Abstract
Objectives
Melatonin is a hormone, which is involved in the control of the circadian rhythm, but also acts as an antioxidant and immune modulator. Previous studies reported decreased salivary and serum melatonin levels in periodontitis. This prospective cohort trial assessed the effect of non-surgical periodontal therapy on melatonin levels.
Methods
Salivary and serum samples of 60 participants (30 patients suffering from a severe generalized form of periodontitis, 30 healthy controls) were collected at baseline and 19 samples of periodontitis patients after treatment. Salivary and serum melatonin levels were determined by a commercially available ELISA kit and serum C-reactive protein (CRP) by a routine laboratory test.
Results
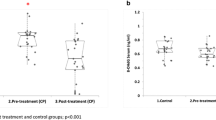
At baseline, periodontitis patients showed significantly increased serum CRP values and significantly decreased salivary melatonin levels compared to the control group. Clinical periodontal parameters significantly correlated with salivary melatonin levels and serum CRP. Periodontal therapy resulted in a recovery of the decreased salivary melatonin levels and a negative correlation was detected for the changes of salivary melatonin and the inflammatory parameter bleeding on probing. Serum melatonin levels showed no significant differences.
Conclusions
Salivary melatonin levels recovered after periodontal therapy and correlated with a decrease of local periodontal inflammation. This may imply the local involvement of melatonin in the pathogenesis of periodontitis due to its antioxidant abilities. However, the exact role of melatonin in periodontal disease remains to be investigated in future trials.
Clinical relevance
The present results suggest salivary melatonin as a risk indicator for the severity of periodontal disease.


Similar content being viewed by others
References
Brook I (2003) Microbiology and management of periodontal infections. Gen Dent 51:424–428
Holtfreter B, Kocher T, Hoffmann T et al (2010) Prevalence of periodontal disease and treatment demands based on a German dental survey (DMS IV). J Clin Periodontol 37:211–219
Akalin FA, Toklu E, Renda N (2005) Analysis of superoxide dismutase activity levels in gingiva and gingival crevicular fluid in patients with chronic periodontitis and periodontally healthy controls. J Clin Periodontol 32:238–243
Sculley DV, Langley-Evans SC (2002) Salivary antioxidants and periodontal disease status. Proc Nutr Soc 61:137–143
Wei D, Zhang XL, Wang YZ et al (2010) Lipid peroxidation levels, total oxidant status and superoxide dismutase in serum, saliva and gingival crevicular fluid in chronic periodontitis patients before and after periodontal therapy. Aust Dent J 55:70–78
Reiter RJ (1991) Pineal melatonin: cell biology of its synthesis and of its physiological interactions. Endocr Rev 12:151–180
Kumasaka S, Shimozuma M, Kawamoto T et al (2010) Possible involvement of melatonin in tooth development: expression of melatonin 1a receptor in human and mouse tooth germs. Histochem Cell Biol 133:577–584
Laakso ML, Porkka-Heiskanen T, Alila A et al (1990) Correlation between salivary and serum melatonin: dependence on serum melatonin levels. J Pineal Res 9:39–50
Cutando A, Aneiros-Fernandez J, Lopez-Valverde A et al (2011) A new perspective in oral health: potential importance and actions of melatonin receptors MT1, MT2, MT3, and RZR/ROR in the oral cavity. Arch Oral Biol 56(10):944–950
Shimozuma M, Tokuyama R, Tatehara S et al (2011) Expression and cellular localizaion of melatonin-synthesizing enzymes in rat and human salivary glands. Histochem Cell Biol 135:389–396
Reiter RJ, Tan DX, Mayo JC et al (2003) Melatonin as an antioxidant: biochemical mechanisms and pathophysiological implications in humans. Acta Biochim Pol 50:1129–1146
Tekbas OF, Ogur R, Korkmaz A et al (2008) Melatonin as an antibiotic: new insights into the actions of this ubiquitous molecule. J Pineal Res 44:222–226
Choi EY, Jin JY, Lee JY et al (2011) Melatonin inhibits Prevotella intermedia lipopolysaccharide-induced production of nitric oxide and interleukin-6 in murine macrophages by suppressing NF-kappaB and STAT1 activity. J Pineal Res 50(2):197–206. doi:10.1111/j.1600-079X.2010.00829.x
Cutando A, Gomez-Moreno G, Villalba J et al (2003) Relationship between salivary melatonin levels and periodontal status in diabetic patients. J Pineal Res 35:239–244
Gomez-Moreno G, Cutando-Soriano A, Arana C et al (2007) Melatonin expression in periodontal disease. J Periodontal Res 42:536–540
Srinath R, Acharya AB, Thakur SL (2010) Salivary and gingival crevicular fluid melatonin in periodontal health and disease. J Periodontol 81:277–283
Armitage GC (1999) Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4:1–6
Saxer UP, Muhlemann HR (1975) Motivation and education. SSO Schweiz Monatsschr Zahnheilkd 85:905–919
Lange DE, Plagmann HC, Eenboom A et al (1977) Clinical methods for the objective evaluation of oral hygiene. Dtsch Zahnarztl Z 32:44–47
Bruckmann C, Durstberger G, Matejka M (2006) The “Viennese Treatment Strategy”. Part II. Stomatologie 103(1):11–16
Durstberger G, Bruckmann C, Matejka M (2006) The “Viennese treatment strategy”. Part II. Stomatologie 103(2):33–38
Cutando A, Galindo P, Gomez-Moreno G et al (2006) Relationship between salivary melatonin and severity of periodontal disease. J Periodontol 77:1533–1538
