Abstract
Objectives
To identify and report the current landmarks used for measuring gingival thickness (GT) in healthy maxillary anterior teeth.
Material and methods
The protocol of this Preferred Reporting Items of Systematic Reviews and Meta-Analyses (PRISMA) 2020-compliant systematic review was registered in PROSPERO. A literature search was conducted to identify articles that met the eligibility criteria published up to 2022. The methods of assessing gingival thickness and the landmarks adopted on the studies were described. Primary outcomes were identified, and the frequency of reporting in the selected articles was calculated. Additionally, risk-of-bias assessments were performed for individual articles.
Results
Fifty-eight articles (34 with low risk of bias and 24 with medium risk of bias) were selected. A total of 3638 individuals had their gingival thickness measured. Thirty-nine different landmarks were adopted in the studies. Fifty-six articles with 22 landmarks were included in the meta-analysis. A higher heterogeneity was found between the studies (GT ranged from 0.48 to 2.59 mm, mean GT 1.074; 95% CI: 1.024–1.104). The 3 most used landmarks were 2 mm from gingival margin (10 studies, mean GT 1.170 mm, 95% CI: 1.085–1.254), bone crest (9 studies, mean GT 1.01 mm; 95% CI: 0.937–1.083), and cemento-enamel junction (7 studies, mean GT 1.172 mm; 95% CI: 1.105, 1.239).
Conclusions
Within the limits of this study, a large heterogeneity in GT was found, and there was no consensus on the ideal landmark for GT measurement.
Clinical relevance
The landmark 2 mm from gingival margin, located at attached gingiva, can be used for GT measurement by clinical and image-based devices. This is an important step for a quantitative instead of a qualitative evaluation of phenotypes.


Similar content being viewed by others
Data Availability
Data available on request from the authors.
References
Jepsen S, Caton JG, Albandar JM et al (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(Suppl 1):S237–S248. https://doi.org/10.1002/JPER.17-0733
Cortellini P, Bissada NF (2018) Mucogingival conditions in the natural dentition: narrative review, case definitions, and diagnostic considerations. J Periodontol 89(Suppl 1):S204–S213. https://doi.org/10.1002/JPER.16-0671
Zweers J, Thomas RZ, Slot DE, Weisgold AS, Van der Weijden FG (2014) Characteristics of periodontal biotype, its dimensions, associations and prevalence: a systematic review. J Clin Periodontol 41(10):958–971. https://doi.org/10.1111/jcpe.12275
Olsson M, Lindhe J, Marinello CP (1993) On the relationship between crown form and clinical features of the gingiva in adolescents. J Clin Periodontol 20(8):570–577. https://doi.org/10.1111/j.1600-051x.1993.tb00773.x
Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH (2010) Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent 30(3):237–243
Eger T, Müller HP, Heinecke A (1996) Ultrasonic determination of gingival thickness. Subject variation and influence of tooth type and clinical features. J Clin Periodontol 23(9):839–845. https://doi.org/10.1111/j.1600-051x.1996.tb00621.x
Alpiste-Illueca F (2004) Dimensions of the dentogingival unit in maxillary anterior teeth: a new exploration technique (parallel profile radiograph). Int J Periodontics Restorative Dent 24(4):386–396
Januário AL, Barriviera M, Duarte WR (2008) Soft tissue cone-beam computed tomography: a novel method for the measurement of gingival tissue and the dimensions of the dentogingival unit. J Esthet Restor Dent 20(6):366–373. https://doi.org/10.1111/j.1708-8240.2008.00210.x
Kim YJ, Park JM, Kim S, Koo KT, Seol YJ, Lee YM, Rhyu IC, Ku Y (2016) New method of assessing the relationship between buccal bone thickness and gingival thickness. J Periodontal Implant Sci 46(6):372–381. https://doi.org/10.5051/jpis.2016.46.6.372
