Abstract
Aim
Infection of a diabetic foot ulcer (DFU) is common. More than the half of DFUs become infected and 15–20% of them necessitate amputation in course of treatment. Diabetic foot infection (DFI) is therefore the major cause for non-traumatic lower limb amputation in Germany. Prompt and effective treatment of DFI is mandatory to safe limbs and lives. We investigated if there are relevant differences in evoked inflammatory response between different species and age-separated groups. We further investigated if there is an impact of ulcer localization on bacterial diversity.
Methods
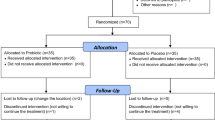
For a 12-month period, we investigated 353 individuals with infected DFU, their laboratory results and bacterial diversity at first-time visit in a Diabetic Foot Care Center in Southern Germany.
Results
The ulcer microbiota was dominated by gram-positive species, primary Staphylococcus aureus. The gram-negative sector was mainly formed by Pseudomonas aeruginosa and Enterobacteriaceae (Proteus spp., Enterobacter spp., Escherichia coli and Klebsiella spp.). With increase in age, P. aeruginosa and S. aureus became more frequent, while Streptococci decreased. Ischemic and/or deep wounds were more likely to bear gram-negative species. Inflammatory response did not differ between gram-positive and gram-negative species, while Streptococci and Proteus spp. induced the highest serum inflammation reaction in their category. Streptococci, Enterobacter spp. and E. coli were more frequent in summer, while Enterococci spp., coagulase-negative Staphylococci and P. aeruginosa were more prevalent in winter half-year. DFIs of the forefoot and plantar side are mostly caused by gram-positive species, while Enterobacteriaceae were most frequent in plantar ulcerations.
Conclusion
Gram-positive species dominate bacterial spectrum in DFI. With increase in age, S. aureus, Streptococci and Pseudomonas aeruginosa became more frequent. The inflammatory response did not differ significantly between different species, but gram-negative species were slightly but not significant more frequent in ischemic wounds. Climatic distinction like summer or winter half-year as well as foot ulcer localization seems to influence bacterial diversity in DFUs.





Similar content being viewed by others
Abbreviations
- DFU:
-
Diabetic foot ulcer
- DFI:
-
Diabetic foot infection
- S. aureus:
-
Staphylococcus aureus
- P. aeruginosa:
-
Pseudomonas aeruginosa
- E. coli:
-
Escherichia coli
- CONS:
-
Coagulase-negative Staphylococci
References
International Diabetes Federation. Recommendations For Managing Type 2 Diabetes In Primary Care, 2017. http://www.idf.org/managing-type2-diabetes
Machado C, Teixeira S, Fonseca L et al (2020) Evolutionary trends in bacteria isolated from moderate and severe diabetic foot infections in a Portuguese tertiary center. Diab Metabol Syn. https://doi.org/10.1016/j.dsx.2020.02.010
Skrepnek GH, Mills JL Sr, Armstrong DG (2015) A diabetic emergency one million feet long: disparities and burdens of illness among diabetic foot ulcer cases within emergency departments in the United States 2006–2010. PLoS ONE 10:e0134914
Apelqvist J, Larsson J, Agardh CD (1993) Long-term patients with foot ulcers. J Intern Med 233:485–491
Armstrong DG, Boulton AJM, Bus SA (2017) Diabetic foot ulcers and their recurrence. NEJM 376:2367–2375
Brownrigg JWR, Davey J, Holt PJ, Davis WA, Thompson MM, Ray KK (2012) The association of ulceration of the foot with cardiovascular and all-cause mortality in patients with diabetes: a meta-analysis. Diabetologia 55:2906–2912
