Abstract
Aims
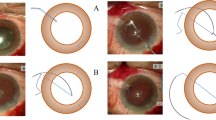
Intraoperative complications in cataract surgery are more common in diabetic patients. Solving aphakia in these circumstances remains a challenge, as the scleral structure has been shown to be different in diabetes. This study aims to analyze the role of a secondary sutureless scleral intraocular lens (IOL) flanged fixation in diabetic patients without capsular support and to compare the anatomical and functional outcomes using a 30 gauge (G) ultrathin wall needle vs. a 27G needle.
Methods
Retrospective, observational cohort study.
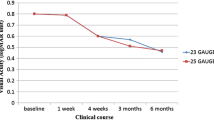
105 eyes (105 patients) who underwent PPV with secondary IOL fixation using a sutureless 27G (n = 51) or a 30G ultrathin wall (UTW) needle technique (n = 54) and had a 24 months postoperative follow up. Consecutive patients’ records were reviewed for lens stability and centration parameters, intra- and postoperative complications at 7 days, 1, 3, 6, 12, and 24 months after surgery. Correlations between outcome measures and needle size (27G vs. 30G UTW) were analyzed.
Results
IOL displacement occurred in 30 patients (41.2%) in the 27G group and did not occur in the 30G UTW needle group (p < 0.001). Mean time until IOL displacement was 10.5 ± 7.0 months (range: 7 days–24 months). IOL centricity was significantly better in the 30G ultrathin wall needle group compared to 27 G (p = 0.001). Additional surgical interventions were necessary only in the 27G group (n = 14).
Conclusions
Sutureless IOL flanged technique using a 30G UTW needle is more predictable and has less complications in aphakic diabetic patients, compared to a 27G needle technique.


Similar content being viewed by others
References
Gelman RA, Garg S (2019) Novel yamane technique modification for haptic exposure after glued intrascleral haptic fixation. Am J Ophthalmol Case Rep 14:101–104. https://doi.org/10.1016/j.ajoc.2019.03.009
Yamane S, Inoue M, Arakawa A, Kadonosono K (2014) Sutureless 27-gauge needle-guided intrascleral intraocular lens implantation with lamellar scleral dissection. Ophthalmology 121:61–66. https://doi.org/10.1016/j.ophtha.2013.08.043
Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K (2017) Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology 124:1136–1142. https://doi.org/10.1016/j.ophtha.2017.03.036
Drolsum L (2003) Long-term follow-up of secondary flexible, open-loop, anterior chamber intraocular lenses. J Cataract Refract Surg 29:498–503. https://doi.org/10.1016/s0886-3350(02)01614-0
Evereklioglu C, Er H, Bekir NA et al (2003) Comparison of secondary implantation of flexible open-loop anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg 29:301–308. https://doi.org/10.1016/s0886-3350(02)01526-2
Baykara M, Ozcetin H, Yilmaz S, Timuçin OB (2007) Posterior iris fixation of the iris-claw intraocular lens implantation through a scleral tunnel incision. Am J Ophthalmol 144:586–591. https://doi.org/10.1016/j.ajo.2007.06.009
Vote BJ, Tranos P, Bunce C et al (2006) Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol 141:308–312. https://doi.org/10.1016/j.ajo.2005.09.012
Matsui Y, Matsubara H, Hanemoto T, Kondo M (2015) Exposure of haptic of posterior chamber intraocular lens after sutureless intrascleral fixation. BMC Ophthalmol 15:104. https://doi.org/10.1186/s12886-015-0102-3
Scharioth GB, Prasad S, Georgalas I et al (2010) Intermediate results of sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg 36:254–259. https://doi.org/10.1016/j.jcrs.2009.09.024
Khan MA, Gupta OP, Smith RG et al (2016) Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. Br J Ophthalmol 100:638–643. https://doi.org/10.1136/bjophthalmol-2015-306839
Das S, Nicholson M, Deshpande K et al (2016) Scleral fixation of a foldable intraocular lens with polytetrafluoroethylene sutures through a Hoffman pocket. J Cataract Refract Surg 42:955–960. https://doi.org/10.1016/j.jcrs.2016.06.018
Coudrillier B, Pijanka J, Jefferys J et al (2015) Effects of age and diabetes on scleral stiffness. J Biomech Eng 137:710071–7100710. https://doi.org/10.1115/1.4029986
Watson PG, Young RD (2004) Scleral structure, organisation and disease. A review. Exp Eye Res 78:609–623. https://doi.org/10.1016/s0014-4835(03)00212-4
Keeley FW, Morin JD, Vesely S (1984) Characterization of collagen from normal human sclera. Exp Eye Res 39:533–542. https://doi.org/10.1016/0014-4835(84)90053-8
Vieira-Potter VJ, Karamichos D, Lee DJ (2016) Ocular complications of diabetes and therapeutic approaches. Biomed Res Int 2016:3801570. https://doi.org/10.1155/2016/3801570
Nguyen BA, Roberts CJ, Reilly MA (2019) Biomechanical impact of the sclera on corneal deformation response to an air-puff: a finite-element study. Front Bioeng Biotechnol 6:210. https://doi.org/10.3389/fbioe.2018.00210
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical standard
Institutional review board (IRB) approval was obtained for a retrospective consecutive chart review. The research adhered to the tenets of the Declaration of Helsinki. All data discussed in this study were fully anonymized before they were accessed.
Informed consent
There was no need for informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Eye Complications of Diabetes, managed by Giuseppe Querques.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 108947 kb)
Rights and permissions
About this article
Cite this article
Iglicki, M., Zur, D., Negri, H.P. et al. Results in comparison between 30 gauge ultrathin wall and 27 gauge needle in sutureless intraocular lens flanged technique in diabetic patients: 24-month follow-up study. Acta Diabetol 57, 1151–1157 (2020). https://doi.org/10.1007/s00592-020-01530-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-020-01530-8