Abstract
Aims
To investigate the lowering BP effects of sodium glucose cotransporter 2 inhibitors (SGLT2i) and glucagon-like peptide 1 receptor agonists (GLP-1 RAs) on the risk of major cardiovascular event stratified by glucose-lowering drugs, baseline BP, glycated hemoglobin (HbA1c), and history of cardiovascular disease in patients with type 2 diabetes.
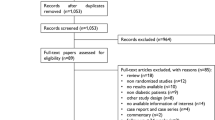
Methods
We performed a systematic review of the MEDLINE and EMBASE databases search up to December 31, 2022, (PROSPERO, CRD42023400899) to identify all large-scale cardiovascular outcomes (CVO) trials of SGLT2i and GLP-1 RAs in which more than 1,000 patient-years of follow-up in each randomized group. Outcomes included all-cause mortality, major adverse cardiovascular event (MACE) and its component (cardiovascular death, myocardial infarction [MI], and stroke), heart failure, and renal failure. A random-effects meta-analyses were used to pool the estimates.
Results
Eighteen CVOTs (ten for SGLT2i and eight for GLP-1 RAs) with 127,606 patients with type 2 diabetes were included. Over 2.5 years median follow-up, the average reduction of systolic BP was 2.2 mmHg (mean difference [MD] − 2.2; 95% CI − 2.7 to − 1.7) with more important reduction (Pinteraction = 0.001) with SGLT2 inhibitors (− 2.9; − 3.4 to − 2.5) than with GLP-1 RAs (− 1.4; − 1.8 to − 1). With SGLT2i, every 5-mmHg reduction in systolic BP was associated with a significantly lower risk of mortality (hazard ratio[HR], 0.77; 95% CI 0.65–0.90), MACE (HR 0.81 [0.74–0.89]), cardiovascular death (HR 0.72 [0.59–0.88]), MI (HR 0.82 [0.71–0.95]), heart failure (HR 0.49 [0.42–0.57]), and renal failure (HR 0.46 [0.38–0.55]), while the association was not significant for stroke (HR 0.91 [0.69–1.19]). The corresponding effects for every 5-mmHg reduction in SBP with GLP-1 RAs were 0.65 (0.51–0.84) for all-cause mortality, 0.65 (0.56–0.76) for MACE, 0.62 (0.45–0.85) for CV death, 0.71 (0.52–0.76) for MI, 0.49 (0.35–0.69) for stroke, and 0.49 (0.35–0.66) for renal failure, while the association was not significant for heart failure (HR 0.82 [0.63–1.08]).
Conclusion
In patients with type 2 diabetes, the hypotensive effects of SGLT2i and GLP-1 RAs were significantly associated with a reduction in mortality and cardiorenal events. These findings suggest that the lowering BP effect could be seen as an additive indicator of cardiovascular protection by SGLT2i and GLP-1 RAs drugs.


Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request (alhassane.diallo@umontpellier.fr).
References
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X et al (2020) Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep 10(1):14790
Yamada T, Wakabayashi M, Bhalla A, Chopra N, Miyashita H, Mikami T et al (2021) Cardiovascular and renal outcomes with SGLT-2 inhibitors versus GLP-1 receptor agonists in patients with type 2 diabetes mellitus and chronic kidney disease: a systematic review and network meta-analysis. Cardiovasc Diabetol déc 20(1):14
Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS et al (2021) Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol 9(10):653–662
Nazarzadeh M, Bidel Z, Canoy D, Copland E, Bennett DA, Dehghan A et al (2022) Blood pressure-lowering treatment for prevention of major cardiovascular diseases in people with and without type 2 diabetes: an individual participant-level data meta-analysis. Lancet Diabetes Endocrinol 10(9):645–654
Georgianos PI, Agarwal R (2019) Ambulatory blood pressure reduction with SGLT-2 inhibitors: dose-response meta-analysis and comparative evaluation with low-dose hydrochlorothiazide. Diabetes Care 42(4):693–700
Wang B, Zhong J, Lin H, Zhao Z, Yan Z, He H et al (2013) Blood pressure-lowering effects of GLP-1 receptor agonists exenatide and liraglutide: a meta-analysis of clinical trials. Diabetes Obes Metab août 15(8):737–749
Liakos CI, Papadopoulos DP, Sanidas EA, Markou MI, Hatziagelaki EE, Grassos CA et al (2021) Blood pressure-lowering effect of newer antihyperglycemic agents (SGLT-2 Inhibitors, GLP-1 receptor agonists, and DPP-4 inhibitors). Am J Cardiovasc Drugs mars 21(2):123–137
Packer M (2020) SGLT2 inhibitors produce cardiorenal benefits by promoting adaptive cellular reprogramming to induce a state of fasting mimicry: a paradigm shift in understanding their mechanism of action. Diabetes Care 43(3):508–511
Packer M, Anker SD, Butler J, Filippatos G, Zannad F (2017) Effects of sodium-glucose cotransporter 2 inhibitors for the treatment of patients with heart failure: proposal of a novel mechanism of action. JAMA Cardiol 2(9):1025
Verma S, McMurray JJV (2018) SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia 61(10):2108–2117
Bonnet F, Scheen AJ (2018) Effects of SGLT2 inhibitors on systemic and tissue low-grade inflammation: the potential contribution to diabetes complications and cardiovascular disease. Diabetes Metab déc 44(6):457–464
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Rohatgi A (2021) WebPlotDigitize. Pacifica, California
