Abstract
Objectives
To evaluate the incorporation of halloysite nanotubes (HNTs) loaded with one of two calcium sources (i.e., calcium hydroxide/CaOH2 or beta-tricalcium phosphate/β-TCP) on the physicochemical and biological properties of an experimental resin-based dual-cured endodontic sealer.
Materials and methods
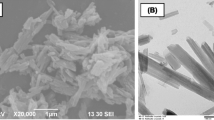
HNTs were encapsulated with CaOH2 or β-TCP at 10 wt.%. HNTs containing CaOH2 or β-TCP were added into the experimental sealers at 50 wt.%. The control sealers were the calcium-free HNT-modified resin-based experimental sealer and AH Plus™, a commercially available endodontic sealer. Degree of conversion, setting time, flow, film thickness, radiopacity, dimensional stability, and calcium ions release were determined. Antibiofilm properties and cytocompatibility of the formulated sealers and commercial control were also evaluated. One and two-way ANOVA analysis followed by Tukey’s post hoc test was conducted to evaluate the effect of the independent variable on the evaluated properties.
Results
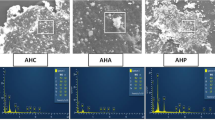
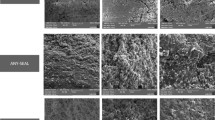
FTIR confirmed the encapsulation of calcium sources into HNTs. Regarding flow and film thickness, the values obtained from these sealers were in accordance with the specifications provided by ISO 6876. For radiopacity, AH Plus™ achieved the highest radiopacity (p<0.05). Among the experimental formulations, all experimental HNT-containing compositions exhibited values below 3 mm Al. The experimental sealers showed greater dimensional changes when compared to the commercial (AH Plus™) control. The release of calcium ions was observed for the HNT_CaOH2 and HNT_β-TCP sealers without statistical differences. Experimental sealers containing HNT_CaOH2 and HNT_β-TCP significantly reduced the CFU/mL count and showed cell compatibility.
Conclusions
The findings of this study demonstrate that the incorporation of HNT_CaOH2 or HNT_β-TCP into resin-based experimental sealers promoted antimicrobial effects and gradual calcium release without impairing cytocompatibility or physicochemical properties of the sealers. Still, an adjustment to reach the minimal radiopacity established by ISO 6876 is needed.
Clinical relevance
The experimental resin-based sealers seemed to be an alternative for endodontics. The incorporation of calcium sources exerts promising antimicrobial effects while displaying low cell toxicity.





Similar content being viewed by others
References
Adebayo ET, Ahaji LE, Nnachetta RN et al (2012) Technical quality of root canal fillings done in a Nigerian general dental clinic. BMC Oral Health 12:42. https://doi.org/10.1186/1472-6831-12-42
Ørstavik DAG (2005) Materials used for root canal obturation: technical, biological and clinical testing. Endod Top 12:25–38
Prada I, Micó-Muñoz P, Giner-Lluesma T et al (2019) Influence of microbiology on endodontic failure. Literature review. Med Oral Patol Oral Cir Bucal 24:e364–e372. https://doi.org/10.4317/medoral.22907
Tabassum S, Khan FR (2016) Failure of endodontic treatment: the usual suspects. Eur J Dent 10:144–147. https://doi.org/10.4103/1305-7456.175682
Liu D, Peng X, Wang S et al (2019) A novel antibacterial resin-based root canal sealer modified by Dimethylaminododecyl Methacrylate. Sci Rep 9:10632. https://doi.org/10.1038/s41598-019-47032-8
Baras BH, Wang S, Melo MAS et al (2019) Novel bioactive root canal sealer with antibiofilm and remineralization properties. J Dent 83:67–76. https://doi.org/10.1016/j.jdent.2019.02.006
