Abstract
Objectives
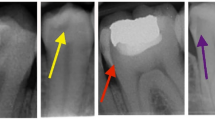
Pulpal calcifications are discrete hard calcified masses of varying sizes in the dental pulp cavity. This study is aimed at measuring the performance of the YOLOv4 deep learning algorithm to automatically determine whether there is calcification in the pulp chambers in bite-wing radiographs.
Materials and methods
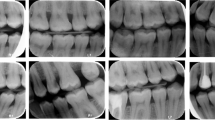
In this study, 2000 bite-wing radiographs were collected from the faculty database. The oral radiologists labeled the pulp chambers on the radiographs as “Present” and “Absent” according to whether there was calcification. The data were randomly divided into 80% training, 10% validation, and 10% testing. The weight file for pulpal calcification was obtained by training the YOLOv4 algorithm with the transfer learning method. Using the weights obtained, pulp chambers and calcifications were automatically detected on the test radiographs that the algorithm had never seen. Two oral radiologists evaluated the test results, and performance criteria were calculated.
Results
The results obtained on the test data were evaluated in two stages: detection of pulp chambers and detection of pulpal calcification. The detection performance of pulp chambers was as follows: recall 86.98%, precision 98.94%, F1-score 91.60%, and accuracy 86.18%. Pulpal calcification “Absent” and “Present” detection performance was as follows: recall 86.39%, precision 85.23%, specificity 97.94%, F1-score 85.49%, and accuracy 96.54%.
Conclusion
The YOLOv4 algorithm trained with bite-wing radiographs detected pulp chambers and calcification with high success rates.
Clinical relevance
Automatic detection of pulpal calcifications with deep learning will be used in clinical practice as a decision support system with high accuracy rates in diagnosing dentists.







Similar content being viewed by others
Data availability
The data sets are available from the corresponding author on a reasonable request.
Change history
08 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00784-023-05240-7
References
Üçok M (2013) Diş Pulpasında Meydana Gelen Kalsifikasyonlar. J Istanbul Univ Fac Dent 13:251–280
Gulsahi A, Cebeci SÖ (2009) A radiographic assessment of the prevalence of pulp stones in a group of Turkish dental patients. Int Endod J 42(8):735–739
Sezgin B, Cakan E, Erdem T (2011) Pulpa Kalsifikasyonlarının Sıklığı Ve Dağılımının Radyografik İnceleme Yöntemiyle Değerlendirilmesi. J Istanbul Univ Fac Dent 45(2):49–55
Arys A, Philippart C, Dourov N (1993) Microradiography and light microscopy of mineralization in the pulp of undemineralized human primary molars. J Oral Pathol Med 22(2):49–53
Hillmann G, Geurtsen W (1997) Light-microscopical investigation of the distribution of extracellular matrix molecules and calcifications in human dental pulps of various ages. Cell Tissue Res 289(1):145–154
Keleş A, C Keskin, MA Versiani (2021) Micro-CT assessment of radicular pulp calcifications in extracted maxillary first molar teeth. Clin Oral Investig: 1–8.
Goga R, Chandler NP, Oginni AO (2008) Pulp stones: a review. Int Endod J 41(6):457–468
Ingle JI, Bakland LK (2002) Endodontics, 5th edn. BC Decker Inc., Hamilton
Shan T, Tay F, Gu L (2021) Application of artificial intelligence in dentistry. J Dent Res 100(3):232–244
Atınç Y (2022) Yapay Zeka, 7th edn. Kodlab Press, Istanbul
Park WJ, Park JB (2018) History and application of artificial neural networks in dentistry. Eur J Dent 12(04):594–601
Jung SK, Kim TW (2016) New approach for the diagnosis of extractions with neural network machine learning. Am J Orthod Dentofacial Orthop 149(1):127–133
Leite AF et al (2021) Artificial intelligence-driven novel tool for tooth detection and segmentation on panoramic radiographs. Clin Oral Investig 25(4):2257–2267
Saglam H. et al (2021) Diş Hekimliğinde Yapay Zeka: artificial intelligence in Dentistry. Journal of Artificial Intelligence in Health Sciences ISSN: 2757–9646, 2021 1(2): 26–33.
