Abstract
Introduction
The novel coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organisation on 11 March 2020. The aim of this study is to assess the impact of COVID-19 on orthopaedic practice and training in the UK.
Methods
Surgeons throughout UK hospitals were asked to complete an electronic survey relating to orthopaedic practice and training in their hospital. The nationwide survey was conducted during the first peak of COVID-19 cases in the UK between 20 March 2020 and 20 April 2020.
Results
All 202 UK participants reported disruption to their daily practice. 91% reported all elective operating had been cancelled and trauma continued as normal in only 24% of cases. 70% reported disruption to trauma operating. Elective clinic capacity significantly reduced with no elective clinics running as normal. 55% reported their elective clinics completely cancelled, whilst 38% reported elective clinics running at a reduced capacity, with non-urgent appointments postponed. Only 9% of fracture clinics ran as normal, and 69% had a reduced service. 67% reported teaching and study leave cancelled. Significantly, 69% of participants felt the pandemic would result in a delay to completion of registrar training programmes.
Conclusion
This is the first nationwide survey assessing the impact of the coronavirus disease 2019 on UK orthopaedic practice and training, during the peak of the pandemic. It highlights the scale of the challenge ahead for the specialty, including during the recovery phase and post-recovery phase of the pandemic.
Similar content being viewed by others
Introduction
The novel coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organisation on 11 March 2020 [1]. There were over three million reported cases in 187 countries by the start of May 2020 [2]. The UK recorded its first confirmed case of acute respiratory infection due to COVID-19 on 31 January 2020 [3]. The initial response was to “track-and-trace”, quarantining at-risk individuals to contain the spread of infection [4]. This was surpassed by the “delay” phase of the response on 12 March 2020 [5]. The two main strategies of this response have been to reduce the rate of transmission by social distancing measures and to increase the National Health Service (NHS) inpatient capacity, with particular emphasis on increasing ventilated bed capacity [5]. Both these strategies have had a significant impact on orthopaedic services, especially elective work in the UK.
As part of this response, NHS Hospitals in England were told to suspend all non-urgent elective surgery for at least three months from 15 April, to increase bed capacity and to free up theatre ventilators to be used for acutely unwell COVID-19 patients [6]. The British Orthopaedic Association subsequently published guidelines advising surgeons to reduce inpatient stays and face to face consultations wherever possible. The guidelines also acknowledged that non-operative options for treatment should be utilised wherever possible [7].
The aim of this study is to assess the impact these measures had on orthopaedic practice in the UK. These include repercussions around patient care and the short- and long-term sequelae on orthopaedic training at all levels in the UK.
Methods
Surgeons throughout UK hospitals were asked to complete a short electronic survey focused on orthopaedics practice in their hospital. Specifically, the questionnaire was sent to all Training Programme Directors in the country, and these were then disseminated to consultants and juniors in each of the deaneries. In addition, the British Orthopaedic Trainee Association and Orthopaedic Trauma Society were used to disseminate the survey. This targeted each geographic region in the country and a combination of trainee and trainer replied. Questions included the effect of COVID-19 on orthopaedic trauma and elective operations, orthopaedic outpatient clinics, the effect on formal teaching and key training requirements and also the long-term effects on orthopaedic training (Online Appendix 1). The survey was conducted during the first peak of COVID-19 cases in the UK, between 20 March 2020 and 20 April 2020. This was during the UK government’s “delay” phase of the response.
Results
The nationwide survey received 202 responses. 60% were consultant orthopaedic surgeons, 35% were orthopaedic specialist registrars, and the remainder were more junior members of hospital orthopaedic teams. These included core trainees, foundation year doctors and specialist nurse practitioners. The surgeons worked in a range of healthcare facilities: 41% in a trauma centre; 53% in a district general hospital with 24 h trauma facilities; 4% in a district general hospital with trauma facilities that were not 24 h; 3% in a paediatric trauma unit; and 2% in an elective only unit.
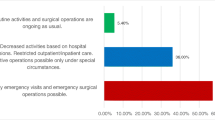
All 202 UK participants reported some disruption to their daily practice. 91% reported all elective operating cancelled, and 6% reported some elective operating was continuing but at a reduced rate. Trauma services were also affected with only 24% reporting trauma lists continuing as normal and 70% reporting reduced trauma capacity (Fig. 1). Participants reported strategies to overcome this included moving trauma cases to elective hospitals, private hospitals or transferring between hospitals within the same trauma network.