Monteiro JC, Garcia IM, Leitune VCB et al (2019) Halloysite nanotubes loaded with alkyl trimethyl ammonium bromide as antibacterial agent for root canal sealers. Dent Mater 35:789–796. https://doi.org/10.1016/j.dental.2019.02.018
Estrela C, Gilson SB et al (1995) Mechanism of action of calcium and hydroxyl ions of calcium hydroxide on tissue and bacteria. Braz Dent J 6(2):85–90 http://143.107.206.201/bdj/t0262.html
Siqueira JF Jr, Lopes H (1999) Mechanisms of antimicrobial activity of calcium hydroxide: a critical review. Int Endod J 32:361–369
Louwakul P, Saelo A, Khemaleelakul S (2017) Efficacy of calcium oxide and calcium hydroxide nanoparticles on the elimination of Enterococcus faecalis in human root dentin. Clin Oral Investig 21:865–871. https://doi.org/10.1007/s00784-016-1836-x
Zaki DY, Zaazou MH, Khallaf ME, Hamdy TM (2018) In vivo comparative evaluation of periapical healing in response to a calcium silicate and calcium hydroxide based endodontic sealers. Open Access Maced J Med Sci 6:1475–1479. https://doi.org/10.3889/oamjms.2018.293
Lvov YM, Shchukin DG, Möhwald H, Price RR (2008) Halloysite clay nanotubes for controlled release of protective agents. ACS Nano 2:814–820. https://doi.org/10.1021/nn800259q
Kalagi S, Feitosa SA, Münchow EA et al (2020) Chlorhexidine-modified nanotubes and their effects on the polymerization and bonding performance of a dental adhesive. Dent Mater 36:687–697. https://doi.org/10.1016/j.dental.2020.03.007
Barot T, Rawtani D, Kulkarni P et al (2020) Physicochemical and biological assessment of flowable resin composites incorporated with farnesol loaded halloysite nanotubes for dental applications. J Mech Behav Biomed Mater 104:103675. https://doi.org/10.1016/J.JMBBM.2020.103675
Salmerón-Valdés EN, Cruz-Mondragón AC, Toral-Rizo VH et al (2022) Mechanical properties and antibacterial effect on mono-strain of Streptococcus mutans of orthodontic cements reinforced with chlorhexidine-modified nanotubes. Nanomaterials 12. https://doi.org/10.3390/nano12172891
Bordini EAF, Ferreira JA, Dubey N et al (2021) Injectable multifunctional drug delivery system for hard tissue regeneration under inflammatory microenvironments. ACS Appl Bio Mater. https://doi.org/10.1021/acsabm.1c00620
Bottino MC, Yassen GH, Platt JA et al (2015) A novel three-dimensional scaffold for regenerative endodontics: materials and biological characterizations. J Tissue Eng Regen Med 9:E116–E123. https://doi.org/10.1002/term.1712
Camargo CHR, Gomes LCL, França MCM et al (2019) Incorporating N-acetylcysteine and tricalcium phosphate into epoxy resin-based sealer improved its biocompatibility and adhesiveness to radicular dentine. Dent Mater 35:1750–1756
Garcia DC, Mingrone LE, de Sá MJC (2022) Evaluation of osseointegration and bone healing using pure-phase β - TCP ceramic implant in bone critical defects. A systematic review. Front Vet Sci 9
Herrera-González AM, Caldera-Villalobos M, Pérez-Mondragón AA et al (2019) Analysis of double bond conversion of photopolymerizable monomers by FTIR-ATR spectroscopy. J Chem Educ 96:1786–1789
Zeller DK, Fischer J, Rohr N (2021) Viscous behavior of resin composite cements. Dent Mater J 40:253–259. https://doi.org/10.4012/dmj.2019-313
Standardization IO for (2012) ISO 6876: 2012 Dentistry - Root canal sealing materials. International Organization for Standardization
Húngaro Duarte MA, de Oliveira El Kadre GD, Vivan RR et al (2009) Radiopacity of portland cement associated with different radiopacifying agents. J Endod 35:737–740. https://doi.org/10.1016/j.joen.2009.02.006
