Abstract
Purpose
The insufficient clearance of regional lymph nodes and unsatisfactory R0 resection rate may result in the metastasis of left-sided pancreatic ductal adenocarcinoma (PDAC) after conventional distal pancreatosplenectomy (CDPS). Radical antegrade modular pancreatosplenectomy (RAMPS) was designed to achieve R0 resection more successfully with better lymph-node clearance; however, there is still insufficient evidence of its short- and long-term results to confirm its superiority. We conducted this study to compare the efficiency of these two procedures.
Methods
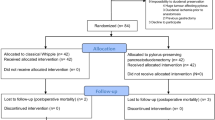
The subjects of this retrospective analysis were 103 patients with left-sided PDAC who underwent either RAMPS (n = 46) or CDPS (n = 57). We assessed perioperative data and surgical information and used univariate and multivariate analyses to identify prognostic factors for survival.
Results
There were no significant differences in baseline data between the groups. RAMPS was associated with a significantly shorter hospital stay (12.11 days vs. 22.98 days; P < 0.001), and significantly less blood loss (451.09 ml vs. 764.04 ml, P = 0.002), as well as a significantly lower rate of blood transfusion (15.22% vs. 33.33%, P = 0.035). RAMPS and CDPS had comparable perioperative complication rates. Moreover, RAMPS achieved more effective lymph-node retrieval (17.87 vs. 10.23; P < 0.001). The RAMPS group had a higher overall survival (OS) rate (28.73 months vs. 18.30 months; P = 0.003) and a higher disease-free survival (DFS) rate (21.97 months vs. 9.40 months; P < 0.001).
Conclusion
RAMPS achieved better survival and surgical outcomes than CDPS for patients with left-sided PDAC.


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
Johnson CD, Schwall G, Flechtenmacher J, Trede M. Resection for adenocarcinoma of the body and tail of the pancreas. Br J Surg. 1993;80:1177–9.
Makohon-Moore AP, Zhang M, Reiter JG, Bozic I, Allen B, Kundu D, et al. Limited heterogeneity of known driver gene mutations among the metastases of individual patients with pancreatic cancer. Nat Genet. 2017;49:358–66.
Strasberg SM, Drebin JA, Linehan D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003;133:521–7.
Christein JD, Kendrick ML, Iqbal CW, Nagorney DM, Farnell MB. Distal pancreatectomy for resectable adenocarcinoma of the body and tail of the pancreas. J Gastrointest Surg. 2005;9:922–7.
Shoup M, Conlon KC, Klimstra D, Brennan MF. Is extended resection for adenocarcinoma of the body or tail of the pancreas justified? J Gastrointest Surg. 2003;7:946–52.
Mitchem JB, Hamilton N, Gao F, Hawkins WG, Linehan DC, Strasberg SM. Long-term results of resection of adenocarcinoma of the body and tail of the pancreas using radical antegrade modular pancreatosplenectomy procedure. J Am Coll Surg. 2012;214:46–52.
Grossman JG, Fields RC, Hawkins WG, Strasberg SM. Single institution results of radical antegrade modular pancreatosplenectomy for adenocarcinoma of the body and tail of pancreas in 78 patients. J Hepatobiliary Pancreat Sci. 2016;23:432–41.
Strasberg SM, Linehan DC, Hawkins WG. Radical antegrade modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg. 2007;204:244–9.
Wang F, Tian X, Zhang Z, Ma Y, Xie X, Liang J, et al. Demethylzeylasteral (ZST93) inhibits cell growth and enhances cell chemosensitivity to gemcitabine in human pancreatic cancer cells via apoptotic and autophagic pathways. Int J Cancer. 2018;142:1938–51.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–91.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8.
Marchegiani G, Andrianello S, Malleo G, De Gregorio L, Scarpa A, Mino-Kenudson M, et al. Does size matter in pancreatic cancer?: Reappraisal of tumour dimension as a predictor of outcome beyond the TNM. Ann Surg. 2017;266:142–8.
Delpero JR, Jeune F, Bachellier P, Regenet N, Le Treut YP, Paye F, et al. prognostic value of resection margin involvement after pancreaticoduodenectomy for ductal adenocarcinoma: updates from a French Prospective Multicenter Study. Ann Surg. 2017;266:787–96.
Rho SY, Hwang HK, Chong JU, Yoon DS, Lee WJ, Kang CM. Association of preoperative total lymphocyte count with prognosis in resected left-sided pancreatic cancer. ANZ J Surg. 2019;89:503–8.
Birnbaum DJ, Bertucci F, Finetti P, Birnbaum D, Mamessier E. Head and body/tail pancreatic carcinomas are not the same tumors. Cancers (Basel). 2019;11:497.
Fink DM, Steele MM, Hollingsworth MA. The lymphatic system and pancreatic cancer. Cancer Lett. 2016;381:217–36.
O’Morchoe CC. Lymphatic system of the pancreas. Microsc Res Tech. 1997;37:456–77.
Morales-Oyarvide V, Rubinson DA, Dunne RF, Kozak MM, Bui JL, Yuan C, et al. Lymph node metastases in resected pancreatic ductal adenocarcinoma: predictors of disease recurrence and survival. Br J Cancer. 2017;117:1874–82.
Li HJ, Chen YT, Yuan SQ. Proposal of a modified American Joint Committee on Cancer staging scheme for resectable pancreatic ductal adenocarcinoma with a lymph node ratio-based N classification: a retrospective cohort study. Medicine (Baltimore). 2018;97:e12094.
Malleo G, Maggino L, Ferrone CR, Marchegiani G, Mino-Kenudson M, Capelli P, et al. Number of examined lymph nodes and nodal status assessment in distal pancreatectomy for body/tail ductal adenocarcinoma. Ann Surg. 2019;270:1138–46.
Fukuda Y, Asaoka T, Maeda S, Hama N, Miyamoto A, Mori M, et al. Prognostic impact of nodal statuses in patients with pancreatic ductal adenocarcinoma. Pancreatology. 2017;17:279–84.
Tummers WS, Groen JV, Sibinga Mulder BG, Farina-Sarasqueta A, Morreau J, Putter H, et al. Impact of resection margin status on recurrence and survival in pancreatic cancer surgery. Br J Surg. 2019;106:1055–65.
Lai CC, Wang SY, Liao CH, Hsu JT, Chiang KC, Yeh TS, et al. Surgical margin status of patients with pancreatic ductal adenocarcinoma undergoing surgery with radical intent: risk factors for the survival impact of positive margins. Vivo. 2018;32:1591–7.
Latorre M, Ziparo V, Nigri G, Balducci G, Cavallini M, Ramacciato G. Standard retrograde pancreatosplenectomy versus radical antegrade modular pancreatosplenectomy for body and tail pancreatic adenocarcinoma. Am Surg. 2013;79:1154–8.
Cao F, Li J, Li A, Li F. Radical antegrade modular pancreatosplenectomy versus standard procedure in the treatment of left-sided pancreatic cancer: a systemic review and meta-analysis. BMC Surg. 2017;17:67.
Funding
This work was supported by the Project of Capital Health Research and Development of Special (No. 2020-1-4011), Beijing, China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was reviewed and approved by the Institutional Review Board (IRB) of Peking Union Medical College Hospital (No. S-k846).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dai, M., Zhang, H., Li, Y. et al. Radical antegrade modular pancreatosplenectomy (RAMPS) versus conventional distal pancreatosplenectomy (CDPS) for left-sided pancreatic ductal adenocarcinoma. Surg Today 51, 1126–1134 (2021). https://doi.org/10.1007/s00595-020-02203-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-02203-3