Abstract
Purpose
The aim of this study was to evaluate the associated factors of patients with LSS who undergo reoperation after a PLSF in a Hispanic-American population.
Methods
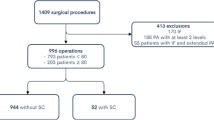
A retrospective single-center review was performed from all non-age-related Hispanic-Americans with LSS who underwent one or two-level PLSF from 2008 to 2018. Baseline characteristics were analyzed between the reoperation and no-reoperation group using a bivariate and multivariate analyses.
Results
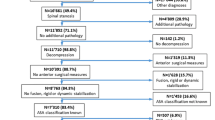
Out of 425 patients who underwent PLSF, 38 patients underwent reoperation. At a two-year follow-up, the reoperation rate was 6.1% (26/425), mostly due to pseudoarthrosis (39.5%), recurrent stenosis (26.3%), new condition (15.8%), infection (10.5%), hematoma (5.3%), and dural tear (2.6%). Patients who underwent reoperation were more likely to have a preoperative history of epidural steroid injection (ESI) (OR 5.18, P = 0.009), four or more comorbidities (OR 2.69, P = 0.028), and operated only with a posterolateral fusion without intervertebral fusion (OR 2.15, P = 0.032). Finally, the multivariable analysis showed that ESI was the only independent associated factor in patients who underwent reoperation after a PLSF in our group.
Conclusion
Among this population who underwent surgery, a reoperation rate at two years of follow-up was less than ten percent. Our study did not find any associated factor inherent to Hispanic-Americans, as ethnic group, who were reoperated after LSS.
Similar content being viewed by others
References
Genevay S, Atlas SJ (2010) Lumbar spinal stenosis. Best Pract Res Clin Rheumatol 24(2):253–265. https://doi.org/10.1016/j.berh.2009.11.001. (PMID:20227646;PMCID:PMC2841052)
Negrini S, Zaina F, Romano M et al (2010) Rehabilitation of lumbar spine disorders: an evidence-based clinical practice approach. In: DeLisa’s physical & rehabilitation principles and practice, 5th ed. Lippincott Williams and Wilkins, Baltimore, pp 837–882
Zaina F, Tomkins-Lane C, Carragee E, Negrini S (2016) Surgical versus nonsurgical treatment for lumbar spinal stenosis. Spine (Phila Pa 1976) 41(14):E857–E868. https://doi.org/10.1097/BRS.0000000000001635. PMID: 27128388
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H (2008) SPORT investigators. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 358(8):794–810. https://doi.org/10.1056/NEJMoa0707136. PMID: 18287602
Lad SP, Bagley JH, Kenney KT, Ugiliweneza B, Kong M, Bagley CA, Gottfried ON, Isaacs RE, Patil CG, Boakye M (2013) Racial disparities in outcomes of spinal surgery for lumbar stenosis. Spine (Phila Pa 1976) 38(11):927–935. https://doi.org/10.1097/BRS.0b013e31828165f9. PMID: 23232216
Weinstein JN, Tosteson TD, Lurie JD, Tosteson A, Blood E, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H (2010) Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine (Phila Pa 1976) 35(14):1329–1338. https://doi.org/10.1097/BRS.0b013e3181e0f04d. PMID: 20453723; PMCID: PMC3392200
Burgstaller JM, Porchet F, Steurer J, Wertli MM (2015) Arguments for the choice of surgical treatments in patients with lumbar spinal stenosis—a systematic appraisal of randomized controlled trials. BMC Musculoskelet Disord 16:96. https://doi.org/10.1186/s12891-015-0548-8 (PMID:25896506;PMCID:PMC4409719)
Gerling MC, Leven D, Passias PG et al (2016) Risk factors for reoperation in patients treated surgically for lumbar stenosis: a subanalysis of the 8-year data from the SPORT trial. Spine (Phila Pa 1976) 41(10):901–909. https://doi.org/10.1097/BRS.0000000000001361
