Abstract
Purpose
The purpose of the study was to investigate several potential imaging biomarkers of CLBP that may be useful for diagnosis and treatment efficacy evaluation. Proton magnetic resonance spectroscopy (1H-MRS) was used to detect the content and ratio of creatine (Cr), choline (Cho), and lipid (Lip) in the multifidus muscle (Mm) in patients with CLBP and to test for relationships between these metabolites and pain severity and duration.
Methods
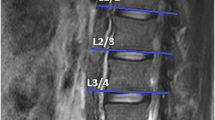
Sixty patients with CLBP (experimental group) and sixty-nine asymptomatic volunteers (control group) underwent routine diagnostic magnetic resonance imaging of the lumbar spine. 1H-MRS was acquired with single-voxel MR spectroscopy. The MRS region of interest for measuring Cho, Cr, and Lip concentrations was determined at the L4/5 multifidus muscle (Mm), bilaterally. The contents and ratios of Cr, Cho, and Lip in bilateral and ipsilateral-to-pain (or matched control side) Mm were obtained, and the integral ratios of different metabolites obtained by using Cr as an internal reference were statistically analyzed.
Results
There were no significant within-group differences in the contents and ratios of Lip, Cr, Cho, Lip/Cr, and Cho/Cr between the left and right Mm of the healthy control group (p > 0.05) or the CLBP group (p > 0.05). The CLBP group showed a much higher Lip and Lip/Cr ratio in the bilateral Mm compared to the healthy control group (p < 0.05) but there were no between-group differences in Cr, Cho, or the Cho/Cr ratio (p > 0.05). The severity of CLBP was correlated with Lip (p < 0.05).
Conclusion
Using 1H-MRS, we demonstrated higher Lip and Lip/Cr ratios in the Mm of patients with CLBP, compared to asymptomatic controls. Mm Lip was correlated with CLBP intensity. An increase in Lip in the Mm may be a characteristic finding in CLBP and may offer a useful prognostic marker for guiding rehabilitation strategies.





Similar content being viewed by others
References
Wu A, March L, Zheng X et al (2020) Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med 8(6):299
Altinel L, Kose KC, Ergan V, Işik C, Aksoy Y, Ozdemir A, Toprak D, Doğan N (2008) The prevalence of low back pain and risk factors among adult population in Afyon region Turkey. Acta Orthop Traumatol Turc 42(5):328–333
Igwesi-Chidobe CN, Kitchen S et al (2020) World Health Organisation Disability Assessment Schedule (WHODAS 2.0): development and validation of the Nigerian Igbo version in patients with chronic low back pain. BMC Musculoskelet Disord 21(1):755
D’hooge R, Cagnie B, Crombez G et al (2012) Increased intramuscular fatty infiltration without differences in lumbar muscle cross-sectional area during remission of unilateral recurrent low back pain. Man Ther 17(6):584–588
Uçar İ, Karartı C, Cüce İ, Veziroğlu E, Özüdoğru A, Koçak FA, Dadalı Y (2021) The relationship between muscle size, obesity, body fat ratio, pain and disability in individuals with and without non-specific low back pain. Clin Anat (New York, NY) 34(8):1201–1207
Liu H, Zhang J, Wang R et al (2020) Chin J Med Rev, 17(21):88–91
Takashima H, Takebayashi T, Ogon I et al (2018) Analysis of intra and extramyocellular lipids in the multifidus muscle in patients with chronic low back pain using MR spectroscopy. Br J Radiol 91(1083)
Masse-Alarie H, Beaulieu LD et al (2017) Repetitive peripheral magnetic neurostimulation of multifidus muscles combined with motor training influences spine motor control and chronic low back pain. Clin Neurophysiol 128(3):442–453
Panchal R, Denhaese R et al (2018) Anterior and lateral lumbar interbody fusion with supplemental interspinous process fixation: outcomes from a multicenter, prospective, randomized, controlled study. Int J Spine Surg 12(2):172–184
Dubé JJ, Amati F, Stefanovic-Racic M et al (2008) Exercise-induced alterations in intramyocellular lipids and insulin resistance:the athlete’s paradox revisited. Am J physiol Endocrinol metab 294(5):E882–E888
Agten CA, Rosskopf AB et al (2016) Quantification of early fatty infiltration of the rotator cuff muscles:comparison of multi-echo Dixon with single-voxel MR spectroscopy. Eur Radiol 26(10):3719–3727
Lamichhane B, Jayasekera D et al (2020) Multi-modal biomarkers of low back pain: a machine learning approach. NeuroImage Clin 29:102530
Lei Xiaoping (2012) Correlation between lumbar stability and lumbar dorsal degeneration. Guangzhou University of Traditional Chinese Medicine, 1–41 (in Chinese)
