Abstract
Background
Routine shunting to minimize ischemia during carotid endarterectomy (CEA) is controversial. The aim of this study was to stratify the ischemic parameters associated with CEA and evaluate the effect of routine shunting in attempting to mitigate those ischemia.
Method
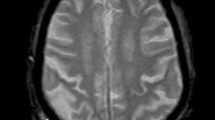
Data from 248 CEAs with routine shunting were retrospectively evaluated. Our assessment included somatosensory evoked potential (SSEP) amplitude reduction more than 50 % and longer than 5 min (SSEP<50%, >5 min), new postoperative diffusion-weighted imaging lesions (new DWI lesions), and severe stenosis as indicated by reduced ipsilateral middle cerebral artery (MCA) signal on preoperative magnetic resonance angiography (MRA asymmetry), as surrogates of hypoperfusion, microembli, and hemodynamic impairment, respectively.
Results
SSEP<50%, >5 min occurred in 15 % of CEAs during cross-clamping, and shunting reversed the SSEP changes. New DWI lesions were observed in 4.1 %. Pre-clamping the common and external carotid artery during dissection (pre-clamp method) decreased the rate of new DWI lesions compared to without pre-clamping (3.5 % vs. 7.5 %, P = 0.22). Occlusion time was significantly longer in the pre-clamp method than without pre-clamping (P < 0.0001). However, the incidence of SSEP<50%, >5 min was not increased with the pre-clamp method (p = 1.0) when using information regarding SSEP and collaterals to modify the speed of shunt manipulation. MRA asymmetry was identified in 39 CEAs (15.8 %) with correction of asymmetry postoperatively. MRA asymmetry correlated with symptomatic hyperperfusion (P = 0.0034). Only three CEAs had symptomatic hyperperfusion (1.2 %) with minimal symptoms. Ten CEAs sustained transient ischemia, symptomatic hyperperfusion, or 30-day-stroke (composite postoperative ischemic symptoms). Logistic regression analysis confirmed that SSEP<50%, >5 min (p = 0.009), new DWI lesions (p = 0.004) and MRA asymmetry (p = 0.042) were independent predictors of composite postoperative ischemic symptoms.
Conclusions
SSEP<50%, >5 min, new DWI lesions, and MRA asymmetry were able to stratify the ischemic impacts in CEA. Meticulous routine shunting could mitigate those appropriately.
Similar content being viewed by others
Abbreviations
- CAG:
-
Carotid angiography
- CCA:
-
Common carotid artery
- CEA:
-
Carotid endarterectomy
- CT:
-
Computed tomography
- CTA:
-
Computed tomographic angiography
- DSA:
-
Digital subtraction angiography
- DWI:
-
Diffusion-weighted imaging
- ECA:
-
External carotid artery
- ICA:
-
Internal carotid artery
- MCA:
-
Middle cerebral artery
- MRA:
-
Magnetic resonance angiography
- MRI:
-
Magnetic resonance imaging
- SPECT:
-
Single photon emission computed tomography
- SSEP:
-
Somatosensory evoked potentials
- STA:
-
Superficial temporal artery
- TIA:
-
Transient ischemic attack
- T2WI:
-
T2-weighted imaging
References
AbuRahma AF, Mousa AY, Stone PA (2011) Shunting during carotid endarterectomy. J Vasc Surg 54:1502–1510
Altinbas A, van Zandvoort MJE, van den Berg E, Jongen LM, Algra A, Moll FL, Nederkoorn PJ, Mali WPTM, Bonati LH, Brown MM, Kappelle LJ, van der Worp HB (2011) Cognition after carotid endarterectomy or stenting. A randomized comparison. Neurology 77:1084–1090
Beese U, Langer H, Lang W, Dinkel M (1998) Comparison of near-infrared spectroscopy and somatosensory evoked potentials for the detection of cerebral ischemia during carotid endarterectomy. Stroke 29:2032–2037
Bellosta R, Luzzani L, Carugati C, Talarico M, Sarcina A (2006) Routine shunting is a safe and reliable method of cerebral protection during carotid endarterectomy. Ann Vasc Surg 20:482–487
Bond R, Rerkasem K, Rothwell PM (2003) Routine or selective carotid artery shunting for carotid endarterectomy (and different methods of monitoring in selective shunting). Stroke 34:824–825
Branston NM, Ladds A, Symon L, Wang AD (1984) Comparison of the effect of ischemia on early components of the soamtosensory evoked potential in brainstem, thalamus, and cerebral cortex. J Cereb Blood Flow Metab 4:68–81