Aizawa T, Ozawa H, Kusakabe T, Tanaka Y, Sekiguchi A, Hashimoto K, Kanno H, Morozumi N, Ishii Y, Sato T, Takahashi E, Kokubun S, Itoi E (2015) Reoperation rates after fenestration for lumbar spinal canal stenosis: a 20-year period survival function method analysis. Eur Spine J 24(2):381–387. https://doi.org/10.1007/s00586-014-3479-4 (Epub 2014 Jul 30 PMID: 25073940)
Ye YP, Xu H, Chen D (2013) Comparison between posterior lumbar interbody fusion and posterolateral fusion with transpedicular screw fixation for isthmic spondylolithesis: a meta-analysis. Arch Orthop Trauma Surg 133(12):1649–1655. https://doi.org/10.1007/s00402-013-1868-5 (Epub 2013 Oct 18 PMID: 24136445)
Kim KT, Lee SH, Lee YH, Bae SC, Suk KS (2006) Clinical outcomes of 3 fusion methods through the posterior approach in the lumbar spine. Spine (Phila Pa 1976) 31(12):1351–1357. discussion 1358. https://doi.org/10.1097/01.brs.0000218635.14571.55. PMID: 16721298
McAfee PC (1999) Interbody fusion cages in reconstructive operations on the spine. J Bone Joint Surg Am 81(6):859–880. https://doi.org/10.2106/00004623-199906000-00014 (PMID: 10391552)
Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG (1997) Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine (Phila Pa 1976) 22(2):210–219. Discussion 219–20. https://doi.org/10.1097/00007632-199701150-00016. PMID: 9122804
Radcliff K, Curry P, Hilibrand A et al (2013) Risk for adjacent segment and same segment reoperation after surgery for lumbar stenosis: a subgroup analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 38(7):531–539. https://doi.org/10.1097/BRS.0b013e31827c99f0
Goel SA, Modi HN (2018) Reoperations following lumbar spinal canal stenosis. Indian J Orthop 52(6):578–583. https://doi.org/10.4103/ortho.IJOrtho_380_17 (PMID: 30532296)
Mok JM, Cloyd JM, Bradford DS, Hu SS, Deviren V, Smith JA, Tay B, Berven SH (2009) Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine (Phila Pa 1976) 34(8):832–839. https://doi.org/10.1097/BRS.0b013e31819f2080. PMID: 19365253
Freedman MK, Hilibrand AS, Blood EA, Zhao W, Albert TJ, Vaccaro AR, Oleson CV, Morgan TS, Weinstein JN (2011) The impact of diabetes on the outcomes of surgical and nonsurgical treatment of patients in the spine patient outcomes research trial. Spine (Phila Pa 1976) 36(4):290–307. https://doi.org/10.1097/BRS.0b013e3181ef9d8c. PMID: 21270715; PMCID: PMC4005359
Seicean A, Seicean S, Neuhauser D, Benzel EC, Weil RJ (2017) The influence of race on short-term outcomes after laminectomy and/or fusion spine surgery. Spine (Phila Pa 1976) 42(1):34–41. https://doi.org/10.1097/BRS.0000000000001657. PMID: 27128387
Eguia E, Cobb AN, Kirshenbaum EJ, Afshar M, Kuo PC (2018) Racial and ethnic postoperative outcomes after surgery: the hispanic paradox. J Surg Res 232:88–93. https://doi.org/10.1016/j.jss.2018.05.074 (Epub 2018 Jul 3 PMID: 30463790)
Bonaccorsi HA, Burns B (2020) Perioperative cardiac management. [Updated 2020 Nov 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK493196/
Le Huec JC, Seresti S, Bourret S, Cloche T, Monteiro J, Cirullo A, Roussouly P (2020) Revision after spinal stenosis surgery. Eur Spine J 29(Suppl 1):22–38. https://doi.org/10.1007/s00586-020-06314-w (Epub 2020 Jan 29 PMID: 31997016)
Skolasky RL, Maggard AM, Thorpe RJ Jr, Wegener ST, Riley LH 3rd (2013) United States hospital admissions for lumbar spinal stenosis: racial and ethnic differences, 2000 through 2009. Spine (Phila Pa 1976) 38(26):2272–2278. https://doi.org/10.1097/BRS.0b013e3182a3d392. PMID: 23873234
Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA (2007) Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine (Phila Pa 1976) 32(3):382–387. https://doi.org/10.1097/01.brs.0000254104.55716.46. PMID: 17268274
Cheng J, Wang H, Zheng W, Li C, Wang J, Zhang Z, Huang B, Zhou Y (2013) Reoperation after lumbar disc surgery in two hundred and seven patients. Int Orthop 37(8):1511–1517. https://doi.org/10.1007/s00264-013-1925-2. Epub 2013 May 22. PMID: 23695881; PMCID: PMC3728382
Kreitz TM, Mangan J, Schroeder GD, Kepler CK, Kurd MF, Radcliff KE, Woods BI, Rihn JA, Anderson DG, Vaccaro AR, Hilibrand AS (2021) Do preoperative epidural steroid injections increase the risk of infection after lumbar spine surgery? Spine (Phila Pa 1976) 46(3):E197–E202. https://doi.org/10.1097/BRS.0000000000003759. PMID: 33079913
Sears WR, Sergides IG, Kazemi N, Smith M, White GJ, Osburg B (2011) Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J 11(1):11–20. https://doi.org/10.1016/j.spinee.2010.09.026 (PMID: 21168094)
Rihn JA, Radcliff K, Hilibrand AS, Anderson DT, Zhao W, Lurie J, Vaccaro AR, Freedman MK, Albert TJ, Weinstein JN (2012) Does obesity affect outcomes of treatment for lumbar stenosis and degenerative spondylolisthesis? Analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 37(23):1933–1946. https://doi.org/10.1097/BRS.0b013e31825e21b2. PMID: 22614793
Bydon M, De la Garza-Ramos R, Abt NB, Gokaslan ZL, Wolinsky JP, Sciubba DM, Bydon A, Witham TF (2014) Impact of smoking on complication and pseudarthrosis rates after single- and 2-level posterolateral fusion of the lumbar spine. Spine (Phila Pa 1976) 39(21):1765–70. https://doi.org/10.1097/BRS.0000000000000527. PMID: 25054650
Kim CH, Chung CK, Shin S, Choi BR, Kim MJ, Park BJ, Choi Y (2015) The relationship between diabetes and the reoperation rate after lumbar spinal surgery: a nationwide cohort study. Spine J 15(5):866–874. https://doi.org/10.1016/j.spinee.2015.01.029 (Epub 2015 Jan 29 PMID: 25638495)
Gerling MC, Leven D, Passias PG, Lafage V, Bianco K, Lee A, Morgan TS, Lurie JD, Tosteson TD, Zhao W, Spratt KF, Radcliff K, Errico TJ (2017) Risk Factors for Reoperation in Patients Treated Surgically for Degenerative Spondylolisthesis: A Subanalysis of the 8-year Data From the SPORT Trial. Spine (Phila Pa 1976) 42(20):1559–1569. https://doi.org/10.1097/BRS.0000000000002196. PMID: 28399551
Funding
No funds were received in support of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
José C. Pérez-López, MD; Gerardo Olivella, MD, MPH; Miguel Cartagena, BS; José Acosta-Julbe, BS; Christian Nieves-Ríos, BS; Norman Ramírez, MD; José Massanet-Volrath, MD; José Montañez-Huertas, MD; Enrique Escobar, MD declare that they have no conflict of interest.
Device status/drug statement
The manuscript submitted does not contain information about medical device(s)/drug(s).
Ethics approval
Protocol # B3340120 by the University of Puerto Rico Medical Sciences Campus Institutional Review Board (IRB #: B3340120).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pérez-López, J.C., Olivella, G., Cartagena, M. et al. Associated factors of patients with spinal stenosis who undergo reoperation after a posterior lumbar spinal fusion in a Hispanic-American population. Eur J Orthop Surg Traumatol 32, 1491–1499 (2022). https://doi.org/10.1007/s00590-021-03127-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03127-5