Abstract
Introduction
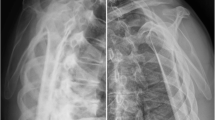
Surgical indication for acromioclavicular joint (ACJ) injuries still represents a reason for shoulder and trauma debate. In high-grade injuries, surgery is advocated because some of the non-operatively managed patients may have persistent shoulder pain that could make them unable to return to their previous activity. It has been shown that many of the patients with high-grade ACJ injuries that are managed non-operatively involve the development of scapular dyskinesis, situation that may result in loss of strength and weakness. On the other side, it has been widely reported that the period while the hook plate is present involves functional limitations and pain. The purpose of this study was to compare the quality of life (QoL) of patients with acute high-grade ACJ injuries (Rockwood grade III–V), managed operatively with a hook plate versus the QoL of patients managed non-operatively, 24 months or more after shoulder injury.
Patients and methods
Patients with acute high-grade ACJ injuries managed operatively (hook plate) or non-operatively, between 2008 and 2012 were included. The QoL was evaluated by means of the Health Survey questionnaire (SF36), the Visual Analogue Scale (VAS) for pain, the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire, the Constant score and the Global Satisfaction (scale from 0 to 10) assessed at the last follow-up visit. The presence of scapular dyskinesis was assessed. Comparison between groups was made.
Results
Thirty-two patients were included: 11 hook plate-group (PLATE group) (5 Rockwood III and 6 V) and 21 conservative-group (CONS group) (4 Rockwood III and 17 V). The mean age was 41 [19–55] years old for the PLATE group and 38 [19–55] for the CONS group (p = 0.513). The mean follow-up was 32.50 ± 11.64 months for the PLATE group and 34.77 ± 21.98 months for the CONS group (p = 0.762). The mean results of the questionnaires assessed at the last follow-up visit were: (1) physical SF36 score (PLATE group 53.70 ± 4.33 and CONS group 52.10 ± 6.11, p = 0.449); (2) mental SF36 score (PLATE group 53.06 ± 6.10 and CONS group 56.99 ± 6.47, p = 0.110); (3) VAS for pain (PLATE group 1.45 ± 1.51 and CONS group 1.50 ± 1.79, p = 0.943); (4) DASH score (PLATE group 4.79 ± 5.60 and CONS group 5.83 ± 6.76, p = 0.668); (5) Constant score (PLATE group 91.36 ± 6.84 and CONS group 91.05 ± 7.35, p = 0.908); (6) Global Satisfaction (PLATE group 8.00 ± 1.18 and CONS group 8.45 ± 1.73, p = 0.449). There was evidence of scapular dyskinesis in 18 % (2/11) of the patients of the PLATE group and in 52.4 % (11/21) of the patients of the CONS group (p = 0.127).
Conclusions
Patients with acute high-grade ACJ injuries managed operatively with a hook plate may have the same QoL and self-reported questionnaires than patients with high-grade ACJ injuries managed non-operatively, 24 months or more after shoulder injury. If surgery is advocated for this type of injury, the orthopedic population must be aware that the hook-plate system might not represent the most suitable option.
Level of evidence
Level IV therapeutic; retrospective comparative study.




