Abstract
Background
Visual instruments are essential to ensure high-quality surgical outcomes for minimally invasive procedures and have gradually become the focus of research. Recently, a novel visual auxiliary instrument, a 3-dimensional exoscope (EX), has been applied for spinal surgery. However, its advantages over other auxiliary means (OAMs) in anterior cervical surgery need to be assessed.
Objective
To compare and evaluate the clinical outcomes of EX and OAMs in anterior cervical spine surgery using a meta-analysis and to provide the latest clinical evidence.
Methods
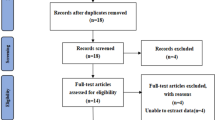
PubMed, Embase, Cochrane Library, Web of Science, CNKI, and Wanfang Database were systematically reviewed for relevant literature published prior to January 21, 2023. Two researchers independently screened the literature, extracted data, and assessed bias risk in the included literature. Review Manager software (version 5.4; the Cochrane Collaboration) was used to conduct the meta-analysis.
Results
five studies, one prospective and four retrospective cohort studies, with a total of 349 patients (154 in the EX group and 195 in the OAMs group) were included. A meta-analysis showed that compared to OAMs, EX-assisted anterior cervical spine surgery resulted in less intraoperative hemorrhage [WMD = -8.96, 95% CI (-14.21, -3.71), P = 0.0008]. Nevertheless, no significant differences in VAS scores, JOA scores, operation time, hospitalization time, and complication rate were observed between the two groups (P > 0.05).
Conclusion
EX and OAMs are equally safe and effective for anterior cervical spine surgery; however, compared to OAMs, EX results in less intraoperative hemorrhage.








Similar content being viewed by others
Data Availability
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ACDF:
-
Anterior cervical discectomy and fusion
- ACCF:
-
Anterior cervical corpectomy and fusion
- ACDR:
-
Artificial cervical disc replacement
- CI:
-
Confidence interval
- EX:
-
3-Dimensional Exoscope
- JOA:
-
Japanese Orthopaedic Association
- NDI:
-
Neck Disability Index
- OM:
-
Operating microscope
- OAMs:
-
Other auxiliary means
- RCTs:
-
Randomized controlled trials
- VAS:
-
Visual Analog Scale
- WMD:
-
Weighted mean differences
- RULA:
-
Rapid upper limb assessment
References
Adogwa O et al (2016) Comparison of surgical outcomes after anterior cervical discectomy and fusion: does the intra-operative use of a microscope improve surgical outcomes. J Spine Surg (Hong Kong) 2(1):25–30. https://doi.org/10.21037/jss.2016.01.04
Ariffin MHM et al (2020) Early Experience, Setup, Learning Curve, Benefits, and Complications Associated with Exoscope and Three-Dimensional 4K Hybrid Digital Visualizations in Minimally Invasive Spine Surgery. Asian Spine J 14(1):59–65. https://doi.org/10.31616/asj.2019.0075
Barbagallo GMV, Certo F (2019) Three-Dimensional, High-Definition Exoscopic Anterior Cervical Discectomy and Fusion: A Valid Alternative to Microscope-Assisted Surgery. World Neurosurg 130:e244–e250. https://doi.org/10.1016/j.wneu.2019.06.049
Choy W et al (2022) Superior Laryngeal Nerve Palsy After Anterior Cervical Diskectomy and Fusion: A Case Report and Cadaveric Description. Oper Neurosur (Hagerstown, Md) 23(2):e152–e155. https://doi.org/10.1227/ons.0000000000000276
Epstein NE (2019) A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int 10:100. https://doi.org/10.25259/SNI-191-2019
Garneau JC et al (2019) The use of the exoscope in lateral skull base surgery: advantages and limitations. Otol Neurotol: Off Publ Am Otol Soc, Am Neurotol Soc Eur Acad Otol Neurotol 40(2):236–240. https://doi.org/10.1097/MAO.0000000000002095
Hafez A, Haeren RHL et al (2021) Comparison of operating microscope and exoscope in a highly challenging experimental setting. World Neurosurg 147:e468–e475. https://doi.org/10.1016/j.wneu.2020.12.093
Hafez A, Haeren R et al (2023) 3D exoscopes in experimental microanastomosis: a comparison of different systems. Life (Basel) 13(2):584. https://doi.org/10.3390/life13020584
