Abstract
Aims
Currently, there is little and inconsistent evidence regarding the possible adverse effects of circulating levels of non-esterified fatty acids (NEFA) on kidney function decline in patients with type 2 diabetes mellitus (T2DM).
Methods
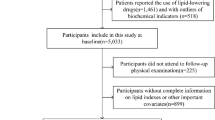
We followed for a median of 4.6 years 85 post-menopausal women with non-insulin-treated T2DM and preserved kidney function at baseline. Serum NEFA concentrations were measured using an enzymatic colorimetric method. Glomerular filtration rate (eGFR) was estimated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation.
Results
Enrolled patients had a baseline mean eGFRCKD-EPI of 83 ± 12 mL/min/1.73 m2 and a median serum NEFA concentration of 662 uEq/L (interquartile range 524–842 uEq/L). During the follow-up period, 13 patients developed kidney function decline at follow-up (defined as an eGFRCKD-EPI decline ≥ 30% from baseline). In Cox proportional hazards regression analyses, higher serum NEFA levels were significantly associated with an increased risk of developing kidney function decline (adjusted-hazard ratio 3.67, 95% CI 1.64–8.22, p < 0.001; for each 1-SD increment, i.e., 262 uEq/L), even after adjustment for waist circumference, hemoglobin A1c, C-reactive protein, HOMA-estimated insulin resistance, hypertension, dyslipidemia, microalbuminuria, baseline eGFRCKD-EPI, as well as temporal changes in HbA1c levels or the use of renin-angiotensin system inhibitors over the follow-up.
Conclusions
The findings of this exploratory prospective study show that in post-menopausal women with T2DM and preserved kidney function at baseline, higher circulating levels of NEFA were strongly associated with a faster kidney function decline, even after adjustment for established renal risk factors and potential confounders.

Similar content being viewed by others
Data availability
Restrictions apply to the availability of some or all data generated or analyzed during this study to preserve patient confidentiality or because they were used under license. The corresponding author will, on request, detail the restrictions and any conditions under which access to some data may be provided.
References
Ebbert JO, Jensen MD (2013) Fat depots, free fatty acids, and dyslipidemia. Nutrients 5:498–508
Miles JM, Nelson RH (2007) Contribution of triglyceride-rich lipoproteins to plasma free fatty acids. Horm Metab Res 39:726–729
Lowell BB, Shulman GI (2005) Mitochondrial dysfunction and type 2 diabetes. Science 307:384–387
Delarue J, Magnan C (2007) Free fatty acids and insulin resistance. Curr Opin Clin Nutr Metab Care 10:142–148
Weinberg JM (2006) Lipotoxicity. Kidney Int 70:1560–1566
Sieber J, Lindenmeyer MT, Kampe K et al (2010) Regulation of podocyte survival and endoplasmic reticulum stress by fatty acids. Am J Physiol Renal Physiol 299:F821–F829
Djousse L, Khawaja O, Bartz TM et al (2012) Plasma fatty acid-binding protein 4, nonesterified fatty acids, and incident diabetes in older adults. Diabetes Care 35:1701–1707
Pankow JS, Duncan BB, Schmidt MI et al (2004) Fasting plasma free fatty acids and risk of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes Care 27:77–82
Khawaja O, Bartz TM, Ix JH et al (2012) Plasma free fatty acids and risk of atrial fibrillation (from the cardiovascular health study). Am J Cardiol 110:212–216
Djousse L, Benkeser D, Arnold A et al (2013) Plasma free fatty acids and risk of heart failure: the cardiovascular health study. Circ Heart Fail 6:964–969
Xiong Z, Xu H, Huang X et al (2015) Nonesterified fatty acids and cardiovascular mortality in elderly men with CKD. Clin J Am Soc Nephrol 10:584–591
Walther CP, Ix JH, Biggs ML et al (2021) Nonesterified fatty acids and kidney function decline in older adults: findings from the cardiovascular health study. Am J Kidney Dis 78:259–267
