Abstract
Purposes
Repeat hepatectomy remains the only curative treatment for recurrent colorectal liver metastasis (CLM) after primary hepatectomy. However, the repeat resection rate is still low, and there is insufficient data on the outcomes after repeat hepatectomy. The aim of this study was to investigate the feasibility and prognostic benefit of aggressive repeat hepatectomy for recurrent CLM.
Methods
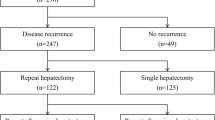
Data were reviewed from 282 consecutive patients who underwent primary curative hepatectomy for CLM between January 1994 and March 2015. The short- and long-term outcomes were analyzed.
Results
One hundred ninety-three patients (68 %) developed recurrence, and repeat hepatectomy was conducted in 62 patients. Overall, 62 s, 11 third, 4 fourth, and 1 fifth hepatectomies were performed. The postoperative morbidity and mortality rates were low (11.5 and 1.3 %, respectively). The overall survival rates at 3 and 5 years after primary hepatectomy for CLM in the repeat hepatectomy group were 79.5 and 57.4 %, respectively. A multivariate analysis indicated that postoperative complications were independently associated with overall survival after repeat hepatectomy.
Conclusions
Repeat hepatectomy for CLM is feasible, with acceptable rates of perioperative morbidity and mortality, and the potential for long-term survival. However, postoperative complications following aggressive repeat hepatectomy for CLM are associated with adverse oncological outcomes.

Similar content being viewed by others
References
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18.
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241:715–22.
Simmonds PC, Primrose JN, Colquitt JL, Garden OJ, Poston GJ, Rees M. Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer. 2006;94:982–99.
Are C, Gonen M, Zazzali K, Dematteo RP, Jarnagin WR, Fong Y, et al. The impact of margins on outcome after hepatic resection for colorectal metastasis. Ann Surg. 2007;246:295–300.
Muratore A, Ribero D, Zimmitti G, Mellano A, Langella S, Capussotti L. Resection margin and recurrence-free survival after liver resection of colorectal metastases. Ann Surg Oncol. 2010;17:1324–9.
Nordlinger B, Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371:1007–16.
Allen PJ, Kemeny N, Jarnagin W, DeMatteo R, Blumgart L, Fong Y. Importance of response to neoadjuvant chemotherapy in patients undergoing resection of synchronous colorectal liver metastases. J Gastrointest Surg. 2003;7:109–15.
Shindoh J, Tzeng CW, Aloia TA, Curley SA, Zimmitti G, Wei SH, et al. Portal vein embolization improves rate of resection of extensive colorectal liver metastases without worsening survival. Br J Surg. 2013;100:1777–83.
Wicherts DA, Miller R, de Haas RJ, Bitsakou G, Vibert E, Veilhan LA, et al. Long-term results of two-stage hepatectomy for irresectable colorectal cancer liver metastases. Ann Surg. 2008;248:994–1005.
Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255:405–14.
Fukami Y, Kurumiya Y, Kobayashi S. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): an analysis of tumor activity. Updates Surg. 2014;66:223–5.
Okuno M, Hatano E, Kasai Y, Nishio T, Seo S, Taura K, et al. Feasibility of the liver-first approach for patients with initially unresectable and not optimally resectable synchronous colorectal liver metastases. Surg Today. 2015 [Epub ahead of print].
Saiura A, Yamamoto J, Koga R, Takahashi Y, Takahashi M, Inoue Y, et al. Favorable outcome after repeat resection for colorectal liver metastases. Ann Surg Oncol. 2014;21:4293–9.
Wicherts DA, de Haas RJ, Salloum C, Andreani P, Pascal G, Sotirov D, et al. Repeat hepatectomy for recurrent colorectal metastases. Br J Surg. 2013;100:808–18.
Jones NB, McNally ME, Malhotra L, Abdel-Misih S, Martin EW, Bloomston M, et al. Repeat hepatectomy for metastatic colorectal cancer is safe but marginally effective. Ann Surg Oncol. 2012;19:2224–9.
Kulik U, Bektas H, Klempnauer J, Lehner F. Repeat liver resection for colorectal metastases. Br J Surg. 2013;100:926–32.
Battula N, Tsapralis D, Mayer D, Isaac J, Muiesan P, Sutcliffe RP, et al. Repeat liver resection for recurrent colorectal metastases: a single-centre, 13-year experience. HPB (Oxford). 2014;16:157–63.
Lam VW, Pang T, Laurence JM, Johnston E, Hollands MJ, Pleass HC, et al. A systematic review of repeat hepatectomy for recurrent colorectal liver metastases. J Gastrointest Surg. 2013;17:1312–21.
Stone MD, Cady B, Jenkins RL, McDermott WV, Steele GD Jr. Surgical therapy for recurrent liver metastases from colorectal cancer. Arch Surg. 1990;125:718–21.
Nordlinger B, Vaillant JC, Guiguet M, Balladur P, Paris F, Bachellier P, et al. Survival benefit of repeat liver resections for recurrent colorectal metastases: 143 cases. Association Francaise de Chirurgie. J Clin Oncol. 1994;12:1491–6.
Adam R, Bismuth H, Castaing D, Waechter F, Navarro F, Abascal A, et al. Repeat hepatectomy for colorectal liver metastases. Ann Surg. 1997;225:51–60.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–8.
