator inhibitor 1 in smoking and non-smoking chronic periodontitis patients: A split-mouth, randomized control study. J Periodontal Res 52:872–882. https://doi.org/10.1111/jre.12457
Behle JH, Sedaghatfar MH, Demmer RT, Wolf DL, Celenti R, Kebschull M, Belusko PB, Herrera-Abreu M, Lalla E, Papapanou PN (2009) Heterogeneity of systemic inflammatory responses to periodontal therapy. J Clin Periodontol 36:287–294. https://doi.org/10.1111/j.1600-051X.2009.01382.x
Taylor B, Tofler G, Morel-Kopp MC, Carey H, Carter T, Elliott M, Dailey C, Villata L, Ward C, Woodward M, Schenck K (2010) The effect of initial treatment of periodontitis on systemic markers of inflammation and cardiovascular risk: a randomized controlled trial. Eur J Oral Sci 118:350–356. https://doi.org/10.1111/j.1600-0722.2010.00748.x
Bizzarro S, van der Velden U, ten Heggeler JM, Leivadaros E, Hoek FJ, Gerdes VE, Bakker SJ, Gans RO, Ten Cate H, Loos BG (2007) Periodontitis is characterized by elevated PAI-1 activity. J Clin Periodontol 34:574–580. https://doi.org/10.1111/j.1600-051X.2007.01095.x
Akman PT, Fentoglu O, Yilmaz G, Arpak N (2012) Serum plasminogen activator inhibitor-1 and tumor necrosis factor-alpha levels in obesity and periodontal disease. J Periodontol 83:1057–1062. https://doi.org/10.1902/jop.2011.110548
Ozawa Y, Shimizu N, Abiko Y (1997) Low-energy diode laser irradiation reduced plasminogen activator activity in human periodontal ligament cells. Lasers Surg Med 21:456–463. https://doi.org/10.1002/(sici)1096-9101(1997)21:5%3c456::aid-lsm7%3e3.0.co;2-p
Takema T, Yamaguchi M, Abiko Y (2000) Reduction of plasminogen activator activity stimulated by lipopolysaccharide from periodontal pathogen in human gingival fibroblasts by low-energy laser irradiation. Lasers Med Sci 15:35–42. https://doi.org/10.1007/s101030050045
Saglie FR, Marfany A, Camargo P (1988) Intragingival occurrence of Actinobacillus actinomycetemcomitans and Bacteroides gingivalis in active destructive periodontal lesions. J Periodontol 59:259–265. https://doi.org/10.1902/jop.1988.59.4.259
Sandros J, Papapanou PN, Nannmark U, Dahlen G (1994) Porphyromonas gingivalis invades human pocket epithelium in vitro. J Periodontal Res 29:62–69. https://doi.org/10.1111/j.1600-0765.1994.tb01092.x
Moritz A, Schoop U, Goharkhay K, Schauer P, Doertbudak O, Wernisch J, Sperr W (1998) Treatment of periodontal pockets with a diode laser. Lasers Surg Med 22:302–311. https://doi.org/10.1002/(sici)1096-9101(1998)22:5%3c302::aid-lsm7%3e3.0.co;2-t
Fleetwood AJ, O’Brien-Simpson NM, Veith PD, Lam RS, Achuthan A, Cook AD, Singleton W, Lund IK, Reynolds EC, Hamilton JA (2015) Porphyromonas gingivalis-derived RgpA-Kgp complex activates the macrophage urokinase plasminogen activator system: implications for periodontıtıs. J Biol Chem 290:16031–16042. https://doi.org/10.1074/jbc.M115.645572
Andreasen PA, Egelund R, Petersen HH (2000) The plasminogen activation system in tumor growth, invasion, and metastasis. Cell Mol Life Sci 57:25–40. https://doi.org/10.1007/s000180050497
Funding
This study was supported by the Scientific Research Fund of Beykent University (Grant/Award Number: 2018–19-BAP-05).
Author information
Authors and Affiliations
Contributions
Pamuk F prepared the manuscript and applied all treatment protocols. Lütfioğlu M prepared the manuscript and applied the statistical analysis and sample size calculation. Paksoy T prepared the manuscript and organised tables. Koyuncuoglu CZ performed all clinical measurements and GCF sampling. Polat NG performed ELISA. Cifcibasi E contributed to all ethical procedures and patient screening. Yildirim S organized the figures and organized data and the results. Kantarci A edited the manuscript and guided the study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The informed consent was obtained from study participants by written.
Competing interests
The authors declare no competing interests.
Conflict of interests
The authors report no conflict of interest related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pamuk, F., Lütfioğlu, M., Paksoy, T. et al. Impact of low-level laser therapy as an adjunct to non-surgical periodontal treatment on the levels of tissue plasminogen activator and plasminogen activator inhibitor 1 in Stage 3–4, Grade C periodontitis patients: a split-mouth, randomized control study. Clin Oral Invest 27, 6439–6449 (2023). https://doi.org/10.1007/s00784-023-05248-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05248-z