Abstract
Purpose
Clinicians detect scoliosis worsening over time using frequent radiographs during growth. Arms must be elevated when capturing sagittal radiographs to visualize the vertebrae, and this may affect the sagittal angles. The aim was to systematically review the published evidence of the effect of arm positions used during radiography on spinal alignment parameters in healthy participants and those with AIS.
Methods
Design was registered in PROSPERO (CRD42022347494). A search strategy was run in Medline, Embase, CINAHL, and Web of Science. Healthy participants ≥ 10 years old and participants with AIS between 10 and 18 years old, with Cobb angles > 10° were included. Study quality was assessed using the Appraisal tool for Cross-Sectional Studies (AXIS). Meta-analysis was performed where possible.
Results
Overall, 1332 abstracts and 33 full texts were screened. Data was extracted from 7 included studies. The most common positions were habitual standing, fists on clavicle, and active (arms raised unsupported). Kyphosis, lordosis, and sagittal vertical axis (SVA) were most measured. Meta-analysis showed significantly decreased kyphosis (SMD = 0.78, 95%CI 0.48, 1.09) and increased lordosis (SMD = − 1.21, 95%CI − 1.58, − 0.85) when clavicle was compared to standing. Significant posterior shifts in SVA were shown in clavicle compared to standing (MD = 30.59 mm, 95%CI 23.91, 37.27) and active compared to clavicle (MD = − 2.01 mm, 95%CI − 3.38, − 0.64). Cobb angles and rotation were rarely studied (1 study).
Conclusion
Meta-analysis evidence showed elevated arm positions modify sagittal measurements compared to standing. Most studies did not report on all relevant parameters. It is unclear which position best represent habitual standing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a 3D structural disorder of the spine with lateral curvature of over 10°, vertebral rotation, and sagittal changes that affects 2–3% of adolescents [1]. Patients with AIS receive numerous x-rays throughout their treatment to establish the diagnosis and monitor curve progression, which is defined as a five degree increase in Cobb angle compared to previous radiographs. This exposes them to harmful radiation throughout their growing years. Particularly in young children, increased exposure to radiation has been shown to increase the incidence of cancer [2]. Ronckers et al. followed 5513 females with scoliosis, finding they were exposed to an average of 22.9 radiographs per person during treatment and follow-up [3]. Similarly, a Milwaukee-based program following 13 females with AIS estimated that each patient had 22 films taken during a three-year course and showed increased risk for leukemia (3.4%), stomach/gastrointestinal (1.3%), lung (7.5%), and breast cancers (110%) [4]. A 2012 SOSORT Consensus Report stated that scoliosis experts agreed x-rays should be performed at the time of first evaluation and then every 6–12 months afterward to minimize total number of x-rays [5].
All radiographic measurements, when imaging patients with AIS, depend on being able to see the detail of key vertebral landmarks while ensuring that the arm position used during the radiograph does not affect the sagittal and frontal spinal parameters. Sagittal views are necessary to measure spinal parameters such as kyphosis and lordosis. The Scoliosis Research Society (SRS) Radiographic Measurement Manual states an ideal standing lateral radiograph should include vertebrae C7 to S1 and the ability to visualize C0–C1 and the hip joints is optimal [6]. Key landmarks to assess kyphosis and lordosis include vertebrae T1/T2, T4/T5, T10-T12, L1 and the sacrum. Another key sagittal parameter includes sagittal vertical axis (SVA), requiring the x-ray to show the anterior–posterior position of vertebrae C7 relative to the superior posterior corner of the sacrum [7]. Historically, only frontal radiographs were collected, but research has demonstrated that sagittal deformity is more strongly related to quality of life [8]. Recently, low-dose radiographic systems have become available that simultaneously acquire a frontal and a sagittal image that reconstruct the spine in 3D [9]. It is necessary to have the arms elevated when using such systems in order to expose the whole sagittal plane of the spine and avoid the arms from overlapping with vertebral bodies. However, raising the arms has been shown to affect sagittal angles [7, 10,11,12,13,14,15,16]. Ideally, patient positioning during standing radiographs would reflect habitual posture parameters, or at minimum, be similar to the standing posture used to monitor frontal angles historically.