Malone M, Nau NS, White J (2014) The effect of diabetes mellitus on costs and length of stay in patients with peripheral arterial disease undergoing vascular surgery. Eur J Vasc Endovasc Surg 48:447–451
Vileikyte L, Rubin RR, Leventhal H (2004) Psychological aspects of diabetic neuropathic foot complications: an review. Diabetes Metab Res Rev 20(Suppl. 1):S13–18
Dörr S, Friedl A, Lobmann R (2019) Differences in microbial spectrum and antibiotic resistance between old and aged people with infected diabetic foot syndrome (DFS). Geriatric 1(1):1
Lawall H, Lobmann R (2019) Das Diabetische Fußsyndrom: aktuelle Entwicklungen, Therapieziele und Zweitmeinung. Deutscher Gesundheitsbericht. Diabetes 2019:66–69
Jneid J, Cassir N, Schuldinger S et al (2018) Exploring the microbiota of diabetic foot infections with culturomics. Front Cell Infect Microbiol 8:282
Benwan Al K, Mulla Al A, Rotini VO (2012) A study of the microbiology of diabetic foot infections in a teaching hospital in Kuwait. J Infect PUblic Health 5:1–8
Benotmane A, Mohammedi F, Ayad F, Kadi K, Azzouz A (2000) Diabetic foot lesions: etiologic and prognostic factors. Diabetes Metabol 26(2):113–117
Pemayun TGD, Naibaho RM (2016) Diabetic foot ulcer registry at a tertiary care hospital in semarang, indonesia: an overview of its clinical profile and management outcome. J Clin Diabetes Pract 1:111
Hatipoglu M, Mutluoglu M, Turhan V, Uzun G, Lipsky BA (2016) Causative pathogens and antibiotic resistance in diabetic foot infections: a prospective multi-center study. J Diabetes Complicat 30(5):910–916
Xie X, Bao Y, Ni L, Liu D, Niu S, Lin H (2017) Bacterial profile and antibiotic resistance in patients with diabetic foot ulcer in Guangzhou (Southern China): focus on the differences among different Wagner's Grades, IDSA/IWGDF grades, and Ulcer types. Int J Endocrinol. https://doi.org/10.1155/2017/8694903
Macdonald KE, Jordan CY, Crichton E et al (2020) A retrospective analysis of the microbiology of diabetic foot infections at a Scottish tertiary hospital. BMC Infect Dis 20:218. https://doi.org/10.1186/s12879-020-4923-1
Dörr S, Schlecht M, Chatzitomaris A et al (2020) Predictive effect of inflammatory response and foot ulcer localization on outcome in younger and older individuals with infected diabetic foot syndrome. Exp Clin Endocrinol Diabetes 128:1–9. https://doi.org/10.1055/a-1149-8989
Victoria von Asten SA, Geradus Peters EJ, Xi Y, Lavery LA (2016) The role of biomarkers to diagnose diabetic foot osteomyelitis. A Meta-analysis Curr Diabetes Res 12(4):396–402
Victoria van Asten SA, Nichols A, La Fontaine J, Peters EJ, Lavery LA (2017) The value of inflammatory markers to diagnose and monitor diabetic foot osteomyelitis. Int Wound J 14(1):40–45
Victoria van Asten SA, Jupiter DC, Mithani M, La Fontaine J, Davis KE, Lavery LA (2017) Erythrocyte sedimentation rate and C-reactive protein to monitor treatment outcomes in diabetic foot osteomyelitis. Int Wound J 14:142–148. https://doi.org/10.1111/iwj.12574
Fleischer AE, Wrobel JS, Leonards A et al (2011) Post-treatment leukocytosis predicts an unfavorable clinical response in patients with moderate to severe diabetic foot infections. J Foot Ankle Surg 50(5):541–546
Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA (2020) Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res 13:16. https://doi.org/10.1186/s13047-020-00383-2
Jacobs E, Rathmann W (2019) Epidemiologie des Diabetes in Deutschland. Deutscher Gesundheitsbericht Diabetes 2019:9–20
Wukich DK, Raspovic KM, Suder NC (2018) Patients with diabetic foot disease fear major lower-extremity amputation more than death. Foot Ankle Spec 11(1):17–21