Orhan K et al (2020) Evaluation of artificial intelligence for detecting periapical pathosis on cone-beam computed tomography scans. Int Endod J 53(5):680–689
Nicolielo LFP et al (2018) Computer-based automatic classification of trabecular bone pattern can assist radiographic bone quality assessment at dental implant site. Br J Radiol 91(1092):20180437
Kim DW et al (2021) Prediction of hand‐wrist maturation stages based on cervical vertebrae images using artificial intelligence. Orthod Craniofac Res.
Schwendicke F et al (2021) Cost-effectiveness of artificial intelligence for proximal caries detection. J Dent Res 100(4):369–376
Farhadian M, Shokouhi P, Torkzaban P (2020) A decision support system based on support vector machine for diagnosis of periodontal disease. BMC Res Notes 13(1):1–6
Şeker A, Diri B, Balik HH (2017) Derin Öğrenme Yöntemleri ve Uygulamaları Hakkında Bir İnceleme. Gazi Mühendislik Bilimleri Dergisi 3(3):47–64
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521(7553):436–444
Arslan E (2021) Evrişimli sinir ağı özelliklerine dayanan korelasyon filtreleme ve veri ilişkilendirme ile çoklu nesne takibi. Bilgisayar Mühendisliği Anabilim Dalı. Bursa Uludağ Üniversitesi (Türkiye).
Bozkaya F et al (2021) (2021) Otonom Sistemlerde Veri Çoğaltma Yöntemleri Kullanılarak İyileştirilmiş Gerçek Zamanlı Nesne Tespiti. Avrupa Bilim ve Teknoloji Dergisi 30:83–87
Bochkovskiy A, CY Wang, HYM. Liao (2020) Yolov4: optimal speed and accuracy of object detection. arXiv preprint arXiv:.10934.
Lee JH et al (2020) Application of a fully deep convolutional neural network to the automation of tooth segmentation on panoramic radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol 129(6):635–642
He K et al (2016) Deep residual learning for image recognition. In Proceedings of the IEEE conference on computer vision and pattern recognition.
Bayraktar Y, E Ayan (2021) Diagnosis of interproximal caries lesions with deep convolutional neural network in digital bite-wing radiographs. Clin Oral Investig: 1–10.
Hung K et al (2020) The use and performance of artificial intelligence applications in dental and maxillofacial radiology: a systematic review. Dentomaxillofac Radiol 49(1):20190107
Thrall JH et al (2018) Artificial intelligence and machine learning in radiology: opportunities, challenges, pitfalls, and criteria for success. J Am Coll Radiol 15(3):504–508
Özkan İ, Ülker E (2017) Derin öğrenme ve görüntü analizinde kullanılan derin öğrenme modelleri. Gaziosmanpaşa Bilimsel Araştırma Dergisi 6(3):85–104
Sayegh F, Reed A (1968) Calcification in the dental pulp. Oral Surg Oral Med Oral Pathol 25(6):873–882
Jacobsen I, Kerekes K (1977) Long-term prognosis of traumatized permanent anterior teeth showing calcifying processes in the pulp cavity. Scand J Dent Res 85(7):588–598
Nayak M, Kumar J, Prasad LK (2010) A radiographic correlation between systemic disorders and pulp stones. Indian J Dent Res 21(3):369
Khanna SS, Dhaimade PA (2017) Artificial intelligence: transforming dentistry today. Indian J Basic Appl Med Res 6(3):161–167
Moss-Salentijn L, Klyvert MH (1983) Epithelially induced denticles in the pulps of recently erupted, noncarious human premolars. J Endod 9(12):554–560
Kayal RA (2016) Distortion of digital panoramic radiographs used for implant site assessment. J Orthod Sci 5(4):117
Tassoker M, Magat G, Sener S (2018) A comparative study of cone-beam computed tomography and digital panoramic radiography for detecting pulp stones. isd 48(3):201–212
Willman W (1934) Calcifications in the pulp. Bur 34:73
Sisman Y et al (2012) The prevalence of pulp stones in a Turkish population A radiographic survey. Med Oral Patol Oral Cir Bucal 17(2):e212–e217
Çolak H et al (2012) Assessment of the prevalence of pulp stones in a sample of Turkish Central Anatolian population. Sci World J 2012:804278
Fariza A et al (2018) Segmenting tooth components in dental x-ray images using Gaussian kernel-based conditional spatial Fuzzy C-Means clustering algorithm. Int J Intell Eng 12(3):108–117
Tom CE (2015) J Thomas (2015) Segmentation of tooth and pulp from dental radiographs. Int J Sci Eng Res 6(11):115–121
Selmi A, L Syed, B Abdulkareem (2021) Pulp stone detection using deep learning techniques. In EAI International Conference on IoT Technologies for HealthCare. Springer.
