Abstract
Background
Psychosocial factors like diabetes distress and social support, as well as the presence of complications, affect an individual’s self-management ability; however, their role in adherence behaviours is not yet clear. We examined the role of psychosocial factors and complications in non-adherence behaviours in individuals with diabetes in primary care.
Methods
Baseline survey with nine-month follow up through medical records of patients with type 2 diabetes attending primary care. Medication adherence and diabetes distress were assessed using Morisky Green Levine Medication Adherence Scale and Problem Areas in Diabetes, respectively. Appointment adherence was assessed through medical records.
Results
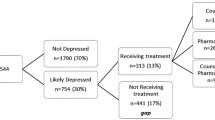
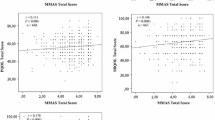
Of the 448 participants studied, 59.8% had medication non-adherence and 21.7% were non-adherent to scheduled appointments. PAID score (odds ratio (OR) 1.01, 95% confidence interval 1.00–1.03, p = 0.013), peripheral neuropathy (OR 1.99, 95%CI 1.18–3.37, p = 0.01), home glucose monitoring (OR 0.46, 95%CI 0.30–0.69, p < 0.001), HbA1c (OR 1.34, 95%CI 1.13–1.61, p = 0.001), and age (OR 0.96, 95%CI 0.93–0.98, p = 0.001) were associated with medication non-adherence. Indian ethnicity (OR 2.93, 95%CI 1.59–5.39, p = 0.001), secondary or higher education (OR 1.94, 95%CI 1.14–3.27, p = 0.014), and HbA1c (OR 1.38, 95%CI 1.18–1.63, p < 0.001) were associated with appointment non-adherence.
Conclusions
Non-adherence behaviours were prevalent and significantly associated with higher HbA1c. Medication non-adherence was more likely in younger individuals, those with higher diabetes distress or peripheral neuropathy. Appointment non-adherence was more likely in individuals of Indian ethnicity or those with higher education. Greater support for these groups may help improve adherence behaviours and outcomes.

Similar content being viewed by others
References
Schectman JM, Schorling JB, Voss JD (2008) Appointment adherence and disparities in outcomes among patients with diabetes. J Gen Intern Med 23(10):1685–1687. https://doi.org/10.1007/s11606-008-0747-1
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group (1998). Lancet (London, England) 352(9131) 837–853
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. New Engl J Med 359(15):1577–1589. https://doi.org/10.1056/NEJMoa0806470
Giugliano D, Maiorino MI, Bellastella G, Esposito K (2018) Glycemic control in type 2 diabetes: from medication nonadherence to residual vascular risk. Endocrine 61(1):23–27. https://doi.org/10.1007/s12020-017-1517-9
Karter AJ, Parker MM, Moffet HH, Ahmed AT, Ferrara A, Liu JY, Selby JV (2004) Missed appointments and poor glycemic control: an opportunity to identify high-risk diabetic patients. Med Care 42(2):110–115. https://doi.org/10.1097/01.mlr.0000109023.64650.73
Griffin SJ (1998) Lost to follow-up: the problem of defaulters from diabetes clinics. Diabet Med J Br Diabet Assoc 15(Suppl 3):S14–24. https://doi.org/10.1002/(sici)1096-9136(1998110)15:3+<s14:aid-dia725>3.3.co;2-9
McQueenie R, Ellis DA, McConnachie A, Wilson P, Williamson AE (2019) Morbidity, mortality and missed appointments in healthcare: a national retrospective data linkage study. BMC Med 17(1):2. https://doi.org/10.1186/s12916-018-1234-0
Krass I, Schieback P, Dhippayom T (2015) Adherence to diabetes medication: a systematic review. Diabetic Med J Br Diabet Assoc 32(6):725–737. https://doi.org/10.1111/dme.12651
Brewster S, Bartholomew J, Holt RIG, Price H (2020) Non-attendance at diabetes outpatient appointments: a systematic review. Diabet Med J Br Diabet Assoc. https://doi.org/10.1111/dme.14241
Capoccia K, Odegard PS, Letassy N (2016) Medication adherence with diabetes medication: a systematic review of the literature. Diabet Educ 42(1):34–71. https://doi.org/10.1177/0145721715619038