International Union Against Cancer. TNM classification of malignant tumors. 7th ed. New York: Wiley-Liss; 2009.
Choti MA, Bowman HM, Pitt HA, Sosa JA, Sitzmann JV, Cameron JL, et al. Should hepatic resections be performed at high-volume referral centers? J Gastrointest Surg. 1998;2:11–20.
Shaw IM, Rees M, Welsh FK, Bygrave S, John TG. Repeat hepatic resection for recurrent colorectal liver metastases is associated with favourable long-term survival. Br J Surg. 2006;93:457–64.
Gold JS, Are C, Kornprat P, Jarnagin WR, Gönen M, Fong Y, et al. Increased use of parenchymal-sparing surgery for bilateral liver metastases from colorectal cancer is associated with improved mortality without change in oncologic outcome: trends in treatment over time in 440 patients. Ann Surg. 2008;247:109–17.
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C. Parenchymal-sparing hepatectomy in colorectal liver metastasis: improves salvageability and survival. Ann Surg. 2016; 263:146–152
Homayounfar K, Bleckmann A, Helms HJ, Lordick F, Rüschoff J, Conradi LC, et al. Discrepancies between medical oncologists and surgeons in assessment of resectability and indication for chemotherapy in patients with colorectal liver metastases. Br J Surg. 2014;101:550–7.
Petrowsky H, Gonen M, Jarnagin W, Lorenz M, DeMatteo R, Heinrich S, et al. Second liver resections are safe and effective treatment for recurrent hepatic metastases from colorectal cancer: a bi-institutional analysis. Ann Surg. 2002;235:863–71.
Yan TD, Lian KQ, Chang D, Morris DL. Management of intrahepatic recurrence after curative treatment of colorectal liver metastases. Br J Surg. 2006;93:854–9.
Thelen A, Jonas S, Benckert C, Schumacher G, Lopez-Hänninen E, Rudolph B, et al. Repeat liver resection for recurrent liver metastases from colorectal cancer. Eur J Surg Oncol. 2007;33:324–8.
Brachet D, Lermite E, Rouquette A, Lorimier G, Hamy A, Arnaud JP. Prognostic factors of survival in repeat liver resection for recurrent colorectal metastases: review of sixty-two cases treated at a single institution. Dis Colon Rectum. 2009;52:475–83.
Law WL, Choi HK, Lee YM, Ho JW. The impact of postoperative complications on long-term outcomes following curative resection for colorectal cancer. Ann Surg Oncol. 2007;14:2559–66.
Chok KS, Ng KK, Poon RT, Lo CM, Fan ST. Impact of postoperative complications on long-term outcome of curative resection for hepatocellular carcinoma. Br J Surg. 2009;96:81–7.
de Melo GM, Ribeiro KC, Kowalski LP, Deheinzelin D. Risk factors for postoperative complications in oral cancer and their prognostic implications. Arch Otolaryngol Head Neck Surg. 2001;127:828–33.
Rizk NP, Bach PB, Schrag D, Bains MS, Turnbull AD, Karpeh M, et al. The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg. 2004;198:42–50.
Farid SG, Aldouri A, Morris-Stiff G, Khan AZ, Toogood GJ, Lodge JP, et al. Correlation between postoperative infective complications and long-term outcomes after hepatic resection for colorectal liver metastasis. Ann Surg. 2010;251:91–100.
Mavros MN, de Jong M, Dogeas E, Hyder O, Pawlik TM. Impact of complications on long-term survival after resection of colorectal liver metastases. Br J Surg. 2013;100:711–8.
Matsuda A, Matsumoto S, Seya T, Matsutani T, Kishi T, Yokoi K, et al. Does postoperative complication have a negative impact on long-term outcomes following hepatic resection for colorectal liver metastasis?: a meta-analysis. Ann Surg Oncol. 2013;20:2485–92.
Kulaylat AN, Bhayani NH, Stokes AL, Schubart JR, Wong J, Kimchi ET, et al. Determinants of repeat curative intent surgery in colorectal liver metastasis. J Gastrointest Surg. 2014;18:1894–901.
Lundy J, Ford CM. Surgery, trauma and immune suppression. Evolving the mechanism. Ann Surg. 1983;197:434–8.
Horn F, Henze C, Heidrich K. Interleukin-6 signal transduction and lymphocyte function. Immunobiology. 2000;202:151–67.
Wong VK, Malik HZ, Hamady ZZ, Al-Mukhtar A, Gomez D, Prasad KR, et al. C-reactive protein as a predictor of prognosis following curative resection for colorectal liver metastases. Br J Cancer. 2007;96:222–5.
Folprecht G, Gruenberger T, Bechstein WO, Raab HR, Lordick F, Hartmann JT, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010;11:38–47.
Masi G, Loupakis F, Salvatore L, Fornaro L, Cremolini C, Cupini S, et al. Bevacizumab with FOLFOXIRI (irinotecan, oxaliplatin, fluorouracil, and folinate) as first-line treatment for metastatic colorectal cancer: a phase 2 trial. Lancet Oncol. 2010;11:845–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with this study.
Rights and permissions
About this article
Cite this article
Fukami, Y., Kaneoka, Y., Maeda, A. et al. Postoperative complications following aggressive repeat hepatectomy for colorectal liver metastasis have adverse oncological outcomes. Surg Today 47, 99–107 (2017). https://doi.org/10.1007/s00595-016-1340-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-016-1340-6