Abstract
Purpose
Pelvic incidence (PI) is commonly used to determine sagittal alignment. Historically, PI was believed to be a fixed anatomic parameter. However, recent studies have suggested that there is positionally-dependent motion that occurs through the sacroiliac joint (SIJ) resulting in changes in PI.
Methods
We reviewed 100 consecutive adult spinal deformity (ASD) patients seen at our academic tertiary referral center. Two reviewers measured pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), and lumbar lordosis (LL) on standing radiographs and scout computed tomography scans (CT). Unilateral, bilateral, or absent SIJ vacuum sign (VS) was determined using CTs.
Results
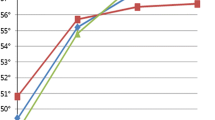
Eighty-six patients (42 M:44 F) were included with an average age of 64.1 years and BMI of 28.8 kg/m2. Standing PI was low (< 50°) in 35 patients (40.7%), average (50°-60°) in 22 (25.6%), and high (> 60°) in 29 (33.7%). Average and high PI patients had significant PI changes of 3.0° (p = 0.037) and 4.6° (p = 0.005), respectively. Bilateral SIJ VS was seen in 68 patients, unilateral VS in 9, and VS was absent in 9. The average change in PI between standing and supine was 2.1° in bilateral SIJ VS patients (p = 0.045), 2.2° in unilateral SIJ VS (p = 0.23), and − 0.1° in patients without SIJ VS (p = 0.93). The average absolute difference in PI between supine and standing was 5.5° ±5.5° (p < 0.001).
Conclusion
There is a change in PI from supine to standing. In patients with high PI and bilateral VS on CT, the change from supine to standing is significant, perhaps representing instability of the SIJ.


Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J Apr 15(4):415–422. https://doi.org/10.1007/s00586-005-0984-5
Schwab F, Lafage V, Patel A, Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 34(17):1828-33. https://doi.org/10.1097/BRS.0b013e3181a13c08
Yamato Y, Hasegawa T, Kobayashi S, Yasuda T, Togawa D, Arima H, Oe S, Iida T, Matsumura A, Hosogane N, Matsumoto M, Matsuyama Y (2016) Calculation of the target lumbar Lordosis Angle for restoring an optimal pelvic tilt in Elderly patients with adult spinal deformity. Spine (Phila Pa 1976). 41(4):E211–E217. https://doi.org/10.1097/BRS.0000000000001209
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F, Pérez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A, European Spine Study Group (ESSG) (2017) Global Alignment and Proportion (GAP) score: development and validation of a New Method of analyzing Spinopelvic Alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am Oct 4(19):1661–1672. https://doi.org/10.2106/JBJS.16.01594
Hyun SJ, Han S, Kim YB, Kim YJ, Kang GB, Cheong JY (2019) Predictive formula of ideal lumbar lordosis and lower lumbar lordosis determined by individual pelvic incidence in asymptomatic elderly population. Eur Spine J Sep 28(9):1906–1913. https://doi.org/10.1007/s00586-019-05955-w
Dial BL, Hills JM, Smith JS, Sardi JP, Lazaro B, Shaffrey CI, Bess S, Schwab FJ, Lafage V, Lafage R, Kelly MP, Bridwell KH (2022) The impact of lumbar alignment targets on mechanical complications after adult lumbar scoliosis surgery. Eur Spine J Jun 31(6):1573–1582. https://doi.org/10.1007/s00586-022-07200-3
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine [published correction appears in Eur Spine J. 2019]. Eur Spine J 28(9):1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Mikula AL, Fogelson JL, Oushy S, Pinter ZW, Peters PA, Abode-Iyamah K, Sebastian AS, Freedman B, Currier BL, Polly DW, Elder BD (2021) Change in pelvic incidence between the supine and standing positions in patients with bilateral sacroiliac joint vacuum signs. J Neurosurg Spine Jan 15(4):617–622. https://doi.org/10.3171/2020.8.SPINE20742
Place HM, Hayes AM, Huebner SB, Hayden AM, Israel H, Brechbuhler JL (2017) Pelvic incidence: a fixed value or can you change it? Spine J Oct 17(10):1565–1569. https://doi.org/10.1016/j.spinee.2017.06.037
Schroeder N, Noschenko A, Burger E, Patel V, Cain C, Ou-Yang D, Kleck C (2018) Pelvic incidence changes between Flexion and Extension. Spine Deform Nov-Dec 6(6):753–761. https://doi.org/10.1016/j.jspd.2018.03.008