Shahin W, Kennedy GA, Stupans I (2019) The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient Preference Adher 13:1019–1035. https://doi.org/10.2147/ppa.S212046
Lee RRS, Samsudin MI, Thirumoorthy T, Low LL, Kwan YH (2019) Factors affecting follow-up non-attendance in patients with type 2 diabetes mellitus and hypertension: a systematic review. Singap Med J 60(5):216–223. https://doi.org/10.11622/smedj.2019042
Lin LK, Sun Y, Heng BH, Chew DEK, Chong PN (2017) Medication adherence and glycemic control among newly diagnosed diabetes patients. BMJ Open Diabet Res Care 5(1):e000429. https://doi.org/10.1136/bmjdrc-2017-000429
Lee CS, Tan JHM, Sankari U, Koh YLE, Tan NC (2017) Assessing oral medication adherence among patients with type 2 diabetes mellitus treated with polytherapy in a developed Asian community: a cross-sectional study. BMJ open 7(9):e016317. https://doi.org/10.1136/bmjopen-2017-016317
Low SK, Khoo JK, Tavintharan S, Lim SC, Sum CF (2016) Missed appointments at a diabetes centre: not a small problem. Ann Acad Med Singap 45(1):1–5
Aikens JE (2012) Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabet Care 35(12):2472–2478. https://doi.org/10.2337/dc12-0181
Saffari M, Lin CY, Chen H, Pakpour AH (2019) The role of religious coping and social support on medication adherence and quality of life among the elderly with type 2 diabetes. Qual Life Res Int J Qual Life Asp Treat Care Rehabilit 28(8):2183–2193. https://doi.org/10.1007/s11136-019-02183-z
Munger MA (2010) Polypharmacy and combination therapy in the management of hypertension in elderly patients with co-morbid diabetes mellitus. Drugs Aging 27(11):871–883. https://doi.org/10.2165/11538650-000000000-00000
WHO (2006) Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia : report of a WHO/IDF consultation. World Health Organization, Geneva, Switzerland
Nguyen TM, La Caze A, Cottrell N (2016) Validated adherence scales used in a measurement-guided medication management approach to target and tailor a medication adherence intervention: a randomised controlled trial. BMJ open 6(11):e013375. https://doi.org/10.1136/bmjopen-2016-013375
Hill-Briggs F, Gary TL, Bone LR, Hill MN, Levine DM, Brancati FL (2005) Medication adherence and diabetes control in urban African Americans with type 2 diabetes. Health Psychol Off J Div Health Psychol, Am Psychol Assoc 24(4):349–357. https://doi.org/10.1037/0278-6133.24.4.349
Venkataraman K, Tan LS, Bautista DC, Griva K, Zuniga YL, Amir M, Lee YS, Lee J, Tai ES, Khoo EY, Wee HL (2015) Psychometric properties of the problem areas in diabetes (PAID) instrument in Singapore. PLoS ONE 10(9):e0136759. https://doi.org/10.1371/journal.pone.0136759
Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH (1988) The Duke-UNC functional social support questionnaire measurement of social support in family medicine patients. Med Care 26(7):709–723. https://doi.org/10.1097/00005650-198807000-00006
Gonzalez JS, Kane NS, Binko DH, Shapira A, Hoogendoorn CJ (2016) Tangled up in blue: unraveling the links between emotional distress and treatment adherence in type 2 diabetes. Diabet Care 39(12):2182–2189. https://doi.org/10.2337/dc16-1657
Venkataraman K, Khoo C, Wee HL, Tan CS, Ma S, Heng D, Lee J, Tai ES, Thumboo J (2014) Associations between disease awareness and health-related quality of life in a multi-ethnic Asian population. PLoS ONE 9(11):e113802. https://doi.org/10.1371/journal.pone.0113802
Tiv M, Viel JF, Mauny F, Eschwège E, Weill A, Fournier C, Fagot-Campagna A, Penfornis A (2012) Medication adherence in type 2 diabetes: the ENTRED study 2007, a french population-based study. PLoS ONE 7(3):e32412. https://doi.org/10.1371/journal.pone.0032412
