Abstract
Study design
An ambispective review of consecutive cervical spine surgery patients enrolled in the Canadian Spine Outcomes and Research Network (CSORN) between January 2015 and September 2019.
Purpose
To compare complication rates of degenerative cervical spine surgery over time between older (> 65) and younger age groups (< 65).
Summary of background data
More elderly people are having spinal surgery. Few studies have examined the temporal nature of complications of cervical spine surgery by patient age groups.
Methods
Adverse events were collected prospectively using adverse event forms. Binary logistic regression analysis was utilized to assess associations between risk modifiers and adverse events at the intra-, peri-operative and 3 months post-surgery.
Results
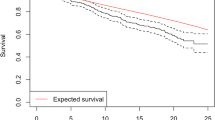
Of the 761 patients studied (age < 65, n = 581 (76.3%) and 65 + n = 180 (23.7%), the intra-op adverse events were not significantly different; < 65 = 19 (3.3%) vs 65 + = 11 (6.1%), p < 0.087. Peri-operatively, the < 65 group had significantly lower percentage of adverse events (65yrs (11.2%) vs. 65 + = (26.1%), p < 0.001). There were no differences in rates of adverse events at 3 months post-surgery (< 65 = 39 (6.7%) vs. 65 + = 12 (6.7%), p < 0.983). Less blood loss (OR = 0.99, p < 0.010) and shorter length of hospital stay (OR = 0.97, p < 0.025) were associated with not having intra-op adverse events. Peri-operatively, > 1 operated level (OR = 1.77, p < 0.041), shorter length of hospital stay (OR = 0.86, p < 0.001) and being younger than 65 years (OR = 2.11, p < 0.006) were associated with not having adverse events.
Conclusion
Following degenerative cervical spine surgery, the older and younger age groups had significantly different complication rates at peri-operative time points, and the intra-operative and 3-month post-operative complication rates were similar in the groups.

Similar content being viewed by others
References
Jeong GK, Bendo JA (2004). Spinal disorders in the elderly. Clin Orthop Relat Res 110–125.
Cheng JS, Chambless LB, McGirt MJ (2011). Trends in geriatric low back pain. AANS Neurosurgeon 20(2). http://www.aansneurosurgeon.org/200811/6/807.
Saleh A, Thirukumaran C, Mesfin A, Molinari R (2017) Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2320 patients. Spine J 17(8):1106–1112
Carreon LY, Puno RM, Dimar JR, Glassman SD, Johnson JR (2003) Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am 85:2089–2092
Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA (1992) Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am 74(4):536–543
Fehlings GM, Tetreault L, Nater A et al (2015) The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery 77(4):S1–S5
Saklad M (1941) Grading of patients for surgical procedures. Anesthesiology 2(3):281–284
Daabiss M (2011) American Society of Anaesthesiologists physical status classification. Indian J Anaesth 55:111–115
Wolters U, Wolf T, Stutzer H, Schroder T (1996) ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth 77(2):217–222
Alomari S, Liu A, Westbroek E et al (2021) Influence of sex on early outcomes of elective lumbar fusions: an updated propensity-matched and subgroup analysis. World Neurosurg 150:e388–e399. https://doi.org/10.1016/j.wneu.2021.03.025
Wang MC, Chan L, Maiman DJ et al (2007) Complications and mortality associated with cervical spine surgery for degenerative disease in the United States. Spine 32:342–347
Nakashima H, Tetreault LA, Nagoshi N et al (2016) Does age affect surgical outcomes in patients with degenerative cervical myelopathy? results from the prospective, multicenter aospine international study on 479 patients. J Neurol Neurosurg Psychiatry 87(7):734–740
Ondeck NT, Bohl DD, Bovonratwet P et al (2018) general health adverse events within 30 days following anterior cervical discectomy and fusion in us patients: a comparison of spine surgeons’ perceptions and reported data for rates and risk factors. Global Spine J 8(4):345–353
Pastorelli F, Di Silvestre M, Plasmati R et al (2011) The prevention of neural complications in the surgical treatment of scoliosis: the role of the neurophysiological intraoperative monitoring. Eur Spine J 20(1):105–114
Mattei TA (2013) Does ‘age’ really matter? Important considerations regarding clinical outcomes in spine surgery in the elderly population. Spine J 13(8):992
Boakye M, Patil CG, Santerelli J et al (2008) Cervical spondylotic myelopathy: complications and outcomes after spinal fusion. Neurosurgery 62(2):455–461
Lad SP, Patil CG, Berta S et al (2009) National trends in spinal fusion for cervical spondylotic myelopathy. Surg Neurol 71(1):66–69
Marquez-Lara A, Nandyala SV, Fineberg SJ, Singh K (2014) Current trends in demographics, practice, and in-hospital outcomes in cervical spine surgery: a national database analysis between 2002 and 2011. Spine (Philadelphia, Pa. 1976) 39(6):476–481
Campbell PG, Malone J, Yadla S et al (2011) Comparison of ICD-9—based, retrospective, and prospective assessments of perioperative complications: assessment of accuracy in reporting. J Neurosurg Spine 14:16–22
Wang MC, Chan L, Maiman DJ et al (2007) Complications and mortality associated with cervical spine surgery for degenerative disease in the United States. Spine (Philadelphia, Pa. 1976) 32(3):342–347
Bernstein DN, Thirukumaran C, Saleh A et al (2017) Complications and readmission after cervical spine surgery in elderly patients: an analysis of 1786 patients. World Neurosurg 103:859–868
Hartig D, Batke J, Dea N et al (2015) Adverse events in surgically treated cervical spondylopathic myelopathy: a prospective validated observational study. Spine (Phila Pa 1976) 40(5):292–298
Soto-Perez-de-Celis E, Li D, Yuan Y et al (2018) Functional versus chronological age: geriatric assessments to guide decision making in older patients with cancer. Lancet Oncol 19(6):e305–e316
Rothrock RJ, Steinberger JM, Badgery H et al (2019) Frailty status as a predictor of 3-month cognitive and functional recovery following spinal surgery: a prospective pilot study. Spine J 19(1):104–112
James LA, Levin MA, Lin HM, Deiner SG (2019) Association of preoperative frailty with intraoperative hemodynamic instability and postoperative mortality. Anesth Analg 128(6):1279–1285
Velanovich V, Antoine H, Swartz A et al (2013) Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 183(1):104–110
Di Capua J, Somani S, Kim JS et al (2017) Elderly age as a risk factor for 30-day postoperative outcomes following elective anterior cervical discectomy and fusion. Global Spine J 7(5):425–431
Harris OA, Runnels JB, Matz PG (2001) Clinical factors associated with unexpected critical care management and prolonged hospitalization after elective cervical spine surgery. Crit Care Med 29(10):1898–1902
Veronesi F, Borsari V, Martini L et al (2021) The impact of frailty on spine surgery: systematic review on 10 years clinical studies. Aging Dis 12(2):625–645
Alsubaie H, Goldenberg M, Grantcharov T (2019) Quantifying recall bias in surgical safety: a need for a modern approach to morbidity and mortality reviews. Can J Surg 62(1):39–43
Acknowledgements
We would like to acknowledge CSORN contributors and staff for making available this data for our review
Funding
No funding was used for the execution of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ajoku, U., Johnson, M.G., McIntosh, G. et al. Temporal analysis of complication rates of cervical spine surgery for degenerative spine disease between younger and older cohorts using the CSORN registry: Is age just a number?. Eur Spine J 32, 3583–3590 (2023). https://doi.org/10.1007/s00586-023-07882-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07882-3