Heravi FS, Zakrzewski M, Vickery K, Armstrong DG, Hu H (2019) Bacterial diversity of diabetic foot ulcers: current status and future prospectives. J Clin Med 8:1935. https://doi.org/10.3390/jcm8111935
Ziegler D, Landgraf R, Lobmann R et al (2020) Polyneuropathy is inadequately treated despite increasing symptom intensity in individuals with and without diabetes (PROTECT follow-up study). J Diabetes Investig. https://doi.org/10.1111/jdi.13267
Commons RJ, Raby E, Athan E et al (2018) Managing diabetic foot infections: a survey of Australasian infectious diseases clinicians. J Foot Ankle Res 11:13
Lipsky BA (2007) Diabetic foot infection: microbiology made modern? Array Hope Diabetes Care 30:2171–2172
Tascini C, Piaggesi A, Tagliaferri E et al (2011) Microbiology at first visit of moderate-to-severe diabetic foot infection with antimicrobial activity and a survey of quinolone monotherapy. Diabetes Res Clin Pract. 94:133–139
Sotto A, Richard JL, Combescure C et al (2010) Beneficial effects of implementing guidelines on microbiology and costs of infected diabetic foot ulcers. Diabetologia 53:2249–2255
Yao Y, Sturdevant DE, Villaruz A, Xu L, Gao Q, Otto M (2005) Factors characterizing Staphylococcus epidermidis invasiveness determined by comparative genomics. Infect Immun 73:1856–1860
Citron DM, Goldstein EJ, Merriam CV, Lipsky BA, Abramson MA (2007) Bacteriology of moderate-to-severe diabetic foot infections and in vitro activity of antimicrobial agents. J Clin Microbiol 45:2819–2828
Seth A, Attri AK, Kataria H, Kochhar S, Seth SA, Gautam N (2019) Clinical profile and outcome in patients of diabetic foot infection. Int J Appl Basic Med Res 9(1):14–19
Lipsky BA, Aragon-Sachez J, Diggle M (2016) IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes. Diabetes Metab Res Rev 32(Suppl 1):4574
Aghdassi SJ, Schwab F, Hoffmann P, Gastmeier P (2019) The association of climatic factors with rates of surgical site infections—17 year's data from hospital infection surveillance. Dtsch Arztebl Int 116:529–536. https://doi.org/10.3238/aerztebl.2019.0529
Dörr S, Lobmann R (2020) Diabetisches Fußsyndrom, cme-zertifizierte Fortbildung. Der Diabetologe. Springer, Verlag. https://doi.org/10.1007/s11428-020-00597-9
Dzieciuchowicz L, Kruszyna L, Krasinski Z, Espinosa G (2012) Monitoring of systemic inflammatory response in diabetic patients with deep foot infection treated with negative pressure wound therapy. Foot Ankle Int 33(10):832–837
Kröger K, Berg C, Santosa F, Malyar N, Reinecke H (2017) Amputationen der unteren Extremität in Deutschland. Dtsch Aerztebl Int 114:130–136
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Author contributions
SD and RL were involved in conceptualization and methodology; SD helped in validation; SD and FF contributed to formal analysis and data curation; SD, MS and FF were involved in investigation; SD and MS helped in resources; FF contributed to writing—original draft preparation; SD, FF and RL were involved in writing—review and editing; SD contributed to visualization; MS helped in supervision; and RL was involved in project administration.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the ethics committee of the Medical University of Tübingen (application number: 636/2020BO).
Informed consent
Informed consent was obtained from the individual participant included in the study.
Additional information
Managed by Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dörr, S., Freier, F., Schlecht, M. et al. Bacterial diversity and inflammatory response at first-time visit in younger and older individuals with diabetic foot infection (DFI). Acta Diabetol 58, 181–189 (2021). https://doi.org/10.1007/s00592-020-01587-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-020-01587-5