Carvalho-Junior JR, Correr-Sobrinho L, Correr AB et al (2007) Solubility and dimensional change after setting of root canal sealers: a proposal for smaller dimensions of test samples. J Endod 33:1110–1116. https://doi.org/10.1016/j.joen.2007.06.004
Standardization IO for, Standardization IO for (2009) ISO 10993-5: Biological evaluation of medical devices-Part 5: Tests for in vitro cytotoxicity
Mishra P, Sharma A, Mishra S, Gupta M (2017) Push-out bond strength of different endodontic obturation material at three different sites - In-vitro study. J Clin and Expe Dent 9:e733–e737. https://doi.org/10.4317/jced.53647
Michaud RA, Burgess J, Barfield RD et al (2008) Volumetric expansion of gutta-percha in contact with eugenol. J Endod 34:1528–1532
Rossetto DB, Fernandes SL, Cavenago BC et al (2014) Influence of the method in root canal filling using active lateral compaction techniques. Braz Dent J 25:295–301
Keçeci AD, Çelik Ünal G, Şen BH (2005) Comparison of cold lateral compaction and continuous wave of obturation techniques following manual or rotary instrumentation. Int Endod J 38:381–388
Chang H-H, Chang M-C, Wang H-H et al (2014) Urethane dimethacrylate induces cytotoxicity and regulates cyclooxygenase-2, hemeoxygenase and carboxylesterase expression in human dental pulp cells. Acta Biomater 10:722–731. https://doi.org/10.1016/j.actbio.2013.10.006
Atmeh AR, Hadis M, Camilleri J (2020) Real-time chemical analysis of root filling materials with heating: guidelines for safe temperature levels. Int Endod J 53:698–708
Mamootil K, Messer HH (2007) Penetration of dentinal tubules by endodontic sealer cements in extracted teeth and in vivo. Int Endod J 40:873–881. https://doi.org/10.1111/j.1365-2591.2007.01307.x
Leitune VCB, Takimi A, Collares FM et al (2013) Niobium pentoxide as a new filler for methacrylate-based root canal sealers. Int Endod J 46:205–210. https://doi.org/10.1111/j.1365-2591.2012.02107.x
Versiani MA, Carvalho-Junior JR, Padilha M et al (2006) A comparative study of physicochemical properties of AH PlusTM and EpiphanyTM root canal sealants. Int Endod J 39:464–471
Marciano MA, Guimarães BM, Amoroso-Silva P et al (2016) Physical and chemical properties and subcutaneous implantation of mineral trioxide aAggregate mixed with propylene glycol. J Endod 42:474–479. https://doi.org/10.1016/j.joen.2015.10.014
Siqueira JFJ, Rôças IN, Lopes HP, de Uzeda M (1999) Coronal leakage of two root canal sealers containing calcium hydroxide after exposure to human saliva. J Endod 25:14–16
Sinhal TM, Shah RRP, Jais PS et al (2018) An in vitro comparison and evaluation of sealing ability of newly introduced C-point system, cold lateral condensation, and thermoplasticized gutta-percha obturating technique: a dye extraction study. Contemp Clin Dent 9:164–169. https://doi.org/10.4103/ccd.ccd_722_17
Ferracane JL (2006) Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater 22:211–222. https://doi.org/10.1016/j.dental.2005.05.005
Hegde V, Arora S (2015) Sealing ability of a novel hydrophilic vs. conventional hydrophobic obturation systems: a bacterial leakage study. J Conserv Dent 18:62–65. https://doi.org/10.4103/0972-0707.148898
Camps J, Pommel L, Bukiet F, About I (2004) Influence of the powder/liquid ratio on the properties of zinc oxide–eugenol-based root canal sealers. Dent Mater 20:915–923
Reis LO, Kaizer MR, Ogliari FA et al (2014) Investigation on the use of triphenyl bismuth as radiopacifier for (di) methacrylate dental adhesives. Int J Adhes Adhes 48:80–84