Liu F, Pelekos G, Jin LJ (2017) The gingival biotype in a cohort of Chinese subjects with and without history of periodontal disease. J Periodont Res 52(6):1004–1010. https://doi.org/10.1111/jre.12471
Rodrigues DM, Petersen RL, de Moraes JR, Barboza EP (2022) Gingival landmarks and cutting points for gingival phenotype determination a clinical and tomographic cross-sectional study. J Periodontol 93(12):1916. https://doi.org/10.1002/JPER.21-0615
Rodrigues DM, Petersen RL, Montez C, de Moraes JR, Januário AL, Barboza EP (2022) Relationship between anterior maxillary tooth sagittal root position and periodontal phenotype: a clinical and tomographic study. Clin Oral Investig 26(2):1309–1321. https://doi.org/10.1007/s00784-021-04105-1
Maria N, Lazaros T, Christos A, Georgios M, Ioannnis V, Antonios K (2016) Classification of periodontal biotypes with the use of CBCT. Cross-Sectional Stud Clin Oral Investig 20(8):2061–2071. https://doi.org/10.1007/s00784-015-1694-y
Esfahanizadeh N, Daneshparvar N, Askarpour F, Akhoundi N, Panjnoush M (2016) correlation between bone and soft tissue thickness in maxillary anterior teeth. J Dent 13(5):302–308
Vandana KL, Savitha B (2005) Thickness of gingiva in association with age, gender and dental arch location. J Clin Periodontol 32(7):828–830. https://doi.org/10.1111/j.1600-051X.2005.00757.x
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane. Available from www.training.cochrane.org/handbook.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100
Chambrone L, Mandia J Jr, Shibli JA, Romito GA, Abrahao M (2013) Dental implants installed in irradiated jaws: a systematic review. J Dent Res 92(Suppl. 2):119S-130S. https://doi.org/10.1177/0022034513504947
Chambrone L, Preshaw PM, Ferreira JD, Rodrigues JA, Cassoni A, Shibli JA (2014) Effects of tobacco smoking on the survival rate of dental implants placed in areas of maxillary sinus floor augmentation: a systematic review. Clin Oral Impl Res 25(4):408–416. https://doi.org/10.1111/clr.12186
Chambrone L, Foz AM, Guglielmetti MR, Pannuti CM, Artese HPC, Feres M, Romito GA (2013) Periodontitis and chronic kidney disease: a systematic review of the association of diseases and the effect of periodontal treatment on estimated glomerular filtration rate. J Clin Periodontol 40(5):443–456. https://doi.org/10.1111/jcpe.12067
Chambrone L, Shibli JA, Mercurio CE, Cardoso B, Preshaw PM (2015) Efficacy of standard (SLA) and modified sandblasted and acid-etched (SLActive) dental implants in promoting immediate and/or early occlusal loading protocols: a systematic review of prospective studies. Clin Oral Impl Res 26(4):359–370. https://doi.org/10.1111/clr.12347
Chambrone L, Tatakis DN (2016) Long-term outcomes of untreated buccal gingival recessions: a systematic review and meta-analysis. J Periodontol 87(7):796–808. https://doi.org/10.1902/jop.2016.150625
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available from: ohri.ca/programs/clinical_epidemiology/oxford.htm
El Khalifa M, Abu el Sadat SM, Gaweesh YS, Gaweesh YY (2022) Assessment of gingival thickness using CBCT compared to transgingival probing and its correlation with labial bone defects: a cross-sectional study. Int J Oral Maxillofac Implants 37(3):464–472. https://doi.org/10.11607/jomi.9234
Yilmaz MN, Koseoglu Secgin C, Ozemre MO, İnonu E, Aslan S, Bulut S (2022) Assessment of gingival thickness in the maxillary anterior region using different techniques. Clin Oral Investig 26(11):6531–6538. https://doi.org/10.1007/s00784-022-04602-x
Montanha-Andrade K, Crusoé-Rebello IM, Araujo NS, Barreto MA, dos Santos JN, Cury PR (2022) Assessment of the relationship between tooth inclination and gingival and alveolar bone dimensions using computed tomography of the maxillary anterior teeth: a cross-sectional study. Dental Press J Orthod 27(4):e222136. https://doi.org/10.1590/2177-6709.27.4.e222136.oar
