Abstract
Purpose
This study was undertaken to establish a model to predict the post-operative mortality for emergency surgeries.
Methods
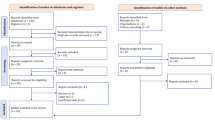
A regression model was constructed to predict in-hospital mortality using data from a cohort of 479 cases of emergency surgery performed in a Japanese referral hospital. The discrimination power of the current model termed the Calculation of post-Operative Risk in Emergency Surgery (CORES), and Portsmouth modification of the Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity (P-POSSUM) were validated using the area under the receiver operating characteristic curve (AUC) in another cohort of 494 cases in the same hospital (validation subset). We further evaluated the accuracy of the CORES in a cohort of 1,471 cases in six hospitals (multicenter subset).
Results
CORES requires only five preoperative variables, while the P-POSSUM requires 20 variables. In the validation subset, the CORES model had a similar discrimination power as the P-POSSUM for detecting in-hospital mortality (AUC, 95 % CI for CORES: 0.86, 0.80–0.93; for P-POSSUM: 0.88, 0.82–0.93). The predicted mortality rates of the CORES model significantly correlated with the severity of the post-operative complications. The subsequent multicenter study also demonstrated that the CORES model exhibited a high AUC value (0.85: 0.81–0.89) and a significant correlation with the post-operative morbidity.
Conclusions
This model for emergency surgery, the CORES, demonstrated a similar discriminatory power to the P-POSSUM in predicting post-operative mortality. However, the CORES model has a substantial advantage over the P-POSSUM in that it utilizes far fewer variables.





Similar content being viewed by others
References
Ingraham AM, Haas B, Cohen ME, Ko CY, Nathens AB. Comparison of hospital performance in trauma vs emergency and elective general surgery: implications for acute care surgery quality improvement. Arch Surg. 2012;147:591–8.
Koushi K, Korenaga D, Kawanaka H, Okuyama T, Ikeda Y, Takenaka K. Using the E-PASS scoring system to estimate the risk of emergency abdominal surgery in patients with acute gastrointestinal disease. Surg Today. 2011;41:1481–5.
Giraudo G, Baracchi F, Pellegrino L, Dal Corso HM, Borghi F. Prompt or delayed appendectomy? Influence of timing of surgery for acute appendicitis. Surg Today. 2013;43:392–6.
Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78:355–60.
Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ. POSSUM and Portsmouth POSSUM for predicting mortality. Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity. Br J Surg. 1998;85:1217–20.
Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA Jr, et al. Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the Private Sector: the patient safety in surgery study. Ann Surg. 2008;248:329–36.
Sjo OH, Larsen S, Lunde OC, Nesbakken A. Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis. 2009;11:733–9.
Kurki TS, Kataja M, Reich DL. Emergency and elective coronary artery bypass grafting: comparisons of risk profiles, postoperative outcomes, and resource requirements. J Cardiothorac Vasc Anesth. 2003;17:594–7.
Lemaire SA, Rice DC, Schmittling ZC. Emergency surgery for thoracoabdominal aortic aneurysms with acute presentation. J Vasc Surg. 2002;35:1171–8.
Cowan JA Jr, Dimick JB, Wainess RM, Upchurch GR Jr, Thompson BG. Outcomes after cerebral aneurysm clip occlusion in the United States: the need for evidence-based hospital referral. J Neurosurg. 2003;99:947–52.
Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Comparison of hospital performance in emergency versus elective general surgery operations at 198 hospitals. J Am Coll Surg. 2011;212:20–8.
Haga Y, Beppu T, Doi K, Nozawa F, Mugita N, Ikei S, et al. Systemic inflammatory response syndrome (SIRS) and organ dysfunction following gastrointestinal surgery. Crit Care Med. 1997;25:1994–2000.
Haga Y, Ikei S, Ogawa M. Estimation of physiologic ability and surgical stress (E-PASS) as a new prediction scoring system for postoperative morbidity and mortality following GI surgery. Surg Today. 1999;29:219–25.
Haga Y, Wada Y, Takeuchi H, Sameshima H, Kimura O, Furuya T. Estimation of surgical costs using a prediction scoring system estimation of physiologic ability and surgical stress. Arch Surg. 2002;137:481–5.
Haga Y, Wada Y, Takeuchi H, Kimura O, Furuya T, Sameshima H, et al. Estimation of physiologic ability and surgical stress (E-PASS) for a surgical audit in elective digestive surgery. Surgery. 2004;135:586–94.
Haga Y, Ikejiri K, Wada Y, Takahashi T, Ikenaga M, Akiyama N, et al. A multicenter prospective study of surgical audit systems. Ann Surg. 2011;253:194–201.
Oka Y, Nishijima J, Oku K, Azuma T, Inada K, Miyazaki S, et al. Usefulness of an estimation of physiologic ability and surgical stress (E-PASS) scoring system to predict the incidence of postoperative complications in gastrointestinal surgery. World J Surg. 2005;29:1029–33.
