Abstract
Purpose
The pleural covering technique, i.e., wrapping a part of or the entire surface of the lung with oxidized regenerative cellulose (ORC), reinforces visceral pleura through pleural thickening for patients with pneumothorax and cystic lung diseases. However, it remains undetermined how ORC induces pleural thickening.
Methods
A histopathological examination was performed for lung specimens from patients who had recurrent pneumothoraces after pleural covering and re-operation (n = 5). To evaluate the influence of ORC on the pleura in vitro, we used MeT-5A cells (a human pleural mesothelial cell line).
Results
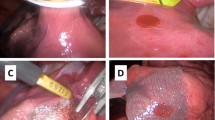
Pleural thickening was confirmed in all lung specimens examined. Three months after covering, the thickened pleura showed inflammatory cell infiltration, proliferation of myofibroblasts, and expression of fibronectin and TGF-β. However, after 1 year, those findings virtually disappeared, and the thickened pleura was composed mainly of abundant collagen. When MeT-5A cells were cultured in ORC-immersed medium, their morphology changed from a cobblestone to spindle-shaped appearance. The expression of E-cadherin decreased, whereas that of N-cadherin, α-smooth muscle actin, and fibronectin increased, suggesting mesothelial–mesenchymal transition (Meso–MT).
Conclusions
Our results suggest that Meso–MT may be involved as a mechanism of pleural thickening induced by pleural covering with ORC.







Similar content being viewed by others
References
Lee S, Kim HR, Cho S, Huh DM, Lee EB, Ryu KM, et al. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg. 2014;98:2005–11.
Kurihara M, Kataoka H, Ishikawa A, Endo R. Latest treatments for spontaneous pneumothorax. Gen Thorac Cardiovasc Surg. 2010;58:113–9.
Kurihara M, Mizobuchi T, Kataoka H, Sato T, Kumasaka T, Ebana H, et al. A total pleural covering for lymphangioleiomyomatosis prevents pneumothorax recurrence. PLoS ONE. 2016;11:e0163637.
Noda M, Okada Y, Maeda S, Sado T, Sakurada A, Hoshikawa Y, et al. An experience with the modified total pleural covering technique in a patient with bilateral intractable pneumothorax secondary to lymphangioleiomyomatosis. Ann Thorac Cardiovasc Surg. 2010;16:439–41.
Noda M, Okada Y, Maeda S, Sado T, Sakurada A, Hoshikawa Y, et al. A total pleural covering technique in patients with intractable bilateral secondary spontaneous pneumothorax: report of five cases. Surg Today. 2011;41:1414–7.
Kusu T, Nakagiri T, Minami M, Shintani Y, Kadota Y, Inoue M, et al. Null allele alpha-1 antitrypsin deficiency: case report of the total pleural covering technique for disease-associated pneumothorax. Gen Thorac Cardiovasc Surg. 2012;60:452–5.
Ebana H, Otsuji M, Mizobuchi T, Kurihara M, Takahashi K, Seyama K. Pleural covering application for recurrent pneumothorax in a patient with Birt–Hogg–Dube syndrome. Ann Thorac Cardiovasc Surg. 2016;22(3):189–92. doi:10.5761/atcs.cr.15-00228.
Kadota Y, Fukui E, Kitahara N, Okura E, Ohta M. Total pleural covering technique for intractable pneumothorax in patient with Ehlers–Danlos syndrome. Gen Thorac Cardiovasc Surg. 2016;64:425–8.
Lebendiger A, Gitlitz GF, Hurwitt ES, Lord GH, Henderson J. Laboratory and clinical evaluation of a new absorbable hemostatic material prepared from oxidized regenerated cellulose. Surg Forum. 1960;10:440–3.
Mutsaers SE. The mesothelial cell. Int J Biochem Cell Biol. 2004;36:9–16.
Haynes J, Srivastava J, Madson N, Wittmann T, Barber DL. Dynamic actin remodeling during epithelial–mesenchymal transition depends on increased moesin expression. Mol Biol Cell. 2011;22:4750–64.
Wu TH, Chiou YW, Chiu WT, Tang MJ, Chen CH, Yeh ML. The F-actin and adherence-dependent mechanical differentiation of normal epithelial cells after TGF-beta1-induced EMT (tEMT) using a microplate measurement system. Biomed Microdevice. 2014;16:465–78.
Chen LJ, Ye H, Zhang Q, Li FZ, Song LJ, Yang J, et al. Bleomycin induced epithelial–mesenchymal transition (EMT) in pleural mesothelial cells. Toxicol Appl Pharmacol. 2015;283:75–82.
Owens S, Jeffers A, Boren J, Tsukasaki Y, Koenig K, Ikebe M, et al. Mesomesenchymal transition of pleural mesothelial cells is PI3K and NFkappaB-dependent. Am J Physiol Lung Cell Mol Physiol. 2015. doi:10.1152/ajplung.00396.2014.
Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial–mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15:178–96.
Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial–mesenchymal transitions in development and disease. Cell. 2009;139:871–90.
Yanez-Mo M, Lara-Pezzi E, Selgas R, Ramirez-Huesca M, Dominguez-Jimenez C, Jimenez-Heffernan JA, et al. Peritoneal dialysis and epithelial-to-mesenchymal transition of mesothelial cells. N Engl J Med. 2003;348:403–13.
Li Y, Wang J, Asahina K. Mesothelial cells give rise to hepatic stellate cells and myofibroblasts via mesothelial–mesenchymal transition in liver injury. Proc Natl Acad Sci USA. 2013;110:2324–9.
Suzuki A, Maeda T, Baba Y, Shimamura K, Kato Y. Acidic extracellular pH promotes epithelial mesenchymal transition in Lewis lung carcinoma model. Cancer Cell Int. 2014;14:129.
Itoigawa Y, Harada N, Harada S, Katsura Y, Makino F, Ito J, et al. TWEAK enhances TGF-beta-induced epithelial–mesenchymal transition in human bronchial epithelial cells. Respir Res. 2015;16:48.
Takeuchi H, Kitade M, Kikuchi I, Shimanuki H, Kumakiri J, Takeda S. Influencing factors of adhesion development and the efficacy of adhesion-preventing agents in patients undergoing laparoscopic myomectomy as evaluated by a second-look laparoscopy. Fertil Steril. 2008;89:1247–53.
Wiseman DM, Trout JR, Franklin RR, Diamond MP. Metaanalysis of the safety and efficacy of an adhesion barrier (Interceed TC7) in laparotomy. J Reprod Med. 1999;44:325–31.
ten Broek RP, Stommel MW, Strik C, van Laarhoven CJ, Keus F, van Goor H. Benefits and harms of adhesion barriers for abdominal surgery: a systematic review and meta-analysis. Lancet. 2014;383:48–59.
Laurens N, Koolwijk P, de Maat MP. Fibrin structure and wound healing. J Thromb Haemost JTH. 2006;4:932–9.
Acknowledgements
We thank Ms. Phyllis Minick for her excellent proofreading of our English writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors have nothing to disclose with regard to commercial support.
Conflict of interest
Ebana H. and the other co-authors have no conflicts of interests to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ebana, H., Hayashi, T., Mitani, K. et al. Oxidized regenerated cellulose induces pleural thickening in patients with pneumothorax: possible involvement of the mesothelial–mesenchymal transition. Surg Today 48, 462–472 (2018). https://doi.org/10.1007/s00595-017-1597-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-017-1597-4