Gürlek Ö, Sönmez Ş, Güneri P, Nizam N (2018) A novel soft tissue thickness measuring method using cone beam computed tomography. J Esthet Restor Dent 30(6):516–522. https://doi.org/10.1111/jerd.12428
Shao Y, Yin L, Gu J, Wang D, Lu W, Sun Y (2018) Assessment of periodontal biotype in a young Chinese population using different measurement methods. Sci Reports 8(1):11212. https://doi.org/10.1038/s41598-018-29542-z
Amid R, Mirakhori M, Safi Y, Kadkhodazadeh M, Namdari M (2017) Assessment of gingival biotype and facial hard/soft tissue dimensions in the maxillary anterior teeth region using cone beam computed tomography. Arch Oral Biol 79:1–6. https://doi.org/10.1016/j.archoralbio.2017.02.021
Alves PHM, Alves TCLP, Pegoraro TA, Costa YM, Bonfante EA, de Almeida ALPF (2018) Measurement properties of gingival biotype evaluation methods. Clin Implant Dent Relat Res 20(3):280–284. https://doi.org/10.1111/cid.12583
Kheur MG, Kantharia NR, Kheur SM, Acharya A, Le B, Sethi T (2015) Three-dimensional evaluation of alveolar bone and soft tissue dimensions of maxillary central incisors for immediate implant placement: a cone-beam computed tomography assisted analysis. Implant Dent 24(4):407–415. https://doi.org/10.1097/ID.0000000000000259
Gluckman H, Pontes CC, Du Toit J, Coachman C, Salama M (2021) Dimensions of the dentogingival tissue in the anterior maxilla. A CBCT descriptive cross-sectional study. Int J Esthet Dent 16(4):580–592
Aslan S, Clauser T, Testori T, Fabbro MD, Rasperini G (2021) A novel technique for the estimation of gingival thickness: a preliminary study. Int J Periodontics Restorative Dent 41(4):571–577. https://doi.org/10.11607/prd.4947
Mallikarjun S, Babu HM, Das S, Neelakanti A, Dawra C, Shinde SV (2016) Comparative evaluation of soft and hard tissue dimensions in the anterior maxilla using radiovisiography and cone beam computed tomography: a pilot study. J Indian Soc Periodontol 20(2):174–177. https://doi.org/10.4103/0972-124X.170813
Yousefzadeh S, Johari M, Sheikhzadeh S, Haghanifar S, Gholinia H, Arbabzadegan Hashemi N (2021) A cross-sectional study of labial bone and covering soft tissue in maxillary anterior segment: a dilemma in orthodontics. Int J Dent 5553301. https://doi.org/10.1155/2021/5553301
Wang L, Chen J, Zhang W, Wu H, Yang F (2019) Accuracy of assessing gingival thickness in the esthetic maxillary region by periodontal probing, cone-beam computed tomography and digital scanning. Int J Clin Exp Med 12(8):10302–10309
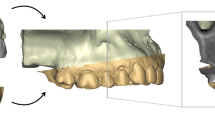
Bednarz-Tumidajewicz M, Sender-Janeczek A, Zborowski J et al (2020) In vivo evaluation of periodontal phenotypes using cone-beam computed tomography, intraoral scanning by computer-aided design, and prosthetic-driven implant planning technology. Med Sci Monit 26:e924469-1. https://doi.org/10.12659/MSM.924469
Couso-Queiruga E, Tattan M, Ahmad U, Barwacz C, Gonzalez-Martin O, Avila-Ortiz G (2021) Assessment of gingival thickness using digital file superimposition versus direct clinical measurements. Clin Oral Investig 25(4):2353–2361. https://doi.org/10.1007/s00784-020-03558-0
Wang L, Ruan Y, Chen J, Luo Y, Yang F (2022) Assessment of the relationship between labial gingival thickness and the underlying bone thickness in maxillary anterior teeth by two digital techniques. Sci Reports 12(1):709. https://doi.org/10.1038/s41598-021-04721-7
Kim YS, Park JS, Jang YH, Son JH, Kim WK, Lee YK, Kim SH (2021) Accuracy of periodontal probe visibility in the assessment of gingival thickness. J Periodontal Implant Sci 51(1):30–39. https://doi.org/10.5051/jpis.2003880194
Gánti B, Bednarz W, Kőműves K, Vág J (2019) Reproducibility of the PIROP ultrasonic biometer for gingival thickness measurements. J Esthet Restor Dent 31(3):263–267. https://doi.org/10.1111/jerd.12446