Similar content being viewed by others
References
Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG, Edgar CM, Imhoff AB, Arciero RA, Mazzocca AD (2013) Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 29:387–397. doi:10.1016/j.arthro.2012.11.023
Gumina S, Carbone S, Postacchini F (2009) Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy 25:40–45. doi:10.1016/j.arthro.2008.08.019
Rosenorn M, Pedersen EB (1974) A comparison between conservative and operative treatment of acute acromioclavicular dislocation. Acta Orthop Scand 45:50–59
Cardone D, Brown JN, Roberts SN, Saies AD, Hayes MG (2002) Grade III acromioclavicular joint injury in Australian rules football. J Sci Med Sport 5:143–148
Galpin RD, Hawkins RJ, Grainger RW (1985) A comparative analysis of operative versus nonoperative treatment of grade III acromioclavicular separations. Clin Orthop Relat Res 193:150–155
Jacobs B, Wade PA (1966) Acromioclavicular-joint injury. An end-result study. J Bone Joint Surg Am 48:475–486
Calvo E, Lopez-Franco M, Arribas IM (2006) Clinical and radiologic outcomes of surgical and conservative treatment of type III acromioclavicular joint injury. J Shoulder Elbow Surg 15:300–305
MacDonald PB, Alexander MJ, Frejuk J, Johnson GE (1988) Comprehensive functional analysis of shoulders following complete acromioclavicular separation. Am J Sports Med 16:475–480
Taft TN, Wilson FC, Oglesby JW (1987) Dislocation of the acromioclavicular joint. An end-result study. J Bone Joint Surg Am 69:1045–1051
Gstettner C, Tauber M, Hitzl W, Resch H (2008) Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg 17:220–225
Walsh WM, Peterson DA, Shelton G, Neumann RD (1985) Shoulder strength following acromioclavicular injury. Am J Sports Med 13:153–158
Bakalim G, Wilppula E (1975) Surgical or conservative treatment of total dislocation of the acromioclavicular joint. Acta Chir Scand 141:43–47
Larsen E, Hede A (1987) Treatment of acute acromioclavicular dislocation. Three different methods of treatment prospectively studied. Acta Orthop Belg 53:480–484
Press J, Zuckerman JD, Gallagher M, Cuomo F (1997) Treatment of grade III acromioclavicular separations. Operative versus nonoperative management. Bull Hosp Joint Dis 56:77–83
Larsen E, Bjerg-Nielsen A, Christensen P (1986) Conservative or surgical treatment of acromioclavicular dislocation. A prospective, controlled, randomized study. J Bone Joint Surg Am 68:552–555
Bannister GC, Wallace WA, Stableforth PG, Hutson MA (1989) The management of acute acromioclavicular dislocation. A randomised prospective controlled trial. J Bone Joint Surg Br 71:848–850
Natera L, Sarasquete J, Abat F, Besalduch M, Monllau JC, Videla S (2015) Acute unstable acromioclavicular joint injuries: quality of life comparison between patients managed operatively with a coracoclavicular suspension device arthroscopically placed versus patients managed non-operatively. Eur Orthop Traumatol 6(4):343–355. doi:10.1007/s12570-015-0326-y
Johansen JA, Grutter PW, McFarland EG, Petersen SA (2011) Acromioclavicular joint injuries: indications for treatment and treatment options. J Shoulder Elbow Surg 20:70–82. doi:10.1016/j.jse.2010.10.030
Warth RJ, Martetschläger F, Gaskill TR, Millett PJ (2013) Acromioclavicular joint separations. Curr Rev Musculoskelet Med 6:71–78. doi:10.1007/s12178-012-9144-9
Jensen G, Katthagen JC, Alvarado LE, Lill H, Voigt C (2014) Has the arthroscopically assisted reduction of acute AC joint separations with the double tight-rope technique advantages over the clavicular hook plate fixation? Knee Surg Sports Traumatol Arthrosc 22:422–430. doi:10.1007/s00167-012-2270-5
Kienast B, Thietje R, Queitsch C, Gille J, Schulz AP, Meiners J (2011) Mid-term results after operative treatment of Rockwood grade III–V acromioclavicular joint dislocations with an AC-hook-plate. Eur J Med Res 16:52–56
