Abstract
Objectives
This study was aimed at evaluating the correlation and reproducibility of gingival thickness quantification using digital and direct clinical assessment methods.
Materials and methods
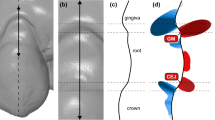
Patients in need of tooth extraction were allocated into two groups according to the gingival thickness measurement method, either using an endodontic spreader (pre-extraction) or a spring caliper (post-extraction), both on the mid-facial (FGT) and mid-lingual (LGT). Pre-extraction Digital Imaging and COmmunications in Medicine (DICOM) and STereoLithography (STL) files of the arch of interest were obtained and merged for corresponding digital measurements. Inter-rater reliability between digital and direct assessment methods was analyzed using inter-class correlation coefficients (ICC).
Results
Excellent inter-rater reliability agreement was demonstrated for all parameters. Comparison between the endodontic spreader and the digital method revealed excellent agreement, with ICC of 0.79 (95% CI 0.55, 0.91) for FGT and 0.87 (95% CI 0.69, 0.94) for LGT, and mean differences of 0.08 (− 0.04 to 0.55) and 0.25 (− 0.30 to 0.81) mm for FGT and LGT, respectively. Meanwhile, the comparison between the caliper and the digital method demonstrated poor agreement, with ICC of 0.38 (95% CI − 0.06, 0.70) for FGT and 0.45 (95% CI − 0.02, 0.74) for LGT, and mean differences of 0.65 (0.14 to 1.16) and 0.64 (0.12 to 1.17) mm for FGT and LGT, respectively.
Conclusions
Digital measurement of gingival thickness is comparable with direct clinical assessments performed with transgingival horizontal probing using an endodontic spreader.
Clinical relevance
Digital assessment of gingival thickness is a non-tissue invasive, reliable, and reproducible method that could be utilized as an alternative to horizontal transgingival probing.




Similar content being viewed by others
References
Kao RT, Curtis DA, Kim DM, Lin GH, Wang CW, Cobb CM, Hsu YT, Kan J, Velasquez D, Avila-Ortiz G, Yu SH, Mandelaris GA, Rosen PS, Evans M, Gunsolley J, Goss K, Ambruster J, Wang HL (2020) American Academy of Periodontology best evidence consensus statement on modifying periodontal phenotype in preparation for orthodontic and restorative treatment. J Periodontol 91(3):289–298. https://doi.org/10.1002/JPER.19-0577
Lin GH, Curtis DA, Kapila Y, Velasquez D, Kan JYK, Tahir P, Avila-Ortiz G, Kao RT (2020) The significance of surgically modifying soft tissue phenotype around fixed dental prostheses: an American Academy of Periodontology best evidence review. J Periodontol 91(3):339–351. https://doi.org/10.1002/JPER.19-0310
Jepsen S, Caton JG, Albandar JM, Bissada NF, Bouchard P, Cortellini P, Demirel K, de Sanctis M, Ercoli C, Fan J, Geurs NC, Hughes FJ, Jin L, Kantarci A, Lalla E, Madianos PN, Matthews D, McGuire MK, Mills MP, Preshaw PM, Reynolds MA, Sculean A, Susin C, West NX, Yamazaki K (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions: classification and case definitions for periodontal manifestations of systemic diseases and developmental and acquired conditions. J Periodontol 89:S237–S248. https://doi.org/10.1002/JPER.17-0733
Cook DR, Mealey BL, Verrett RG, Mills MP, Noujeim ME, Lasho DJ, Cronin RJ Jr (2011) Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. The International journal of periodontics & restorative dentistry 31(4):345–354
Fu J-H, Yeh C-Y, Chan H-L, Tatarakis N, Leong DJM, Wang H-L (2010) Tissue biotype and its relation to the underlying bone morphology. J Periodontol 81(4):569–574. https://doi.org/10.1902/jop.2009.090591
Stellini E, Comuzzi L, Mazzocco F, Parente N, Gobbato L (2013) Relationships between different tooth shapes and patient’s periodontal phenotype. J Periodontal Res 48(5):657–662. https://doi.org/10.1111/jre.12057
Hwang D, Wang H-L (2006) Flap thickness as a predictor of root coverage: a systematic review. J Periodontol 77(10):1625–1634. https://doi.org/10.1902/jop.2006.060107
Baldi C, Pini-Prato G, Pagliaro U, Nieri M, Saletta D, Muzzi L, Cortellini P (1999) Coronally advanced flap procedure for root coverage. Is flap thickness a relevant predictor to achieve root coverage? A 19-case series. J Periodontol 70(9):1077–1084. https://doi.org/10.1902/jop.1999.70.9.1077
Avila-Ortiz G, Gonzalez-Martin O, Couso-Queiruga E, Wang HL (2020) The peri-implant phenotype. J Periodontol 91(3):283–288. https://doi.org/10.1002/JPER.19-0566
Linkevicius T, Grybauskas S, Puisys A (2009) The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial.8
Vervaeke S, Matthys C, Nassar R, Christiaens V, Cosyn J, De Bruyn H (2018) Adapting the vertical position of implants with a conical connection in relation to soft tissue thickness prevents early implant surface exposure: a 2-year prospective intra-subject comparison. J Clin Periodontol 45(5):605–612. https://doi.org/10.1111/jcpe.12871
Bressan E, Paniz G, Lops D, Corazza B, Romeo E, Favero G (2011) Influence of abutment material on the gingival color of implant-supported all-ceramic restorations: a prospective multicenter study. Clin Oral Implants Res 22(6):631–637. https://doi.org/10.1111/j.1600-0501.2010.02008.x