Sharma S, Thakur SL, Joshi SK, Kulkarni SS (2014) Measurement of gingival thickness using digital vernier caliper and ultrasonographic method: a comparative study. J Investig Clin Dent 5(2):138–143. https://doi.org/10.1111/jicd.12026
Chou YH, Tsai CC, Wang JC, Ho YP, Ho KY, Tseng CC (2008) New classification of crown forms and gingival characteristics in Taiwanese. The Open Dent J 2:114–119. https://doi.org/10.2174/1874210600802010114
Müller HP, Könönen E (2005) Variance components of gingival thickness. J Periodont Res 40(3):239–244. https://doi.org/10.1111/j.1600-0765.2005.00798.x
Younes F, Eghbali A, Raes M, De Bruyckere T, Cosyn J, De Bruyn H (2016) Relationship between buccal bone and gingival thickness revisited using non-invasive registration methods. Clin Oral implant Res 27(5):523–528. https://doi.org/10.1111/clr.12618
Issrani R, Chavva S, Prabhu N, Keluskar V, Jirge V, Kumbujkar V, Patil S (2013) Transgingival probing and ultrasonographic methods for determination of gingival thickness-a comparative study. Adv Human Biol 3(3):43–51
Müller HP, Schaller N, Eger T, Heinecke A (2000) Thickness of masticatory mucosa. J Clin Periodontol 27(6):431–436. https://doi.org/10.1034/j.1600-051x.2000.027006431.x
Anand PS, Bansa A, Shenoi BR, Kamath KP, Kamath NP, Anil S (2022) Width and thickness of the gingiva in periodontally healthy individuals in a central Indian population: a cross-sectional study. Clin Oral Investig 26(1):751–759. https://doi.org/10.1007/s00784-021-04053-w
Lee WZ, Ong MM, Yeo ABK (2018) Gingival profiles in a select Asian cohort: a pilot study. J Investig Clin Dent 9(1):e12269. https://doi.org/10.1111/jicd.12269
Kolte A, Kolte R, Shirke P, Ahuja C (2019) Assessment and correlation of gingival angle, gingival zenith angle, and gingival thickness: a cross-sectional study. Int J Esthet Dent 14(2):198–208
Kolte R, Kolte A, Mahajan A (2014) Assessment of gingival thickness with regards to age, gender, and arch location. J Indian Soc Periodontol 18(4):478–481. https://doi.org/10.4103/0972-124X.138699
Kolte RA, Kolte AP, Rathi P (2019) Association of the gingival line angle with the gingival and interdental smile line: a gender-based evaluation. Int J Esthet Dent 31(6):601–607. https://doi.org/10.1111/jerd.12517
Egreja AM, Kahn S, Barceleiro M, Bittencourt S (2012) Relationship between the width of the zone of keratinized tissue and thickness of gingival tissue in the anterior maxilla. Int J Periodontics Restorative Dent 32(5):573–579
Agarwal V, Mehrotra N, Vijay V (2017) Gingival biotype assessment: variations in gingival thickness with regard to age, gender, and arch location. Indian J Dent Sci 9(1):12–15
Aimetti M, Massei G, Morra M, Cardesi E, Romano F (2008) Correlation between gingival phenotype and Schneiderian membrane thickness. Int J Oral Maxillofac Implants 23(6):1128–1132
La Rocca AP, Alemany AS, Levi P Jr, Juan MV, Molina JN, Weisgold AS (2012) Anterior maxillary and mandibular biotype: relationship between gingival thickness and width with respect to underlying bone thickness. Implant Dent 21(6):507–515. https://doi.org/10.1097/ID.0b013e318271d487
de Araújo LNM, Borges SB, Dos Santos MT, Lima KC, Gurgel BCV (2020) Assessment of gingival phenotype through periodontal and crown characteristics: a cluster analysis. J Int Acad Periodontol 22(1):21–28
Frost NA, Mealey BL, Jones AA, Huynh-Ba G (2015) Periodontal biotype: gingival thickness as it relates to probe visibility and buccal plate thickness. J Periodontol 86(10):1141–1149. https://doi.org/10.1902/jop.2015.140394
Vandana KL, Shivani S, Savitha B, Vivek HP (2017) Assessment of gingival sulcus depth, width of attached gingiva, and gingival thickness in primary, mixed, and permanent dentition. J Den Res 4(1):42–49. https://doi.org/10.4103/jdrr.jdrr_42_17
Sanadi RM, Singh U, Ramteke KR (2018) Thick or thin-Visual vs direct assessment of gingival biotype. Int J Recent Sci Res 9(1):23345–23348. https://doi.org/10.24327/ijrsr.2018.0901.1450