Duranton F, Laget J, Gayrard N et al (2019) The CKD plasma lipidome varies with disease severity and outcome. J Clin Lipidol 13(176–85):e8
Baek J, He C, Afshinnia F et al (2022) Lipidomic approaches to dissect dysregulated lipid metabolism in kidney disease. Nat Rev Nephrol 18:38–55
Webster AC, Nagler EV, Morton RL et al (2017) Chronic kidney disease. Lancet 389:1238–1252
Romagnani P, Remuzzi G, Glassock R et al (2017) Chronic kidney disease. Nat Rev Dis Primers 3:17088
Kalantar-Zadeh K, Jafar TH, Nitsch D et al (2021) Chronic kidney disease. Lancet 398:786–802
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Kerschbaum J, Rudnicki M, Dzien A et al (2020) Intra-individual variability of eGFR trajectories in early diabetic kidney disease and lack of performance of prognostic biomarkers. Sci Rep 10:19743
Lambers Heerspink HJ, Tighiouart H, Sang Y et al (2014) GFR decline and subsequent risk of established kidney outcomes: a meta-analysis of 37 randomized controlled trials. Am J Kidney Dis 64:860–866
Koska J, Gerstein HC, Beisswenger PJ et al (2022) Advanced glycation end products predict loss of renal function and high-risk chronic kidney disease in type 2 diabetes. Diabetes Care 45:684–691
Wirthensohn G, Guder WG (1983) Renal lipid metabolism. Miner Electrolyte Metab 9:203–211
Lennon R, Pons D, Sabin MA et al (2009) Saturated fatty acids induce insulin resistance in human podocytes: implications for diabetic nephropathy. Nephrol Dial Transpl 24:3288–3296
D’Agati VD, Chagnac A, de Vries AP et al (2016) Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol 12:453–471
Despres JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444:881–887
Clement LC, Avila-Casado C, Mace C et al (2011) Podocyte-secreted angiopoietin-like-4 mediates proteinuria in glucocorticoid-sensitive nephrotic syndrome. Nat Med 17:117–122
Turolo S, Edefonti A, Syren ML et al (2018) Fatty acids in nephrotic syndrome and chronic kidney disease. J Ren Nutr 28:145–155
Afshinnia F, Rajendiran TM, He C et al (2021) Circulating free fatty acid and phospholipid signature predicts early rapid kidney function decline in patients with type 1 diabetes. Diabetes Care 44:2098–2106
Afshinnia F, Nair V, Lin J et al (2019) Increased lipogenesis and impaired beta-oxidation predict type 2 diabetic kidney disease progression in American Indians. JCI Insight 4:e130317
Nagata M (2016) Podocyte injury and its consequences. Kidney Int 89:1221–1230
de Vries AP, Ruggenenti P, Ruan XZ et al (2014) Fatty kidney: emerging role of ectopic lipid in obesity-related renal disease. Lancet Diabetes Endocrinol 2:417–426
Ko SH, Kim HS (2020) Menopause-associated lipid metabolic disorders and foods beneficial for postmenopausal women. Nutrients 12:202
Funding
GT is partly supported by grants from the University School of Medicine of Verona, Verona, Italy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors do not have any conflicts of interest to declare.
Ethical approval
The study was performed according to the Declaration of Helsinki. The local Ethics Committee approved the study protocol. All participants gave their written informed consent for participation in this research.
Additional information
This article belongs to the Topical Collection “Diabetic Nephropathy”, managed by Giuseppe Pugliese.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mantovani, A., Csermely, A., Cappelli, D. et al. Higher circulating levels of non-esterified fatty acids are associated with faster kidney function decline in post-menopausal women with type 2 diabetes: a pilot prospective study. Acta Diabetol 61, 281–288 (2024). https://doi.org/10.1007/s00592-023-02198-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02198-6