The disruption to trauma operations appears to have affected major trauma centres (MTC) and district general hospitals (DGH) proportionally at this stage of the crisis. However, those that worked at a MTC reported their hospitals were more likely to be continuing some elective operating at a reduced rate (Fig. 2).
Elective outpatient clinic capacity was significantly reduced with no elective clinics running as normal. 55% reported their elective clinics were completely cancelled, whilst 38% reported elective clinics were running at a reduced capacity, with non-urgent appointments postponed. Many reported running a telephone or virtual elective clinic service.
Fracture clinics were less severely affected with 9% running as normal and 69% with a reduced service (Fig. 3). Again, participants reported adopting telephone or virtual clinics where possible. Many units also set up trauma clinics in the emergency department. The theory behind this is to reduce the need for follow-up clinic appointments if definitive treatment can be given at the initial hospital visit.
COVID-19 was also reported to have a significant impact on non-clinical training opportunities, including 67% reporting all teaching and study leave being cancelled and 33% reporting teaching had been reduced or the method of delivery changed. 35% of registrars reported having essential training opportunities such as examinations and key courses cancelled. Significantly, 69% of registrars felt the pandemic would result in a delay of their certificate of completion date.
Discussion
This survey provides an initial insight into the level of disruption that the COVID-19 pandemic and associated UK government response strategies are having on orthopaedic services in the UK. It highlights the scale of the challenge ahead, including during the following recovery phase and post-recovery phase.
Elective surgery has been cancelled for three months at least. In addition, as social distancing measures are eased, it is unclear whether a resurgence of COVID-19 cases will be seen and at what stage elective operations will fully resume. However, it is certain we will face a large backlog of elective operations once services resume [8]. It is likely that there will be a phased return as service providers must consider the timing and risks and benefits based on individual units, case type and patient demographics. COVID-19 will continue to circulate in the population for the foreseeable future, and therefore, the risk to patients attending hospitals for elective surgery must be considered. In particular, COVID-19 has a significantly worse prognosis in those older than 65, with underlying co-morbidities including hypertension, diabetes, cardiovascular disease, respiratory disease and obesity [9]. These are important factors to consider when implementing services such as arthroplasty surgery, where many patients will have one or more of these risk factors.
Managing the capacity safely in the presence of ongoing social distancing rules is also going to be a challenge. It may be that virtual and telephone consultations will have to become the new “normal” in outpatient services until an effective treatment or vaccination for COVID-19 can be implemented. Ensuring the operating theatre remains safe for staff, especially where aerosol generation risk is high, will require additional steps in cleaning and utilisation of personal protective equipment [10]. This will increase turnover times between cases and reduce list utilisation. With 70% of participants reporting a reduction of trauma capacity at their hospitals, there will be an inevitable increase in trauma cases as lockdown is lifted. This will put considerable strain on these trauma lists and hospitals must prepare for this surge in trauma with increased trauma theatre capacity.
In the UK, all orthopaedic trainees must fulfil certain criteria before being awarded a Certificate for Completion of Training (CCT). These include passing both parts of the Fellowship of the Royal Colleges of Surgeons (FRCS) examination; attending mandatory courses (Advanced Trauma Life Support), Research Methodologies Course, AO principles course, Training the Trainer and a Management Course); showing competence in performing a range of index operative procedures and showing evidence of being involved with teaching, quality improvement activities, presenting at conferences and management and leadership roles.
With the majority of elective cases cancelled and significantly reduced trauma capacity as reported in the questionnaire, UK orthopaedic trainees are going to see a dramatic reduction in the number of operations they participate in and therefore the breadth of pathologies they are exposed to. In addition, the use of personal protection equipment and delay in turnover time between cases due to theatre cleaning will increase further pressure on training opportunities in theatre. This will no doubt continue during the recovery phase. Loss of elective clinic will result in less exposure to new conditions. Reduced volume of trauma will not only lead to reduction in surgical skills training but also a reduced discussion content in morning meetings. Finally, postponement of FRCS examination dates is likely to affect CCT date and progression onto fellowship and consultant roles for senior trainees.