Joshi A, Suragimath G, Zope SA, Ashwinirani SR, Varma SA (2017) Comparison of gingival biotype between different genders based on measurement of dentopapillary complex. J Clin Diagnostic Res 11(9):40–45. https://doi.org/10.7860/JCDR/2017/30144.10575
Stein JM, Lintel-Höping N, Hammächer C, Kasaj A, Tamm M, Hanisch O (2013) The gingival biotype: measurement of soft and hard tissue dimensions-a radiographic morphometric study. J Clin Periodontol 40(12):1132–1139. https://doi.org/10.1111/jcpe.12169
Mermon S, Patel JR, Sethuraman R, Patel R, Arora H (2015) A comparative evaluation of the reliability of three methods of assessing gingival biotype in dentate subjects in different age groups: an in vivo study. J Indian Prosthodont Soc 15(4):313–317. https://doi.org/10.4103/0972-4052.171830
Fischer KR, Richter T, Kebschull M, Petersen N, Fickl S (2015) On the relationship between gingival biotypes and gingival thickness in young Caucasians. Clin Oral Implant Res 26(8):865–869. https://doi.org/10.1111/clr.12356
Fischer KR, Künzlberger A, Donos N, Fickl S, Friedmann A (2018) Gingival biotype revisited—novel classification and assessment tool. Clin Oral Investig 22(1):443–448. https://doi.org/10.1007/s00784-017-2131-1
Rungcharassaeng K, Kan JY, Yoshino S, Morimoto T, Zimmerman G (2012) Immediate implant placement and provisionalization with and without a connective tissue graft: an analysis of facial gingival tissue thickness. Int J Periodontics Restorative Dent 32:657–663
Chow RLK, Lau SL, Leung YY, Chow JKF (2022) A non-invasive method for the assessment of gingival thickness in the aesthetic zone and the concept of the gingival geometric ratio in an Asian population. Int J Oral Maxillofac Surg S0901 5027(22):00319–8
Das G, Ahmed AR, Suleman G, Lal A, Rana MH, Ahmed N, Arora S (2022) A comparative evaluation of dentogingival tissue using transgingival probing and cone-beam computed tomography. Med 58(9):1312. https://doi.org/10.3390/medicina58091312
Nik-Azis NM, Razali M, Goh V, Ahmad Shuhaimi NN, Mohd Nazrin NAS (2022) Assessment of gingival thickness in multi-ethnic subjects with different gingival pigmentation levels. J Clin Periodontol. 12. https://doi.org/10.1111/jcpe.13723
Matosinhos FRP, Nigro F, Barbosa BA, Franco AG, Sotto-Maior BS, Francischone CE (2022) Analysis of buccal gingival thickness in maxillary implants and its relation to gingival biotype. Res, Soc Dev 11:e46411528472. https://doi.org/10.33448/rsd-v11i5.28472
Costa FA, Perussolo J, Dias DR, Araújo M (2022) Identification of thin and thick gingival phenotypes by two transparency methods: a diagnostic accuracy study. J Periodontolhttps://doi.org/10.1001/JPER.220488
Kao RT, Curtis DA, Kim DM et al (2020) American Academy of Periodontology best evidence consensus statement on modifying periodontal phenotype in preparation for orthodontic and restorative treatment. J Periodontol 91(3):289–298. https://doi.org/10.1002/JPER.19-0577
Ainamo J, Löe H (1966) Anatomical characteristics of gingiva. A clinical and microscopic study of the free and attached gingiva. J Periodontol 37(1):5–13. https://doi.org/10.1902/jop.1966.37.1.5
Lee CT, Sanz-Miralles E, Zhu L, Glick J, Heath A, Stoupel J (2020) Predicting bone and soft tissue alterations of immediate implant sites in the esthetic zone using clinical parameters. Clin Implant Dent Relat Res 22(3):325–332. https://doi.org/10.1111/cid.12910
Cabello G, Rioboo M, Fábrega JG (2013) Immediate placement and restoration of implants in the aesthetic zone with a trimodal approach: soft tissue alterations and its relation to gingival biotype. Clin Oral Implants Res 24(10):1094–1100. https://doi.org/10.1111/j.1600-0501.2012.02516.x
Chambrone L, Avila-Ortiz G (2021) An evidence-based system for the classification and clinical management of non-proximal gingival recession defects. J Periodontol 92(3):327–335. https://doi.org/10.1002/JPER.20-0149
