Abstract
Purpose
Rotator cuff repair (RCR) is commonly performed and can have good functional outcomes. However, failure of RCR surgery can be challenging for both patient and surgeon alike. This study examines the outcomes of early revision RCR for the management of clinically failed RCRs.
Methods
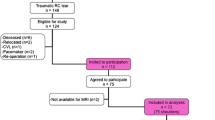
Thirty-six patients undergoing revision RCR within 1 year of primary surgery were evaluated. Range of motion (ROM) and patient-reported outcomes (PROMs) were assessed at baseline, post-primary RCR, and post-revision RCR.
Results
Patients with a documented repair failure after primary RCR failed to improve in both ROM and PROMs compared to before primary RCR. Following early revision, RCR SANE (p = 0.024, p < 0.001), ASES (p = 0.004, p < 0.001), and SST (p < 0.001, p = 0.001) scores improved significantly compared to pre-primary and pre-revision scores, respectively. Documentation of a new traumatic injury did not affect clinical or functional outcomes compared to atraumatic re-tears. Number of tendons torn was positively correlated with higher SANE scores (r = 0.638, p = 0.008) and negatively correlated with SST score (r = −0.475, p = 0.03) and improvement in forward elevation (r = −0.368, p = 0.03) after primary RCR. There were significant correlations between number of tendons torn and improvement in SANE (r = 0.664, p = 0.007) and ASES scores (r = 0.468, p = 0.043) from post-primary RCR to post-revision RCR.
Conclusion
Early revision after failed RCR can lead to clinically significant improvement in functional outcomes. The presence of a traumatic re-injury does not appear to affect revision RCR outcomes as it does in the primary setting. Patients with early clinical failures of primary RCR may benefit from early revision RCR.
Level of evidence: III
Retrospective Case Series.
Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Aleem AW, Brophy RH (2012) Outcomes of rotator cuff surgery. Clin Sports Med 31:665–674. https://doi.org/10.1016/j.csm.2012.07.004
Keener JD, Wei AS, Kim HM et al (2010) Revision arthroscopic rotator cuff repair: repair integrity and clinical outcome. J Bone Joint Surg Am 92:590–598. https://doi.org/10.2106/JBJS.I.00267
Rashid MS, Cooper C, Cook J et al (2017) Increasing age and tear size reduce rotator cuff repair healing rate at 1 year. Acta Orthop, pp 1–6. https://doi.org/10.1080/17453674.2017.1370844
Le BTN, Wu XL, Lam PH, Murrell GAC (2014) Factors Predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med 42:1134–1142. https://doi.org/10.1177/0363546514525336
Iannotti JP, Deutsch A, Green A et al (2013) Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am 95:965–971. https://doi.org/10.2106/JBJS.L.00708
Petersen SA, Murphy TP (2011) The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg 20:62–68. https://doi.org/10.1016/j.jse.2010.04.045
Keener JD, Hsu JE, Steger-May K et al (2015) Patterns of tear progression for asymptomatic degenerative rotator cuff tears. J Shoulder Elbow Surg 24:1845–1851. https://doi.org/10.1016/j.jse.2015.08.038
Cvetanovich GL, Gowd AK, Liu JN et al (2019) Establishing clinically significant outcome after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 28:939–948. https://doi.org/10.1016/j.jse.2018.10.013
Hein J, Reilly JM, Chae J et al (2015) Retear rates after arthroscopic single-row, double-row, and suture bridge rotator cuff repair at a minimum of 1 year of imaging follow-up: a systematic review. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 31:2274–2281. https://doi.org/10.1016/j.arthro.2015.06.004
Tan M, Lam PH, Le BTN, Murrell GAC (2016) Trauma versus no trauma: an analysis of the effect of tear mechanism on tendon healing in 1300 consecutive patients after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 25:12–21. https://doi.org/10.1016/j.jse.2015.06.023
Lädermann A, Denard PJ, Burkhart SS (2016) Management of failed rotator cuff repair: a systematic review. J Isakos 1:32–37. https://doi.org/10.1136/jisakos-2015-000027
Abechain JJK, Godinho GG, Matsunaga FT et al (2017) Functional outcomes of traumatic and non-traumatic rotator cuff tears after arthroscopic repair. World J Orthop 8:631–637. https://doi.org/10.5312/wjo.v8.i8.631