Conlee EM, Driscoll SW, Coleman Wood KA et al (2019) Posterior vertebral endplate fractures: a retrospective study on a rare etiology of back pain in youth and young adults. Pm R J Inj Funct Rehabil 11(6):619–630
White TL, Gonsalves MA et al (2021) The neurobiology of wellness:1H-MRS correlates of agency, flexibility and neuroaffective reserves in healthy young adults. Neuroimage 225:117509
Peterson P, Trinh L et al (2021) Quantitative 1H-MRI and MRS of fatty acid composition. Magn Reson Med 85(1):49–67
Chen S, Chen M, Wu X, Lin S, Tao C, Cao H, Shao Z, Xiao G (2022) Global, regional and national burden of low back pain 1990–2019: a systematic analysis of the Global Burden of Disease study 2019. J Orthop Transl 32:49–58
Meucci RD, Fassa AG, Faria NMX (2015) Prevalence of chronic low back pain: systematic review. Rev Saúde Pública 49:1–10
Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH (2010) The prevalence of chronic pain in united states adults: results of an internet-based survey. J Pain 11(11):1230–1239
Meucci RD, Fassa AG, Paniz VM et al (2013) Increase of chronic low back pain prevalence in a medium-sized city of southern Brazil. BMC Musculoskelet Disord 14(1):1–11
Heneweer H, Vanhees L, Picavet HSJ (2008) Physical activity and low back pain: a U-shaped relation? Pain 143(1):21–25
Heuch I, Hagen K, Heuch I, Nygaard Ø, Zwart JA (2010) The impact of body mass index on the prevalence of low back pain: the HUNT study. Spine 35(7):764–768
Knuth AG, Bacchieri G, Victora CG et al (2010) Changes in physical activity among Brazilian adults over a 5-year period. J Epidemiol Community Health 64(7):591–595
Hoy D, Bain C, Williams G et al (2012) A systematic review of the global prevalence of low back pain. Arthritis Rheum 64(6):2028–2037
Ahlawat S, Fritz J et al (2019) Magnetic resonance imaging biomarkers in musculoskeletal soft tissue tumors: review of conventional features and focus on nonmorphologic imaging. J Magn Reson Imaging 50(1):11–27
Shilei W, Zhenhua Li, Baodong Li et al (2020) Diagnosis of glioma by hydrogen proton magnetic resonance spectroscopy in 50 cases. Chin Med Instrum Inf 26(13):67–68
Tkáč I, Deelchand D et al (2020) Water and lipid suppression techniques for advanced 1H-MRS and MRSI of the human brain: experts’ consensus recommendations. NaMR Biomed 34(5):e4459
Bergmark A (1989) Stability of the lumbar spine: a study in mechanical engineering. Acta Orthop 60(230):1–54
Masse-Alarie H, Beaulieu LD, Preuss R, Schneider C (2017) Repetitive peripheral magnetic neurostimulation of Mm combined with motor training influences spine motor control and chronic low back pain. Clin Neurophysiol 128(3):442–453
Hildebrandt M, Fankhauser G, Meichtry A, Luomajoki H (2017) Correlation between lumbar dysfunction and fat infiltration in lumbar multifidus muscles in patients with low back pain. BMC Musculoskelet Disord 18(1):1–9
Weerasekara I, Hiller CE (2017) Chronic musculoskeletal ankle disorders in Sri Lanka. BMC Musculoskelet Disord 18:1–8
Collebrusco L, Lombardini R (2013) Osteopathic manipulative treatment and nutrition: An alternative approach to the irritable bowel syndrome. Health 5(6B):87–93
Faur C, Patrascu JM, Haragus H, Anglitoiu B (2019) Correlation between multifidus fatty atrophy and lumbar disc degeneration in low back pain. BMC Musculoskelet Disord 20(1):1–6
Teichtahl AJ, Urquhart DM, Wang Y, Wluka AE, Wijethilake P, O’Sullivan R, Cicuttini FM (2015) Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J 15(7):1593–1601
Lamichhanea B, Jayasekerab D, Jakesb R, Glassercd MF, Zhanga J, Yangd C, Grimesa D, Franka TL, Rayab WZ, Leuthardtabd EC, Hawasliae AH (2021) Multi-modal biomarkers of low back pain: a machine learning approach. NeuroImage Clin 29:102530
Peterson P, Trinh L, Månsson S et al (2021) Quantitative 1H-MRI and MRS of fatty acid composition. Magn Reson Med 85(1):49–67
Ahlawat S, Fritz J, Morris CD et al (2019) Magnetic resonance imaging biomarkers in musculoskeletal soft tissue tumors: review of conventional features and focus on nonmorphologic imaging. Magn Reson Imaging 50(1):11–27
Funding
Tai’an science and technology innovation development project, 2021NS229, Limeng Sun.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, L., Yan, H. & Zhang, Y. Magnetic resonance spectroscopy (MRS) of multifidus muscle metabolites in chronic low back pain (CLBP). Eur Spine J 32, 4397–4404 (2023). https://doi.org/10.1007/s00586-023-07933-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07933-9