Cohen HW, Shmukler C, Ullman R, Rivera CM, Walker EA (2010) Measurements of medication adherence in diabetic patients with poorly controlled HbA(1c). Diabet Med J Br Diabet Assoc 27(2):210–216. https://doi.org/10.1111/j.1464-5491.2009.02898.x
Aikens JE, Piette JD (2013) Longitudinal association between medication adherence and glycaemic control in type 2 diabetes. Diabet Med J Br Diabet Assoc 30(3):338–344. https://doi.org/10.1111/dme.12046
García Díaz E, Ramírez Medina D, García López A, Morera Porras ÓM (2017) Determinants of adherence to hypoglycemic agents and medical visits in patients with type 2 diabetes mellitus. Endocrinol, Diabet y Nutr 64(10):531–538. https://doi.org/10.1016/j.endinu.2017.08.004
Luo M, Tan KHX, Tan CS, Lim WY, Tai ES, Venkataraman K (2018) Longitudinal trends in HbA(1c) patterns and association with outcomes: a systematic review. Diabet/metab Res Rev 34(6):e3015. https://doi.org/10.1002/dmrr.3015
Venkataraman K, Wee HL, Leow MK, Tai ES, Lee J, Lim SC, Tavintharan S, Wong TY, Ma S, Heng D, Thumboo J (2013) Associations between complications and health-related quality of life in individuals with diabetes. Clin Endocrinol 78(6):865–873. https://doi.org/10.1111/j.1365-2265.2012.04480.x
Riandini T, Wee HL, Khoo EYH, Tai BC, Wang W, Koh GCH, Tai ES, Tavintharan S, Chandran K, Hwang SW, Venkataraman K (2018) Functional status mediates the association between peripheral neuropathy and health-related quality of life in individuals with diabetes. Acta Diabetol 55(2):155–164. https://doi.org/10.1007/s00592-017-1077-8
Timar B, Timar R, Schiller A, Oancea C, Roman D, Vlad M, Balinisteanu B, Mazilu O (2016) Impact of neuropathy on the adherence to diabetes-related self-care activities: a cross-sectional study. Patient Preference Adher 10:1169–1175. https://doi.org/10.2147/ppa.S107621
Luo M, Lim WY, Tan CS, Ning Y, Chia KS, van Dam RM, Tang WE, Tan NC, Chen R, Tai ES, Venkataraman K (2017) Longitudinal trends in HbA1c and associations with comorbidity and all-cause mortality in Asian patients with type 2 diabetes: a cohort study. Diabet Res Clin Pract 133:69–77. https://doi.org/10.1016/j.diabres.2017.08.013
Chua L, Soh I (2016) Health status and health-related behaviours in adults with self-reported diabetes. Statistics singapore newsletter september:5–9
Acknowledgements
The authors would like to acknowledge the help and support of Dr Richard Hui and Dr Kwek Sing Cheer from National University Polyclinics and the staff from Department of Family Medicine Development, National University Polyclinics.
Funding
This study was not funded.
Author information
Authors and Affiliations
Author notes
Zhi Peng Zhang and M. Premikha have contributed equally to this work and are joint first authors.
This article belongs to the topical collection Health Education and Psycho-Social Aspects, managed by Massimo Porta and Marina Trento.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
National Healthcare Group Domain Specific Review Board.
Consent to participate
All participants provided written informed consent prior to participation.
Availability of data
The datasets generated during and/or analysed during the current study are not publicly available due to concerns about data confidentiality but are available from the corresponding author on reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Health Education and Psycho-Social Aspects, managed by Massimo Porta and Marina Trento.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Z.P., Premikha, M., Luo, M. et al. Diabetes distress and peripheral neuropathy are associated with medication non-adherence in individuals with type 2 diabetes in primary care. Acta Diabetol 58, 309–317 (2021). https://doi.org/10.1007/s00592-020-01609-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-020-01609-2