Brinkman SD, Braun P, Ganji S, Morrell RM, Jacobs LA (1984) Neuropsychological performance one week after carotid endarterectomy reflects intra-operative ischemia. Stroke 15(3):497–503
Cho H, Nemoto EM, Yonas H, Balzer J, Sclabassi RJ (1998) Cerebral monitoring by means of oximetry and somatosensory evoked potentials during carotid endarterectomy. J Neurosurg 89:533–538
De Rango P, Caso V, Leys D, Paciaroni M, Lenti M, Cao P (2008) The role of carotid artery stenting and carotid endarterectomy in cognitive performance. A systematic review. Stroke 39:3116–3127
De Vleeschauer P, Horsch S, Matamorous R (1988) Monitoring of somatosensory evoked potential in carotid surgery: results, usefulness and limitations of the method. Ann Vasc Surg 2(1):63–68
Feliziani FT, Polidori MC, Rango PD, Mangialasche F, Monastero R, Ercolani S, Raichi T, Cornacchiola V, Nelles G, Cao P, Mecocci P (2010) Cognitive performance in elderly patients undergoing carotid endarterectomy or carotid artery stenting: a twelve-month follow-up study. Cerebrovasc Dis 30:244–251
Furui T, Hasuo M (1984) Indwelling double-balloon shunt for carotid endarterectomy. Technical note. J Neurosurg 60:861–863
Gaunt ME, Martin PJ, Smith JL, Rimmer T, Cherryman G, Ratliff DA, Bell PRF, Naylor AR (1994) Clinical relevance of intraoperative embolization detected by transcranial Doppler ultrasonography during carotid endarterectomy: a prospective study of 100 patients. Br J Surg 81:1435–1439
Ghogawala Z, Westerveld M, Amin-Hanjani S (2008) Cognitive outcome after carotid revascularization: the role of cerebral emboli and hypoperfusion. Neurosurgery 62:385–395
Halsey JH (1992) Risk and benefit of shunting in carotid endarterectomy. Stroke 23:1589–1587
Hamdan AD, Pomposelli FB, Gibbons GW, Campbell DR, LoGerfo FW (1999) Perioperative stroke after 1001 consecutive carotid endarterectomy procedures without an electroencephalogram. Arch Surg 134:412–415
Heyer EJ, Adams DC, Solomon RA, Todd GJ, Quest DO, McMahon DJ, Steneck SD, Choudhri TF, Connolly ES (1998) Neuropsychometric changes in patients after carotid endarterectomy. Stroke 29:1110–1115
Heyer EJ, DeLaPaz R, Halazum HJ, Rampersad A, Sciacca R, Zurica J, Benvenisty AI, Quest DO, Todd GJ, Lavine S, Solomon RA, Connolly ES (2006) Neuropsychological dysfunction in the absence of structural evidence for cerebral ischemia after uncomplicated carotid endarterectomy. Neurosurgery 58:474–480
Heyer EJ, Sharma R, Rampersad A, Winfree CJ, Mack WJ, Solomon RA, Todd GJ, McCormick PC, McMurtry JG, Quest DO, Stern Y, Lazar RM, Connolly ES (2002) A controlled prospective study of neuropsychological dysfunction following carotid endarterectomy. Arch Neurol 59:217–222
Hirooka R, Ogasawara K, Inoue T, Fujiwara S, Sasaki M, Chida K, Ishigaki D, Kobayashi M, Nishimoto H, Otawara Y, Tsushima E, Ogawa A (2009) Simple assessment of cerebral hemodynamics using single-slab three dimensional time-of-flight magnetic resonance angiography in patients with quantitative perfusion single-photon emission computed tomography. AJNR Am J Neuroradiol 30:559–563
Inoue T, Ohwaki K, Tamura A, Tsutsumi K, Saito I, Saito N (2013) Subclinical ischemia verified by somatosensory evoked potential amplitude reduction during carotid endarterectomy: negative effects on cognitive performance. J Neurosurg. doi:10.3171/2013.1JNS121668
Inoue T, Tsutsumi K, Maeda K, Adachi S, Tanaka S, Yako K, Saito K, Kunii N (2006) Incidence of ischemic lesions by diffusion-weighted imaging after carotid endarterectomy with routine shunt usage. Neurol Med Chir (Tokyo) 46:529–534
Kawamata T, Okada Y, Kawashima A, Yoneyama T, Yamaguchi K, Ono Y, Hori T (2009) Postcarotid endarterectomy cerebral hyperperfusion can be prevented by minimizing intraoperative cerebral ischemia and strict postoperative blood pressure control under continuous sedation. Neurosurgery 64:447–454
Kuroda H, Ogasawara K, Hirooka R, Kobayashi M, Fujiwara S, Chida K, Ishigaki D, Otawara Y, Ogawa A (2009) Prediction of cerebral hyperperfusion after carotid endarterectomy using middle cerebral artery signal intensity in preoperative single-slab 3-dimensional time-of-flight magnetic resonance angiography. Neurosurgery 64:1065–1072