Burkhart SS, Danaceau SM, Pearce CE (2001) Arthroscopic rotator cuff repair: analysis of results by tear size and by repair technique—margin convergence versus direct tendon-to-bone repair. Arthrosc J Arthrosc Relat Surg 17:905–912. https://doi.org/10.1053/jars.2001.26821
Nho SJ, Shindle MK, Adler RS et al (2009) Prospective analysis of arthroscopic rotator cuff repair: Subgroup analysis. J Shoulder Elbow Surg 18:697–704. https://doi.org/10.1016/j.jse.2008.11.018
Valencia Mora M, Morcillo Barrenechea D, Martín Ríos MD et al (2017) Clinical outcome and prognostic factors of revision arthroscopic rotator cuff tear repair. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 25:2157–2163. https://doi.org/10.1007/s00167-016-4392-7
Kowalsky MS, Keener JD (2011) Revision arthroscopic rotator cuff repair: repair integrity and clinical outcome: surgical technique. J Bone Joint Surg Am 93(Suppl 1):62–74. https://doi.org/10.2106/JBJS.J.01173
Lo IKY, Burkhart SS (2004) Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 20:250–267. https://doi.org/10.1016/j.arthro.2004.01.006
Hartzler RU, Sperling JW, Schleck CD, Cofield RH (2013) Clinical and radiographic factors influencing the results of revision rotator cuff repair. Int J Shoulder Surg 7:41–45. https://doi.org/10.4103/0973-6042.114221
Lädermann A, Denard PJ, Burkhart SS (2011) Midterm outcome of arthroscopic revision repair of massive and nonmassive rotator cuff tears. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 27:1620–1627. https://doi.org/10.1016/j.arthro.2011.08.290
Boorman RS, More KD, Hollinshead RM et al (2018) What happens to patients when we do not repair their cuff tears? Five-year rotator cuff quality-of-life index outcomes following nonoperative treatment of patients with full-thickness rotator cuff tears. J Shoulder Elbow Surg 27:444–448. https://doi.org/10.1016/j.jse.2017.10.009
Petri M, Ettinger M, Brand S et al (2016) Non-operative management of rotator cuff tears. Open Orthop J 10:349–356. https://doi.org/10.2174/1874325001610010349
Kukkonen J, Joukainen A, Lehtinen J et al (2015) Treatment of nontraumatic rotator cuff tears: a randomized controlled trial with two years of clinical and imaging follow-up. J Bone Joint Surg Am 97:1729–1737. https://doi.org/10.2106/JBJS.N.01051
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Schoch: Exactech: paid consultant, royalties; Horneff: Miami Device Solutions: Paid consultant, Springer Nature: Publishing royalties, financial or material support, Tigon: Unpaid consultant; Abboud: Aevumed: Stock or stock Options, Arthrex, Inc: Research support, Bioventus: Paid consultant, Department of Defense: Research support, DJ Orthopaedics: IP royalties; Paid consultant, Globus Medical: IP royalties; Paid consultant, Integra: Research support, Lima: Research support, Marlin Medical Alliance, LLC: Stock or stock Options, Mid Atlantic Shoulder and Elbow Society, Executive Board and Founder: Board or committee member, OBERD: Stock or stock Options, OREF: Research support, Orthofix, Inc.: Research support, Orthospace: Research support, OsteoCentric Technologies: IP royalties, OTS Medical: Stock or stock Options, Shoulder JAM LLC: Stock or stock Options, SLACK Incorporated: Publishing royalties, financial or material support, Smith & Nephew: IP royalties, Stryker: IP royalties; Paid consultant, Wolters Kluwer Health - Lippincott Williams & Wilkins: Publishing royalties, financial or material support, Zimmer: IP royalties; Paid consultant; Research support.
IRB Approval #
12D.223.
IRB
Thomas Jefferson University, Office of Human Research, Institutional Review Board, Jefferson Alumni Hall, 1020 Locust St. Suite M-34, Philadelphia PA 19107.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Monir, J.G., Astolfi, M.M., Sholder, D. et al. Early revision rotator cuff repair: an analysis of outcomes and function. Eur J Orthop Surg Traumatol 33, 321–326 (2023). https://doi.org/10.1007/s00590-021-03182-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03182-y