Lee JH, Na KH, Kim JH, Jeong HY, Chang DG (2016) Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur Spine J Nov 25(11):3707–3714. https://doi.org/10.1007/s00586-015-4199-0
Ivanov AA, Kiapour A, Ebraheim NA, Goel V (2009) Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine (Phila Pa 1976). 34(5):E162-9. https://doi.org/10.1097/BRS.0b013e3181978ea3
Sturesson B, Udén A, Onsten I (1999) Can an external frame fixation reduce the movements in the sacroiliac joint? A radiostereometric analysis of 10 patients. Acta Orthop Scand 70(1):42–46. https://doi.org/10.3109/17453679909000956
Jacob HA, Kissling RO (1995) The mobility of the sacroiliac joints in healthy volunteers between 20 and 50 years of age. Clin Biomech (Bristol Avon) 10(7):352–361. https://doi.org/10.1016/0268-0033(95)00003-4
Wilke HJ, Fischer K, Jeanneret B, Claes L, Magerl F (1997) In-vivo-Messung der dreidimensionalen Bewegung des Iliosakralgelenks [In vivo measurement of 3-dimensional movement of the iliosacral joint]. Z Orthop Ihre Grenzgeb. 135(6):550-6. German. https://doi.org/10.1055/s-2008-1039744
Smidt GL, Wei SH, McQuade K, Barakatt E, Sun T, Stanford W (1997) Sacroiliac motion for extreme hip positions. A fresh cadaver study. Spine (Phila Pa 1976) 15(18):2073–2082. https://doi.org/10.1097/00007632-199709150-00003
Koo TK, Li MY (2017) A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15(2):155 – 63. https://doi.org/10.1016/j.jcm.2016.02.012. Erratum in: J Chiropr Med. 2017;16(4):346
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16(9):1459–1467. https://doi.org/10.1007/s00586-006-0294-6
Oba H, Ebata S, Takahashi J, Ikegami S, Koyama K, Haro H, Kato H, Ohba T (2019) Loss of Pelvic Incidence Correction After Long Fusion Using Iliac Screws for Adult Spinal Deformity: Cause and Effect on Clinical Outcome. Spine (Phila Pa 1976). 44(3):195–202. https://doi.org/10.1097/BRS.0000000000002775
Jentzsch T, Geiger J, Bouaicha S, Slankamenac K, Nguyen-Kim TD, Werner CM (2013) Increased pelvic incidence may lead to arthritis and sagittal orientation of the facet joints at the lower lumbar spine. BMC Med Imaging Nov 5:13:34. https://doi.org/10.1186/1471-2342-13-34
Gaspoz F, Monnin P, Petter D, Plé J, Ding S (2015) Precision and Accuracy of measurements on CT Scout View. J Med Imaging Radiat Sci 46(3):309–316. https://doi.org/10.1016/j.jmir.2015.06.006
Manzetti M, Ruffilli A, Barile F, Fiore M, Viroli G, Cappello L, Faldini C (2023) Sacroiliac Joint Degeneration and Pain After Spinal Arthrodesis: A Systematic Review. Clin Spine Surg. 36(4):169–182. https://doi.org/10.1097/BSD.0000000000001341
Cecchinato R, Redaelli A, Martini C, Morselli C, Villafañe JH, Lamartina C, Berjano P (2017) Long fusions to S1 with or without pelvic fixation can induce relevant acute variations in pelvic incidence: a retrospective cohort study of adult spine deformity surgery. Eur Spine J 26(Suppl 4):436–441. https://doi.org/10.1007/s00586-017-5154-z
Author information
Authors and Affiliations
Contributions
MG, JH, and DP made substantial contributions to the conception of the work; acquisition, analysis, and interpretation of data; drafted the work and revised it critically for important intellectual content; and all authors approved the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
The authors did not receive support from any organization for the submitted work. MG and JH have nothing to disclose. DP declares consulting fees from Alexion, Globus Medical, and SI Bone; institutional research support from Medtronic and Mizuho OSI; honoraria from SI Bone; and royalties from SI Bone and Springer.
Ethics approval and consent to participate
This observational study was reviewed and deemed exempt by the Institutional Review Board prior to the start of data collection. Due to the retrospective design, it provided no more than minimal risks to subjects, and thus a waiver of patient consent was granted.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Godlewski, M.W., Haselhuhn, J.J. & Polly, D.W. Standing versus supine pelvic incidence in adult spinal deformity patients. Eur Spine J 33, 3851–3856 (2024). https://doi.org/10.1007/s00586-024-08386-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-024-08386-4
Keywords
Profiles
- Jason J. Haselhuhn View author profile
- David W. Polly Jr. View author profile