Natera L, Sarasquete J, Escolà A, Rodriguez-Miralles J (2016) Acute high-grade acromioclavicular joint injuries treatment: arthroscopic nonrigid coracoclavicular fixation provides better quality of life outcomes than hook plate ORIF. Orthop Traumatol Surg Res 102(1):31–39. doi:10.1016/j.otsr.2015.10.007
Ding M, Ni J, Hu J, Song D (2011) Rare complication of clavicular hook plate: clavicle fracture at the medial end of the plate. J Shoulder Elbow Surg 20:18–20. doi:10.1016/j.jse.2011.06.005
Hackenberger J, Schmidt J, Altmann T (2004) The effects of hook plates on the subacromial space—a clinical and MRT study. Z Orthop Ihre Grenzgeb 142:603–610
Lin HY, Wong PK, Ho WP, Chuang TY, Liao YS, Wong CC (2014) Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion-dynamic sonographic evaluation. J Orthop Surg Res 6(9):6. doi:10.1186/1749-799X-9-6
Rockwood CA Jr, Williams GR Jr, Young DC (1998) Disorders of the acromioclavicular joint. In: Rockwood CA Jr, Matsen FA 3rd (eds) The shoulder. WB Saunders, Philadelphia, pp 483–553
Beitzel K, Mazzocca AD, Bak K, Itoi E, Kibler WB, Mirzayan R, Imhoff AB, Calvo E, Arce G, Shea K (2014) ISAKOS upper extremity committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy 30:271–278. doi:10.1016/j.arthro.2013.11.005
Kibler WB, McMullen J (2003) Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg 11:142–151
Uhl TL, Kibler WB, Gecewich B, Tripp BL (2009) Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy 25:1240–1248. doi:10.1016/j.arthro.2009.06.007
Jari R, Costic RS, Rodosky MW, Debski RE (2004) Biomechanical function of surgical procedures for acromioclavicular joint dislocations. Arthroscopy 20:237–245
Kim YS, Yoo YS, Jang SW, Nair AV, Jin H, Song HS (2015) In vivo analysis of acromioclavicular joint motion after hook plate fixation using three-dimensional computed tomography. J Shoulder Elbow Surg 24(7):1106–1111. doi:10.1016/j.jse.2014.12.012
Chiang CL, Yang SW, Tsai MY, Kuen-Huang Chen C (2010) Acromion osteolysis and fracture after hook plate fixation for acromioclavicular joint dislocation: a case report. J Shoulder Elbow Surg 19:13–15. doi:10.1016/j.jse.2009.12.005
Hoffler CE, Karas SG (2010) Transacromial erosion of a locked subacromial hook plate: case report and review of literature. J Shoulder Elbow Surg 19:e12–e15. doi:10.1016/j.jse.2009.10.019
Bahk MS, Kuhn JE, Galatz LM, Connor PM, Williams GR Jr (2010) Acromioclavicular and sternoclavicular injuries and clavicular, glenoid, and scapular fractures. Instr Course Lect. J Bone Joint Surg Am 59:209–226
Sim E, Schwarz N, Hocker K, Berzlanovich A (1995) Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Clin Orthop Relat Res 314:134–142. doi:10.1097/00003086-199505000-00017
Nadarajah R, Mahaluxmivala J, Amin A, Goodier DW (2005) Clavicular hook-plate: complications of retaining the implant. Injury 36:681–683. doi:10.1016/j.injury.2004.08.010
McKee M, Pelet S, McCormack RG, Harvey E, Papp S, Rouleau D et al (2015) Multicenter randomized clinical trial of nonoperative versus operative treatment of acute acromio-clavicular joint dislocation. J Orthop Trauma 29(11):479–487. doi:10.1097/BOT.0000000000000437
Murena L, Canton G, Vulcano E, Cherubino P (2013) Scapular dyskinesis and SICK scapula syndrome following surgical treatment of type III acute acromioclavicular dislocations. Knee Surg Sports Traumatol Arthrosc 21:1146–1150
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Luis Natera Cisneros and Dr. Juan Sarasquete declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Natera Cisneros, L.G., Sarasquete Reiriz, J. Acute high-grade acromioclavicular joint injuries: quality of life comparison between patients managed operatively with a hook plate versus patients managed non-operatively. Eur J Orthop Surg Traumatol 27, 341–350 (2017). https://doi.org/10.1007/s00590-016-1862-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1862-z