Jung RE, Holderegger C, Sailer I, Khraisat A, Suter A, Hammerle CH (2008) The effect of all-ceramic and porcelain-fused-to-metal restorations on marginal peri-implant soft tissue color: a randomized controlled clinical trial. Int J Periodontics Restorative Dent 28(4):357–365
Evans CDJ, Chen ST (2007) Esthetic outcomes of immediate implant placements. Clinical Oral Implants Research 0 (0):071025001541009-??? doi:https://doi.org/10.1111/j.1600-0501.2007.01413.x
Eghbali A, De Rouck T, De Bruyn H, Cosyn J (2009) The gingival biotype assessed by experienced and inexperienced clinicians. J Clin Periodontol 36(11):958–963. https://doi.org/10.1111/j.1600-051X.2009.01479.x
De Rouck T, Eghbali R, Collys K, De Bruyn H, Cosyn J (2009) The gingival biotype revisited: transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J Clin Periodontol 36(5):428–433. https://doi.org/10.1111/j.1600-051X.2009.01398.x
Rasperini G, Acunzo R, Cannalire P, Farronato G (2015) Influence of periodontal biotype on root surface exposure during orthodontic treatment: a preliminary study. The International Journal of Periodontics & Restorative Dentistry 35(5):665–675. https://doi.org/10.11607/prd.2239
Kan JY, Rungcharassaeng K, Umezu K, Kois JC (2003) Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol 74(4):557–562. https://doi.org/10.1902/jop.2003.74.4.557
Alves PHM, Alves T, Pegoraro TA, Costa YM, Bonfante EA, de Almeida A (2018) Measurement properties of gingival biotype evaluation methods. Clin Implant Dent Relat Res 20(3):280–284. https://doi.org/10.1111/cid.12583
Chan H-L, Sinjab K, Li J, Chen Z, Wang H-L, Kripfgans OD (2018) Ultrasonography for noninvasive and real-time evaluation of peri-implant tissue dimensions. J Clin Periodontol 45(8):986–995. https://doi.org/10.1111/jcpe.12918
Tattan M, Sinjab K, Lee E, Arnett M, Oh TJ, Wang HL, Chan HL, Kripfgans OD (2019) Ultrasonography for chairside evaluation of periodontal structures: a pilot study. J Periodontol 91:890–899. https://doi.org/10.1002/JPER.19-0342
Claffey N, Shanley D (1986) Relationship of gingival thickness and bleeding to loss of probing attachment in shallow sites following nonsurgical periodontal therapy. J Clin Periodontol 13(7):654–657. https://doi.org/10.1111/j.1600-051X.1986.tb00861.x
Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH (2010) Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent 30(3):237–243
Güth J-F, Runkel C, Beuer F, Stimmelmayr M, Edelhoff D, Keul C (2017) Accuracy of five intraoral scanners compared to indirect digitalization. Clin Oral Investig 21(5):1445–1455. https://doi.org/10.1007/s00784-016-1902-4
Pieterse H, Diamant Z (2014) Good clinical practice in clinical interventional studies. Eur Clin Respir J 1. doi:https://doi.org/10.3402/ecrj.v1.26422
Doyle DJ, Garmon EH American Society of Anesthesiologists Classification (ASA Class). https://www.ncbi.nlm.nih.gov/books/NBK441940/. Accessed April 1st 2020
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86(2):420–428
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Lee JS, Jeon YS, Strauss FJ, Jung HI, Gruber R (2020) Digital scanning is more accurate than using a periodontal probe to measure the keratinized tissue width. Sci Rep 10(1):3665. https://doi.org/10.1038/s41598-020-60291-0
Schneider D, Ender A, Truninger T, Leutert C, Sahrmann P, Roos M, Schmidlin P (2014) Comparison between clinical and digital soft tissue measurements. J Esthet Restor Dent 26(3):191–199. https://doi.org/10.1111/jerd.12084
Eger T, Muller HP, Heinecke A (1996) Ultrasonic determination of gingival thickness. Subject variation and influence of tooth type and clinical features. J Clin Periodontol 23(9):839–845. https://doi.org/10.1111/j.1600-051x.1996.tb00621.x
Sala L, Alonso-Perez R, Agustin-Panadero R, Ferreiroa A, Carrillo-de-Albornoz A (2018) Comparative in vitro study of two methods for gingival biotype assessment. J Clin Exp Dent 10(9):e858–e863. https://doi.org/10.4317/jced.55049
Kloukos D, Koukos G, Doulis I, Sculean A, Stavropoulos A, Katsaros C (2018) Gingival thickness assessment at the mandibular incisors with four methods: a cross-sectional study. J Periodontol 89(11):1300–1309. https://doi.org/10.1002/JPER.18-0125
Acknowledgments
The authors would like to thank Ms. Karen Kluesner, study coordinator at the Craniofacial Clinical Research Program at the University of Iowa College of Dentistry, for her efforts and support during the conduction of the study.
Funding
This study was supported by the Department of Periodontics Graduate Student Research Fund, University of Iowa College of Dentistry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the University of Iowa Institutional Review Board (IRB) in October 2019 (HawkIRB #201909749). This study was conducted and monitored according to the principles of Good Clinical Practice (GCP) [25]. All clinical procedures were performed in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Couso-Queiruga, E., Tattan, M., Ahmad, U. et al. Assessment of gingival thickness using digital file superimposition versus direct clinical measurements. Clin Oral Invest 25, 2353–2361 (2021). https://doi.org/10.1007/s00784-020-03558-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03558-0