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. https://doi.org/10.1136/bmj.l4898
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A (2015) Blood pressure lowering in Type 2 diabetes: a systematic review and meta-analysis. JAMA 313(6):603
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J et al (2016) Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet mars 387(10022):957–967
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al (2022) Cochrane Handbook for Systematic Reviews of Interventions [Internet], 1re éd. Wiley, New York. [cité 6 août 2022]. Disponible sur: https://doi.org/10.1002/9781119536604
Husain M, Birkenfeld AL, Donsmark M, Dungan K, Eliaschewitz FG, Franco DR et al (2019) Oral semaglutide and cardiovascular outcomes in patients with Type 2 diabetes. N Engl J Med 381(9):841–851
Hernandez AF, Green JB, Janmohamed S, D’Agostino RB, Granger CB, Jones NP et al (2018) Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. The Lancet 392(10157):1519–1529
Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Køber LV et al (2015) Lixisenatide in patients with Type 2 diabetes and acute coronary syndrome. N Engl J Med 373(23):2247–2257
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med 373(22):2117–2128
Mann JFE, Ørsted DD, Brown-Frandsen K, Marso SP, Poulter NR, Rasmussen S et al (2017) Liraglutide and renal outcomes in Type 2 diabetes. N Engl J Med 377(9):839–848
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA et al (2016) Semaglutide and cardiovascular outcomes in patients with Type 2 diabetes. N Engl J Med 375(19):1834–1844
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N et al (2017) Canagliflozin and cardiovascular and renal events in Type 2 diabetes. N Engl J Med 377(7):644–657
Holman RR, Bethel MA, Mentz RJ, Thompson VP, Lokhnygina Y, Buse JB et al (2017) Effects of once-weekly exenatide on cardiovascular outcomes in Type 2 diabetes. N Engl J Med 377(13):1228–1239
Gerstein HC, Sattar N, Rosenstock J, Ramasundarahettige C, Pratley R, Lopes RD et al (2021) Cardiovascular and renal outcomes with efpeglenatide in Type 2 diabetes. N Engl J Med 385(10):896–907
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A et al (2019) Dapagliflozin and cardiovascular outcomes in Type 2 diabetes. N Engl J Med 380(4):347–357
Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P et al (2019) Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet juill 394(10193):121–130
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM et al (2019) Canagliflozin and renal outcomes in Type 2 diabetes and nephropathy. N Engl J Med 380(24):2295–2306
Bhatt DL, Szarek M, Pitt B, Cannon CP, Leiter LA, McGuire DK et al (2021) Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med 384(2):129–139
Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U et al (2020) Cardiovascular outcomes with ertugliflozin in Type 2 diabetes. N Engl J Med 383(15):1425–1435
McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA et al (2019) Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 381(21):1995–2008
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M et al (2021) Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 385(16):1451–1461
The EMPA-KIDNEY Collaborative Group (2023) Empagliflozin in patients with chronic kidney disease. N Engl J Med 388(2):117–127
Solomon SD, McMurray JJV, Claggett B, de Boer RA, DeMets D, Hernandez AF et al (2022) Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med 387(12):1089–1098
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P et al (2020) Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med 383(15):1413–1424
Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA et al (2010) Effects of intensive blood-pressure control in Type 2 diabetes mellitus. N Engl J Med 362(17):1575–1585
Acknowledgements
None.
Funding
No funding source was involved to the data collection, statistical analyses, and writing of the manuscript.
Author information
Authors and Affiliations
Contributions
AD conceived the study design, analyzed the data, and drafted the first version of the manuscript; MCB involved in supervision of data collection and critical revision of the manuscript; and FG interpreted and substantially revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
AD, MCB, and FG declare no competing interests. The authors declare no financial relationships with any organizations that might have an interest in the submitted work, no other relationships or activities that could appear to have influenced the submitted work.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors approved the final version of the manuscript for publication.
Additional information
Managed by Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Diallo, A., Carlos-Bolumbu, M. & Galtier, F. Blood pressure-lowering effects of SGLT2 inhibitors and GLP-1 receptor agonists for preventing of cardiovascular events and death in type 2 diabetes: a systematic review and meta-analysis. Acta Diabetol 60, 1651–1662 (2023). https://doi.org/10.1007/s00592-023-02154-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02154-4