Bertl K, Haririan H, Laky M et al (2012) Smoking influences salivary histamine levels in periodontal disease. Oral Dis 18:410–416
Haririan H, Bertl K, Laky M et al (2012) Salivary and serum chromogranin A and alpha-amylase in periodontal health and disease. J Periodontol. doi:10.1902/jop.2012.110604
Raggam RB, Santner BI, Kollroser M et al (2008) Evaluation of a novel standardized system for collection and quantification of oral fluid. Clin Chem Lab Med 46:287–291
Team RDC (2010) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Tamaki N, Tomofuji T, Ekuni D et al (2009) Short-term effects of non-surgical periodontal treatment on plasma level of reactive oxygen metabolites in patients with chronic periodontitis. J Periodontol 80:901–906
Cutando A, Gomez-Moreno G, Arana C et al (2007) Melatonin: potential functions in the oral cavity. J Periodontol 78:1094–1102
Reiter RJ, Tan DX, Manchester LC et al (2007) Medical implications of melatonin: receptor-mediated and receptor-independent actions. Adv Med Sci 52:11–28
Tan DX, Chen LD, Poeggeler B, Manchester LC, Reiter RJ (1993) Melatonin: a potent, endogenous hydroxyl radical scavenger. Endocr J 1:57–60
Andrukhov O, Ulm C, Reischl H et al (2010) Serum cytokine levels in periodontitis patients in relation to the bacterial load. J Periodontol 82(6):885–892
Nakajima T, Honda T, Domon H et al (2010) Periodontitis-associated up-regulation of systemic inflammatory mediator level may increase the risk of coronary heart disease. J Periodontal Res 45:116–122
Shimada Y, Komatsu Y, Ikezawa-Suzuki I et al (2010) The effect of periodontal treatment on serum leptin, interleukin-6, and C-reactive protein. J Periodontol 81:1118–1123
Sener G, Tugtepe H, Velioglu-Ogunc A et al (2006) Melatonin prevents neutrophil-mediated oxidative injury in Escherichia coli-induced pyelonephritis in rats. J Pineal Res 41:220–227
Matejka M, Partyka L, Ulm C et al (1998) Nitric oxide synthesis is increased in periodontal disease. J Periodontal Res 33:517–518
Gitto E, Reiter RJ, Cordaro SP et al (2004) Oxidative and inflammatory parameters in respiratory distress syndrome of preterm newborns: beneficial effects of melatonin. Am J Perinatol 21:209–216
Gulcin I, Buyukokuroglu ME, Kufrevioglu OI (2003) Metal chelating and hydrogen peroxide scavenging effects of melatonin. J Pineal Res 34:278–281
Koyama H, Nakade O, Takada Y et al (2002) Melatonin at pharmacologic doses increases bone mass by suppressing resorption through down-regulation of the RANKL-mediated osteoclast formation and activation. J Bone Miner Res 17:1219–1229
Nakade O, Koyama H, Ariji H et al (1999) Melatonin stimulates proliferation and type I collagen synthesis in human bone cells in vitro. J Pineal Res 27:106–110
Roth JA, Kim BG, Lin WL et al (1999) Melatonin promotes osteoblast differentiation and bone formation. J Biol Chem 274:22041–22047
Ramirez-Fernandez MP, Calvo-Guirado JL, Sanchez de-Val JES et al (2012) Melatonin promotes angiogenesis during repair of bone defects: a radiological and histomorphometric study in rabbit tibiae. Clin Oral Investig. doi:10.1007/s00784-012-0684-6
Gomez-Moreno G, Guardia J, Ferrera MJ et al (2010) Melatonin in diseases of the oral cavity. Oral Dis 16:242–247
Dodson ER, Zee PC (2010) Therapeutics for circadian rhythm sleep disorders. Sleep Med Clin 5:701–715
Miller SC, Pandi-Perumal SR, Esquifino AI et al (2006) The role of melatonin in immuno-enhancement: potential application in cancer. Int J Exp Pathol 87:81–87
Sanchez-Barcelo EJ, Mediavilla MD, Tan DX et al (2010) Clinical uses of melatonin: evaluation of human trials. Curr Med Chem 17:2070–2095
Cutando A, Arana C, Gomez-Moreno G et al (2007) Local application of melatonin into alveolar sockets of beagle dogs reduces tooth removal-induced oxidative stress. J Periodontol 78:576–583
Calvo-Guirado JL, Gomez-Moreno G, Barone A et al (2009) Melatonin plus porcine bone on discrete calcium deposit implant surface stimulates osteointegration in dental implants. J Pineal Res 47:164–172
Calvo-Guirado JL, Gomez-Moreno G, Lopez-Mari L et al (2010) Actions of melatonin mixed with collagenized porcine bone versus porcine bone only on osteointegration of dental implants. J Pineal Res 48:194–203
Cutando A, Gomez-Moreno G, Arana C et al (2008) Melatonin stimulates osteointegration of dental implants. J Pineal Res 45:174–179
Takechi M, Tatehara S, Satomura K et al (2008) Effect of FGF-2 and melatonin on implant bone healing: a histomorphometric study. J Mater Sci Mater Med 19:2949–2952
Acknowledgments
The authors thank Mrs. Hedwig Rutschek and Mrs. Phuong Quynh Nguyen (laboratory technicians of the Bernhard Gottlieb School of Dentistry, Medical University of Vienna, Austria) for their excellent work in preparing and performing the experiments. Greiner Bio One supported this study by financing materials (reagents and saliva collection system) (Medical University of Vienna, §26, project number AP00345OFF).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bertl, K., Schoiber, A., Haririan, H. et al. Non-surgical periodontal therapy influences salivary melatonin levels. Clin Oral Invest 17, 1219–1225 (2013). https://doi.org/10.1007/s00784-012-0801-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-012-0801-6