Yamashita S, Haga Y, Nemoto E, Nagai S, Ohta M. E-PASS (the estimation of physiological ability and surgical stress) scoring system helps the prediction of postoperative morbidity and mortality in thoracic surgery. Eur Surg Res. 2004;36:249–55.
Kotera A, Haga Y, Kei J, Okamoto M, Seo K. Evaluation of estimation of physiologic ability and surgical stress (E-PASS) to predict of in-hospital mortality in cardiac surgery. J Anesth. 2011;25:481–91.
Tang T, Walsh SR, Fanshawe TR, Gillard JH, Sadat U, Varty K, et al. Estimation of physiologic ability and surgical stress (E-PASS) as a predictor of immediate outcome after elective abdominal aortic aneurysm surgery. Am J Surg. 2007;194:176–82.
Hirose J, Mizuta H, Ide J, Nomura K. Evaluation of estimation of physiologic ability and surgical stress (E-PASS) to predict the postoperative risk for hip fracture in elder patients. Arch Orthop Trauma Surg. 2008;128:1447–52.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–9.
Ohta T, Kikuchi H, Hashi K, Kudo Y. Nizofenone administration in the acute stage following subarachnoid hemorrhage. Results of a multi-center controlled double-blind clinical study. J Neurosurg. 1986;64:420–6.
Namiki J, Yamazaki M, Funabiki T, Hori S, Aikawa N, et al. Problems of assessment of consciousness levels using GCS: Comparison to JCS assessment. Nippon Rinsyo Kyukyuigakukai Zasshi (J Jpn Society Emerg Med). 2007;10:20–5 (in Japanese).
Doglietto GB, Gallitelli L, Pacelli F, Bellantone R, Malerba M, Sgadari A, et al. Protein-sparing therapy after major abdominal surgery: lack of clinical effects. Ann Surg. 1996;223:357–62.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Hosmer DW, Lemeshow S. Summary measures of goodness-of-fit. In: Hosmer DW, Lemeshow S, editors. Applied logistic regression. 2nd ed. New York: Wiley; 2000. p. 144–67.
Wijesinghe LD, Mahmood T, Scott DJ, Berridge DC, Kent PJ, Kester RC. Comparison of POSSUM and the Portsmouth predictor equation for predicting death following vascular surgery. Br J Surg. 1998;85:209–12.
Moore FA, Moore EE. Evolving concepts in the pathogenesis of post injury multiple organ failure. Surg Clin North Am. 1995;75:257–77.
Tekkis PP, Kessaris N, Kocher HM, Poloniecki JD, Lyttle J, Windsor AC. Evaluation of POSSUM and P-POSSUM scoring systems in patients undergoing colorectal surgery. Br J Surg. 2003;90:340–5.
Bann SD, Sarin S. Comparative audit: the trouble with POSSUM. J R Soc Med. 2001;94:632–4.
Williamson DR, Lesur O, Tétrault JP, Nault V, Pilon D. Thrombocytopenia in the critically ill: prevalence, incidence, risk factors, and clinical outcomes. Can J Anaesth. 2013;. doi:10.1007/s12630-013-9933-7.
Shigematsu K, Nakano H, Watanabe Y. The eye response test alone is sufficient to predict stroke outcome–reintroduction of Japan Coma Scale: a cohort study. BMJ Open. 2013;3:4. doi:10.1136/bmjopen-2013-002736.
Acknowledgements
The authors have no financial support or conflict of interests with regard to this study. The authors wish to thank Professor Jonathan D. Kaunitz, M.D., UCLA School of Medicine, for his helpful comments. The authors also appreciate all of the institutional investigators listed below for collecting the patients’ data or coordinating the data collection: (1) Yoshikazu Haratake, M.D., Yoichiro Sakata, M.D., Kiyohiko Kato, M.D., Hiroko Iwamasa, M.D., Yuji Kunitoku, M.D., Kotaro Murakami, M.D., Ayako Haga, M.D., Yukiko Tokunaga, M.D., Taichi Kotani, M.D., Junya Matsumura, M.D. from Saiseikai Kumamoto Hospital. (2) Noriko Narimatsu, M.D., Takahiro Nonaka, M.D., Masahiro Hashimoto, M.D., Masahiro Onoda, M.D., Chiaki Ito, M.D., Tomoko Uehara, M.D. from Kumamoto Rosai Hospital. (3) Michiaki Sadanaga, M.D. from Japanese Red Cross Kumamoto Hospital. (4) Akihiko Tajiri, M.D. from Minamata City Hospital and Medical Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyazaki, N., Haga, Y., Matsukawa, H. et al. The development and validation of the Calculation of post-Operative Risk in Emergency Surgery (CORES) model. Surg Today 44, 1443–1456 (2014). https://doi.org/10.1007/s00595-013-0707-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-013-0707-1