Marins NH, Meereis CTW, Silva RM et al (2018) Radiopaque dental adhesive with addition of niobium pentoxide nanoparticles. Polym Bull 75:2301–2314
Zhu W, Liu F, He J (2018) Synthesis of radio-opaque methacrylate monomer and its application in visible light-curable dental resin. Adv Polym Technol 37:922–928
He J, Söderling E, Vallittu PK, Lassila LVJ (2013) Preparation and evaluation of dental resin with antibacterial and radio-opaque functions. Int J Mol Sci 14:5445–5460
Gandolfi MG, Siboni F, Botero T et al (2015) Calcium silicate and calcium hydroxide materials for pulp capping: biointeractivity, porosity, solubility and bioactivity of current formulations. J Appl Biomater Funct Mater 13:43–60
Duarte MAH, Midena RZ, Zeferino MA et al (2009) Evaluation of pH and calcium ion release of calcium hydroxide pastes containing different substances. J Endod 35:1274–1277. https://doi.org/10.1016/j.joen.2009.05.009
Peng W, Liu W, Zhai W et al (2011) Effect of tricalcium silicate on the proliferation and odontogenic differentiation of human dental pulp cells. J Endod 37:1240–1246. https://doi.org/10.1016/j.joen.2011.05.035
Shen Q, Sun J, Wu J et al (2010) An in vitro investigation of the mechanical-chemical and biological properties of calcium phosphate/calcium silicate/bismutite cement for dental pulp capping. J Biomed Mater Res Part B, Appl Biomater 94:141–148. https://doi.org/10.1002/jbm.b.31634
Holland R, de Souza V, Nery MJ et al (2002) Calcium salts deposition in rat connective tissue after the implantation of calcium hydroxide-containing sealers. J Endod 28:173–176. https://doi.org/10.1097/00004770-200203000-00007
Estrela C, de Araújo Estrela CR, Bammann LL, Pecora JD (2001) Two methods to evaluate the antimicrobial action of calcium hydroxide paste. J Endod 27:720–723. https://doi.org/10.1097/00004770-200112000-00002
Al-Dulaijan YA, Cheng L, Weir MD et al (2018) Novel rechargeable calcium phosphate nanocomposite with antibacterial activity to suppress biofilm acids and dental caries. J Dent 72:44–52
Wu J, Zhou C, Ruan J et al (2019) Self-healing adhesive with antibacterial activity in water-aging for 12 months. Dent Mater 35:1104–1116
Bhadila G, Baras BH, Weir MD et al (2020) Novel antibacterial calcium phosphate nanocomposite with long-term ion recharge and re-release to inhibit caries. Dent Mater J:2019–2203
Chandra S (2014) Grossman’s endodontic practice. Wolters kluwer india Pvt Ltd
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. Conceptualization: Xavier SR, Ribeiro JS. Data curation: Ribeiro JS, Xavier SR, Suárez CEC, Pappen FG. Formal analysis: Ribeiro JS, Xavier SR, Suárez CEC. Investigation: Ribeiro JS, Xavier SR, Suárez CEC. Methodology: Ribeiro JS, Xavier SR, Suárez CEC. Project administration: Ribeiro JS. Resources: Piva E, Lund RG, Bottino MC. Supervision: Lund RG, Bottino MC. Validation: Ribeiro JS. Visualization: Ribeiro JS, Pappen FG, Piva E. Writing—original draft: Ribeiro JS, Xavier SR, Suárez CEC. Writing—review and editing: Ribeiro JS, Lund RG, Bottino MC.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies performed by the authors involving human participants or animals.
Consent to participate
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ribeiro, J.S., Xavier, S.R., Cuevas Suárez, C.E. et al. Synthesis and characterization of calcium-releasing elastomeric resin-based endodontic sealers. Clin Oral Invest 27, 3447–3456 (2023). https://doi.org/10.1007/s00784-023-04952-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04952-0