Lal BK, Younes M, Cruz G, Kapadia I, Jamil Z, Pappas PJ (2011) Cognitive changes after surgery vs stenting for carotid artery stenosis. J Vasc Surg 54:691–698
Manninen PH, Tan TK, Sarjeant RM (2001) Somatosensory evoked potential monitoring during carotid endarterectomy in patients with a stroke. Anesth Analg 93:39–44
Mazul-Sunko B, Hromatko I, Tadinac M, Sekulić A, Ivanec Ž, Gvozudenović A, Tomašević B, Gavranović Z, Maladić-Batinica I, Čima A, Vrkić N, Lovričević I (2010) Subclinical neurocognitive dysfunction after carotid endarterectomy—the impact of shunting. J Neurosurg Anesthesiol 22:195–201
Mocco J, Wilson DA, Komotar RJ, Zurica J, Mack WJ, Halazun HJ, Hatami R, Sciacca RR, Connolly ES, Heyer EJ (2006) Predictors of neurocognitive decline after carotid endarterectomy. Neurosurgery 58:844–850
North American Symptomatic Carotid Endarterectomy Trial Collaborators (1991) Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 325:445–453
Ogasawara K, Yamadate K, Kobayashi M, Endo H, Fukuda T, Yoshida K, Terasaki K, Inoue T, Ogawa A (2005) Postoperative cerebral hyperperfusion associated with impaired cognitive function in patients undergoing carotid endarterectomy. J Neurosurg 102:38–44
Ropper AH (1986) Evoked potentials in cerebral ischemia. Stroke 17:3–5
Rowed DW, Houlden DA, Burkholder LM, Taylor AB (2004) Comparison of monitoring technique for intraoperative cerebral ischemia. Can J Neurol Sci 31:347–356
Schnaudigel S, Gröschel K, Pilgram SM, Kastrup A (2008) New brain lesions after carotid stenting versus carotid endarterectomy. A systematic review of the literature. Stroke 39:1911–1919
Skejelland M, Krohg-SØrensen K, TennØe B, Bakke SJ, Brucher R, Russell D (2009) Cerebral microemboli and brain injury during carotid artery endarterectomy and stenting. Stroke 40:230–234
Smith JL, Evans DH, Fan L, Gaunt ME, London NJM, Bell PRF, Naylor AR (1995) Interpretation of embolic phenomena during carotid endarterectomy. Stroke 26:2281–2284
Sundt TM Jr, Sharbrough FW, Piepgras DG, Kearns TP, Messick J Jr, O’Fallon WM (1981) Correlation of cerebral blood flow and electroencephalographic changes during carotid endarterectomy: with results of surgery and hemodynamics of cerebral ischemia. Mayo Clin Proc 56:533–543
Sztriha LK, Nemeth D, Sefcsik T, Vecsei L (2009) Carotid stenosis and the cognitive function. J Neurol Sci 283:36–40
Wasser K, Pilgram-Pastor SM, Schnaudigel S, Stojanovic T, Schmidt H, Knauf J, Gröschel K, Knauth M, Hildebrandt H, Kastrup A (2011) New brain lesions after carotid revascularization are not associated with cognitive performance. J Vasc Surg 53:61–70
Weigand MA, Laipple A, Plaschke K, Eckstein HH, Martin E, Bardenheuer HJ (1999) Concentration changes of malondialdehyde across the cerebral vascular bed and shedding of l-selectin during carotid endarterectomy. Stroke 30:306–311
Wolf O, Heider P, Heinz M, Poppert H, Sander D, Greil O, Weiss W, Hanke M, Eckstein H (2004) Microembolic signals detected by transcranial Doppler sonography during carotid endarterectomy and correlation with serial diffusion-weighted imaging. Stroke:e373–e375
Woodworth GF, McGirt MJ, Than KD, Huang J, Perler BA, Tamargo RJ (2007) Selective versus routine intraoperative shunting during carotid endarterectomy: a multivariate outcome analysis. Neurosurgery 61:1170–1177
Acknowledgments
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
We read with particular interest the article by Inoue et al. The authors should be congratulated for all the data they collected and presented. The authors admit to several study limitations, including retrospective analysis design and a small number of cases in some subgroups. The authors report on 248 carotid endarterectomies and the aims of study were to stratify ischemic parameters associated with carotid endarterectomy (CEA) and evaluate the combination of routine electrophysiological monitoring and shunting to mitigate the ischemia.