Higgins JPT et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clin Res ed) 343:d5928. https://doi.org/10.1136/bmj.d5928
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–58. https://doi.org/10.1002/sim.1186
Kim LH et al (2018) Anterior Techniques in Managing Cervical Disc Disease. Cureus 10(8):e3146. https://doi.org/10.7759/cureus.3146
Kosary IZ et al (1976) Microsurgery in anterior approach to cervical discs. Surg Neurol 6(5):275–277
Kwan K et al (2019) Lessons Learned Using a High-Definition 3-Dimensional Exoscope for Spinal Surgery. Oper Neurosurg (Hagerstown, Md) 16(5):619–625. https://doi.org/10.1093/ons/opy196
Lin H et al (2022) Cervical Spine Microsurgery with the High-Definition 3D Exoscope: Advantages and Disadvantages. World Neurosurg 161:e1–e7. https://doi.org/10.1016/j.wneu.2021.07.033
Liberati A et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clin Res ed) 339:b2700. https://doi.org/10.1136/bmj.b2700
Lu J et al (2000) Anterior approach to the cervical spine: surgical anatomy. Orthopedics 23(8):841–845. https://doi.org/10.3928/0147-7447-20000801-19
McAtamney L, Corlett EN (1993) RULA: a survey method for the investigation of work-related upper limb disorders. Appl Ergon 24(2):91–9. https://doi.org/10.1016/0003-6870(93)90080-s
Moher D et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1. https://doi.org/10.1186/2046-4053-4-1
Oertel JM, Burkhardt BW (2017) Vitom-3D for exoscopic neurosurgery: initial experience in cranial and spinal procedures. World Neurosurg 105:153–162. https://doi.org/10.1016/j.wneu.2017.05.109
Raheja A, Mishra S et al (2021) Impact of different visualization devices on accuracy, efficiency, and dexterity in neurosurgery: a laboratory investigation. Neurosurg Focus 50(1):E18. https://doi.org/10.3171/2020.10.FOCUS20786
Ramirez ME, Baez IP et al (2023) Comparative survey study of the use of a low cost exoscope vs. microscope for anterior cervical discectomy and fusion (ACDF). Front Med Technol 4:1055189. https://doi.org/10.3389/fmedt.2022.1055189
Riew KD et al (2003) Microsurgery for degenerative conditions of the cervical spine. Instr Course Lect 52:497–508
Rossmann T, Veldeman M et al (2023) 3d exoscopes are noninferior to operating microscopes in aneurysm surgery: comparative single-surgeon series of 52 consecutive cases. World Neurosurg 170:e200–e213. https://doi.org/10.1016/j.wneu.2022.10.106
Sachdev VP, Radna RJ (1994) Anterior-approach cervical diskectomy under the operating microscope. Mount Sinai J Med, New York 61(3):233–8
Sack J et al (2018) Initial experience using a high-definition 3-dimensional exoscope system for microneurosurgery. Oper Neurosurg (Hagerstown, Md) 14(4):395–401. https://doi.org/10.1093/ons/opx145
Siller S et al (2020) A high-definition 3D exoscope as an alternative to the operating microscope in spinal microsurgery. J Neurosurg Spine 1–10. https://doi.org/10.3171/2020.4.SPINE20374
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Wang PT et al (2021) Clinical effect of anterior cervical surgery assisted by 3D microscope. Orthopaedics 12(03):232–235.253.
Yao Y et al (2021) Three-dimensional high-definition exoscope (Kestrel View II) in anterior cervical discectomy and fusion: a valid alternative to operative microscope-assisted surgery. Acta Neurochir 163(12):3287–3296. https://doi.org/10.1007/s00701-021-04997-8
Yao ZP et al (2021) Preliminary clinical outcomes of 3D exoscopic anterior cervical discectomy and fusion for cervical spondylotic myelopathy. Orthop J China 29(09):779–783
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was not necessary as this study is a meta-analysis.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lei, F., Xie, Y., Fu, J. et al. Advantages of 3-dimensional exoscope-assisted anterior cervical spine surgery: A meta-analysis. Acta Neurochir 165, 3077–3087 (2023). https://doi.org/10.1007/s00701-023-05721-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05721-4