Cairo F, Cortellini P, Pilloni A et al (2016) Clinical efficacy of coronally advanced flap with or without connective tissue graft for the treatment of multiple adjacent gingival recessions in the aesthetic area: a randomized controlled clinical trial. J Clin Periodontol 43(10):849–856. https://doi.org/10.1111/jcpe.12590
Hwang D, Wang HL (2006) Flap thickness as a predictor of root coverage: a systematic review. J Periodontol 77(10):1625–1634. https://doi.org/10.1902/jop.2006.060107
Santamaria MP, Silveira CA, Mathias IF et al (2018) Treatment of single maxillary gingival recession associated with non-carious cervical lesion: randomized clinical trial comparing connective tissue graft alone to graft plus partial restoration. J Clin Periodontol 45(8):968–976. https://doi.org/10.1111/jcpe.12907
Batista EL Jr, Moreira CC, Batista FC, de Oliveira RR, Pereira KK (2012) Altered passive eruption diagnosis and treatment: a cone beam computed tomography-based reappraisal of the condition. J Clin Periodontol 39(11):1089–1096. https://doi.org/10.1111/j.1600-051X.2012.01940.x
Borges GJ, Ruiz LF, de Alencar AH, Porto OC, Estrela C (2015) Cone-beam computed tomography as a diagnostic method for determination of gingival thickness and distance between gingival margin and bone crest. Sci World J 2015:142108. https://doi.org/10.1155/2015/142108
Bienz SP, Pirc M, Papageorgiou SN, Jung RE, Thoma DS (2022) The influence of thin as compared to thick peri-implant soft tissues on aesthetic outcomes: a systematic review and meta-analysis. Clin Oral Implants Res 33(Suppl 23):56–71. https://doi.org/10.1111/clr.13789
Wang J, Cha S, Zhao Q, Bai D (2022) Methods to assess tooth gingival thickness and diagnose gingival phenotypes: a systematic review. J Esthet Restor Dent 34(4):620–632. https://doi.org/10.1111/jerd.12900
Ferry K, AlQallaf H, Blanchard S, Dutra V, Lin WS, Hamada Y (2022) Evaluation of the accuracy of soft tissue thickness measurements with three different methodologies: an in vitro study. J Periodontol 93(10):1468–1475
Avila-Ortiz G, Couso-Queiruga E, Pirc M, Chambrone L, Thoma DS (2022) Outcome measures and methods of assessment of soft tissue augmentation interventions in the context of dental implant therapy: a systematic review of clinical studies published in the last 10 years. J Clin Periodontol. https://doi.org/10.1111/jcpe.13597
Pini Prato G, Gianfilippo RD, Pannuti CM et al (2022) Diagnostic reproducibility of the 2018 classification of gingival recession defects and gingival phenotype: a multicenter inter- and intra-examiner agreement study. J Periodontolhttps://doi.org/10.1002/JPER.22-0501
Funding
This study was supported in part by the Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ), Brazil, FAPERJ-E-26/200.746/2021.
Author information
Authors and Affiliations
Contributions
DMR had the idea for the article. DMR and LC contributed to conception and design. CM and DL performed the literature search. DMR, CM, DL, and EPB contribute to data acquisition and extraction. DMR and LC analyzed and interpreted the data found. DMR, LC, and CM made the draft manuscript. DMR, LC, and EPB critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All investigations and procedures were conducted according to the principles expressed in the Declaration of Helsinki. Ethical approval for the review was not required. No experiments involving human participants/animals (or their tissue) were conducted. The analysis was performed only by reviewing published articles.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rodrigues, D.M., Chambrone, L., Montez, C. et al. Current landmarks for gingival thickness evaluation in maxillary anterior teeth: a systematic review. Clin Oral Invest 27, 1363–1389 (2023). https://doi.org/10.1007/s00784-023-04898-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04898-3