Lee S et al (2021) Deep learning for early dental caries detection in bite-wing radiographs. Sci Rep 11(1):16807
Yang YM et al (2016) CBCT-aided microscopic and ultrasonic treatment for upper or middle thirds calcified root canals. Biomed Res Int.
Liu W et al (2016) Ssd: single shot multibox detector. In European conference on computer vision. 2016. Springer.
Redmon J, A Farhadi (2017) YOLO9000: better, faster, stronger. In 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR).
Park JH et al (2019) Automated identification of cephalometric landmarks: part 1—comparisons between the latest deep-learning methods YOLOV3 and SSD. Angle Orthod 89(6):903–909
Jiang L et al (2021) A two-stage deep learning architecture for radiographic assessment of periodontal bone loss.
Yang H et al (2020) Deep learning for automated detection of cyst and tumors of the jaw in panoramic radiographs. J Clin Med 9(6):1839
Tao R, E Gavves, AW Smeulders (2016) Siamese instance search for tracking. In Proceedings of the IEEE conference on computer vision and pattern recognition.
Behpour S, KM Kitani, BD Ziebart (2017) ADA: A game-theoretic perspective on data augmentation for object detection. arXiv preprint arXiv:.07735
Zhao ZQ et al (2019) Object detection with deep learning: a review. IEEE Trans Neural Netw Learn Syst 30(11):3212–3232
Takahashi T et al (2021) Deep learning-based detection of dental prostheses and restorations. Sci Rep 11(1):1–7
Chen H et al (2019) A deep learning approach to automatic teeth detection and numbering based on object detection in dental periapical films. Sci Rep 9(1):1–11
Buckley CE, EM Voorhees (2005) Retrieval system evaluation. 2005.
Alalharith DM et al (2020) A deep learning-based approach for the detection of early signs of gingivitis in orthodontic patients using faster region-based convolutional neural networks. Int J Environ Res Public Health 17(22):8447
Laishram A, K Thongam (2020) Detection and classification of dental pathologies using faster-RCNN in orthopantomogram radiography image. In 2020 7th International Conference on Signal Processing and Integrated Networks (SPIN). IEEE.
Lipton ZC, C Elkan, B Narayanaswamy (2014) Thresholding classifiers to maximize F1 score. arXiv preprint arXiv:.01396
Wang CW et al (2016) A benchmark for comparison of dental radiography analysis algorithms. Med Image Anal 31:63–76
Jader G et al (2018) Deep instance segmentation of teeth in panoramic X-ray images. in 2018 31st SIBGRAPI Conference on Graphics, Patterns and Images (SIBGRAPI)
Acknowledgements
None. This study was presented as an oral presentation at XVIII. ECDMFR (European Congress of Dentomaxillofacial Radiology) Congress (Virtual) on 8th-10th June, 2022.
Author information
Authors and Affiliations
Contributions
FY and MT obtained the imaging data and performed the radiological examination. MÜÖ designed the method and conducted the deep learning work and statistical analyses. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was conducted at the Faculty of Dentistry, Necmettin Erbakan University, Department of Dentomaxillofacial Radiology, with the approval of the Ethics Committee (No. 12/94) and was performed according to the stipulations laid out by the Declaration of Helsinki.
Informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: This article was originally published with equations written incorrectly.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuce, F., Öziç, M.Ü. & Tassoker, M. Detection of pulpal calcifications on bite-wing radiographs using deep learning. Clin Oral Invest 27, 2679–2689 (2023). https://doi.org/10.1007/s00784-022-04839-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04839-6