It remains to be seen how long this situation will continue and therefore whether the pandemic will have any lasting impact on surgical skills. These are points we will address with future studies looking in more detail at the extent and duration of limitations of training in the recovery phase. These will include the potential reduction in indicative numbers achieved, the potential reduction in the total number of operations trainees participate in and the ratio of assisting in operations versus operations performed by the trainee. Orthopaedic departments must consider how they are going to face the challenge of delivering effective training in this new environment. Within the clinic setting, service provision is going to risk disrupting important leaning opportunities in fracture and elective clinics. Training programme directors, academic supervisors and trainees must together consider ways in which these training opportunities can be reinstated and surgical skills maintained and monitored.
The majority (67%) of participants in the survey reported that teaching and study leave has been cancelled in the acute phase of the UK COVID-19 response. Some reported that alternative methods of delivery, such as virtual lectures, have already been initiated for regional and local teaching. It is likely that virtual teaching is going to play a bigger role going forward and training providers should continue to use technology to increase learning resources for surgical trainees across the country. Certainly, this is one area where trainees, with reduced clinic and theatre commitments or opportunities, can improve learning opportunities.
Significantly, 35% of registrars reported, during this small time window, cancellation of key courses such as Advance Trauma Life Support and FRCS examinations. As we progress through the “delay” phase and then the “recovery” phase, this number is likely to increase. These are key requirements for attaining a certificate of completion of training in the UK. Despite evolving discussions involving training directors and the Joint Committee on Surgical Training in the UK aiming to find pragmatic and safe solutions to these difficulties, this has undoubtedly led to significant anxiety for trainees. The majority of registrars in the survey believe the disruption will lead to a delay in their completion of training and subsequent progression of their career.
Conclusion
This is the first nationwide survey assessing the impact of the coronavirus disease 2019 on UK orthopaedic practice and training. It highlights the level of disruption faced by surgeons and the likely challenges the speciality faces going forward. It provides a general overview of the current situation, with collection of real-time information during the peak of the pandemic. To gather further insight, we intend to repeat the survey in three- and six-month time with more detailed follow-up questions to provide a picture of how different parts of the UK have been affected. This will include how quickly services are re-instated over the coming months as we enter the recovery phase and the possible long-term effects on orthopaedic training in the UK.
References
World Health Organisation (2020) Rolling updates on coronavirus disease (COVID-19). Accessed May 2, 2020, from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
Johns Hopkins University (2020) COVID-19 Dashboard by the centre systems science and engineering. Accessed May 2, 2020, from https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
Department of Health and Social Care (2020) CMO confirms cases of coronavirus in England. Accessed 2020, from https://www.gov.uk/government/news/cmo-confirms-cases-of-coronavirus-in-england
Department of Health and Social Care (2020) Health Secretary sets out government 'battle plan' for COVID-19. Accessed May 2, 2020, from https://www.gov.uk/government/news/health-secretary-sets-out-government-battle-plan-for-covid-19
Public Health England (2020) COVID-19: infection prevention and control guidance. Accessed May 2, 2020, from https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-contro
Iacobucci G (2020) Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ 368:m1106
British Orthopaedic Association 2020 BOAST—Management of patients with urgent Orthopaedic conditions and trauma during the coronavirus pandemic. Accessed May 2, 2020, from https://www.boa.ac.uk/resources/covid-19-boasts-combined.html
Swiontkowski M (2020) COVID-19 pandemic and JBJS. J Bone Joint Surg Am 102(9):733. https://doi.org/10.2106/JBJS.20.00471
Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J et al (2020) Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect 81:e16–e25
Raghavan R, Middleton PR, Mehdi A (2020) Minimising aerosol generation during orthopaedic surgical procedures- Current practice to protect theatre staff during Covid-19 pandemic. J Clin Orthop Trauma 1(3):506
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Khan, H., Williamson, M. & Trompeter, A. The impact of the COVID-19 pandemic on orthopaedic services and training in the UK. Eur J Orthop Surg Traumatol 31, 105–109 (2021). https://doi.org/10.1007/s00590-020-02748-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02748-6