Some facts are noteworthy, such as the analysis of magnetic resonance angiography (MRA) asymmetry for postoperative hyperperfusion, the incidence of somatosensory evoked potential (SSEP) decrease reversed by shunt introduction, introduction of extracranial-intracranial bypass for security in contralateral occlusion and absence of any single injury to the ramus marginalis of the facial nerve in 248 CEAs.
However, the article is often difficult to read and follow. The authors present a tremendous amount of data and a number of correlations. The title includes 24 words and the reader has to pay utmost attention not to get lost in the article. We would like to underscore a few issues that deserve special comment and criticism.
Monitoring and routine shunting. Over the past 25 years, many articles have been published on various CEA practices ranging from obsolete “no shunting, no monitoring” to routine shunting in monitored surgery. With no respect to this, to the CEA techniques and type of anesthesia, the MM results always range from 1 to 3 % when the series is reported by a single institution. It seems the risk of CEA resides elsewhere and not in the technical aspects of surgery. Timing of surgery, selection of patients for CEA, clinical presentation, the true extent of carotid stenosis, the length of the stenosis probably represent some of the factors that are more likely to influence the outcome of surgery than the technical aspects of surgery [1, grant project IGA NT 13627-4]. Inoue et al. report an MM rate of 2 %, a figure well within reported limits outside randomized trials.
There are various techniques used today to localize potential hypoperfusion during CEA. Using local anesthesia, any neurological deterioration during surgery calls for the need of shunt placement. The GALA trial showed that local anesthesia does not lead to a significantly better outcomes than CEA performed under general anesthesia [2]. Various techniques have been used when general anesthesia is applied for CEA. Recently, the most frequently used policy is a selective shunting strategy with some type of monitoring (e.g., SSEP, EEG, TCD, xenon CT, or even old-fashioned stump pressure monitoring). Selective shunting minimizes the inherent risk of shunt introduction. No definitive answer is available as to which technique is most reliable. In our hands a combination of bilateral SSEP and EEG provides the best results [3].
To detect cerebral hypoperfusion the authors used the SSEP monitoring procedure. They believe that a cut-off of 50 % amplitude decrease longer than 5 min predicts postoperative neurological deficits. There are many studies on this topic, including one from our group [3]. Our strategy is rather similar (bilateral SSEP and EEG) but the shunt is used selectively. Inoue et al. monitor SSEP and introduce a shunt in every case. In our view, the combination of routine shunting and SSEP monitoring is redundant in the sense that it is like wearing both belt and suspenders.
The authors spent 17 min during CEA for cross-clamping. This time of internal carotid artery blood flow interruption consists of 10 min for shunt introduction and 7 min for its removal. Their “pre-clamp” technique to occlude common and external carotids to decrease the risk of embolization is one explanation for the long duration of the clamping period. It is well documented that the sequelae of ischemic events depends on duration and depth of ischemia in the ischemic area [4]. Unlike Inoue et al., we are aware that the absence of oxygen causes neuronal death within 5 min and therefore the clamping period should be shortened as much as possible. In cases when a shunt is introduced, the monitoring with SSEP and EEG and subsequent shunt introduction takes 3–4 min while shunt removal requires another 1–2 min. It may easily be possible that some of the ischemic events in the Inoue et al. study were caused rather than prevented by this very long occlusion time. The fundamental question is whether the surgeon believes that significant changes in monitoring correlate with the risk of neurological deterioration. In such a scenario, a shunt is introduced; in those cases with stable monitoring, endarterectomy is performed without shunt placement. If monitoring is considered unreliable or not available, routine shunting is an acceptable strategy.
In the Inoue et al. study SSEPs were monitored unilaterally only. Thus, the value of this type of monitoring is very limited. It is highly unlikely that all conditions that might influence the monitoring and that can be adjusted and evaluated in bilateral monitoring only are adjusted (especially, e.g., the effects of arterial blood pressure fluctuations and depth of anesthesia). We do not understand how the lack of manpower may cause unilateral rather than logical bilateral monitoring.
The authors claim that new DWI lesions independently predict postoperative ischemic symptoms and that such lesions stratify the ischemic affects in CEA. A new DWI lesion is an ischemic lesion, which has or does not have clinical sequelae. It is not a predictor of ischemic events. Meningioma as seen on MR imaging is not a predictor of meningioma; rather, it is meningioma. Because it is so apparent that new DWI lesions correlate with postoperative symptoms, we do not find any value in this finding.
Contralateral internal carotid artery (ICA) occlusion was present in 10 CEAs (4 %), with seven CEAs preceded by contralateral superficial temporal artery-middle cerebral artery anastomosis (EC-IC) after confirming the compromized vascular reserve of the contralateral side with single photon emission computed tomography (SPECT). The number of patients who passed this test (7 of 10) is surprising. In our study we have found this ratio to be far less (1 of 10) [5]. This ratio seems to be a standard ratio in the selection process for possible EC-IC. After the contralateral CEA, the hemodynamic parameters of the hemisphere ipsilateral to the carotid occlusion improved due to the increased flow via the Circle of Willis. We do not believe that insufficient anterior communicating artery is common in the Japanese population. Further, we do not believe in an MM rate of 0 % in any surgery, but as of now our stats show an MM rate of 0 % in our series of 77 patients with contralateral carotid occlusion and with shunting in 5 % of the cases. Two surgeries can never have less risk than one surgery. The authors performed seven EC-IC bypasses without any complications, which is nothing exceptional. A first complication, which unavoidably must come, will most likely be the last bypass for security. Inoue et al. do not present any data supporting the strategy of preventive contralateral bypass.
In the introduction the authors discussed cognitive function after CEA and potential neurocognitive decline, as well as a possible effect of shunting to reduce these potential impairments. We fully agree with the authors on this topic and this is most likely the reason for the employment of routine shunting. However, Inoue et al. did not study any neurocognitive sequelae of CEA and thus the authors could not correlate their results of ischemic risk stratification to neurocognitive outcome.
We would like to congratulate the authors for amassing an extraordinary amount of data. They also should be applauded for how thoroughly the patients are managed. CEA at the present authors’ institution is not a 60-min routine surgical procedure as in the majority of other institutions in the world. Although Inoue et al. raise many questions and speculate about a number of issues related to CEA and its ischemic complication, it is a pity the reader is offered few substantiated answers.
We are thankful to the authors for presenting the topic of CEA and cerebral ischemia in a neurosurgical journal. In many European countries, neurosurgeons do not perform CEAs. In these countries CEA is a procedure used primarily by vascular or general surgeons. The goal of CEA is the prevention of cerebral damage (stroke) in the same manner as in clipping the aneurysm, resecting the arteriovenous malformation (AVM) or cavernoma. For us, it is rather difficult to make the distinction between the damge caused by bleeding or ischemia. If the brain is endangered and a neurosurgeon has the means and knowledge to prevent such damage, he or she is the best suited physician to provide this support.
Vladimír Beneš
David Netuka
Prague, Czech Republic
1. Netuka D, Ostrý S, Belsán T, Rucka D, Mandys V, Charvát F, Bradác O, Benes V (2010) Magnetic resonance angiography, digital subtraction angiography and Doppler ultrasonography in detection of carotid artery stenosis: a comparison with findings from histological specimens. Acta Neurochir (Wien) 152(7):1215–21
2. GALA Trial Collaborative Group, Lewis SC, Warlow CP, Bodenham AR, Colam B, Rothwell PM, Torgerson D, Dellagrammaticas D, Horrocks M, Liapis C, Banning AP, Gough M, Gough MJ (2008) General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet 372(9656):2132–42
3. Stejskal L, Kramár F, Ostrý S, Benes V, Mohapl M, Limberk B (2007) Experience of 500 cases of neurophysiological monitoring in carotid endarterectomy. Acta Neurochir (Wien) 149(7):681–8
4. Carter LP, Yamagata S, Erspamer R (1983) Time limits of reversible cortical ischemia. Neurosurgery 12:620–623
5. Beneš V, Mohapl M (2000) Reconstructive Surgery in Cerebral Ischemia: Reconstructive surgery in cerebral ischemia: extra-intracranial arterial bypass—is revival possible. Adv Clin Exper Med Suppl 1:33–40
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video clip showing CEA with the pre-clamp method. (MPG 30988 kb)
Rights and permissions
About this article
Cite this article
Inoue, T., Tsutsumi, K., Ohwaki, K. et al. Stratification of intraoperative ischemic impact by somatosensory evoked potential monitoring, diffusion-weighted imaging and magnetic resonance angiography in carotid endarterectomy with routine shunt use. Acta Neurochir 155, 2085–2096 (2013). https://doi.org/10.1007/s00701-013-1858-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1858-y