It would be beneficial to know which arm position used during imaging will simultaneously allow exposing the hands in order to determine skeletal maturity. Assessment of skeletal maturity can be done using the Sanders Skeletal Maturity Staging System. This system breaks down the fusion of the epiphyseal growth plates into 8 stages and can be used to determine how much growth a patient with AIS has left, and thus, estimate the scoliosis progression risk [17]. Risser staging has traditionally been the primary marker of skeletal maturity utilized in decision making for treatment of AIS because it is scored on routine frontal spine radiographs. This method requires determining ossification of the left iliac apophysis that is associated with the patient’s state of spinal maturity [18]. Compared to Sanders assessment, Risser staging has been shown to result in suboptimal treatment in one in every four patients, with the vast majority being undertreated [18].
The aim of this study was to review and synthesise the published evidence of the effect of arm positions used during radiography on spinal alignment parameters compared to habitual standing in healthy populations and populations with AIS. Spinal alignment parameters of interest include Cobb angle, whole thoracic kyphosis, T5–T12 kyphosis, lordosis, AVR twist, and any other spinopelvic parameters such as sagittal vertical axis (SVA). Sagittal angles are a primary parameter of interest. We hypothesized that:
-
1.
We will be able to identify an arm position that will allow exposing the hands for skeletal maturity assessment that does not significantly alter vertebral rotation, or any frontal or sagittal angles compared to habitual standing, and
-
2.
The largest differences due to elevating the arms will be detected using sagittal angles (kyphosis and lordosis) compared to frontal or transverse measurements.
Methods
Design and methods used for this systematic review were registered with the International Prospective Register of Systematic Reviews (PROSPERO CRD42022347494). Reporting is compliant with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [19].
Search strategy
The search employed sensitive topic-based strategies designed for each database from inception to June 29, 2022. Databases include Cumulated Index to Nursing and Allied Health Literature (CINAHL) (EBSCO), Embase (OVID), Medline (OVID), and Web of Science (All databases). The search syntax used in each database is reported in the Appendix. The strategy includes terms and keywords identified by an expert on scoliosis, a master’s student, and by librarian Liz Dennett from the Health Science library at University of Alberta. The search for this review was designed by identifying terms related to the scoliosis population, imaging methods, measurements of interest, and patient positioning. To limit to the most relevant references, we eliminated any populations where scoliosis was a symptom of another disease. Covidence was used to import all articles, and duplicates were eliminated automatically. Covidence is a web-based collaboration software platform that streamlines the production of systematic and other literature reviews [20].
Study selection criteria
Studies were included if they focused on healthy participants aged ≥ 10 years old and participants with AIS between the ages of 10 and 18 years old with Cobb angles > 10°. Studies comparing the effect of patient positioning and arm positioning for full spine imaging, limited to standing, were included. Cohort or cross-sectional study designs where positions were compared within a short time interval were included. Studies with participants diagnosed with spinal disorders other than AIS, injuries to the lower body, and studies with pregnant participants were excluded.
Selection process
Two independent reviewers used Covidence to select relevant articles during a titles and abstract screening stage using the eligibility criteria outlined above. Reviewers were blinded to selections. For references meeting the criteria as identified by both reviewers, the two independent reviewers screened full text articles uploaded to Covidence. At both screening stages, if reviewers disagreed, they first had a consensus discussion, and if needed, a third reviewer made the final decision. Percent agreement was calculated between reviewers.
Data extraction
Two reviewers independently extracted study information using a piloted Google spreadsheet. Reviewers first tried extraction on three papers and discussed results before continuing further. During extraction, if reviewers disagreed, they attempted to reach consensus via discussion, then consulted the opinion of a third reviewer if needed. The reviewers extracted the following study information (where available); sample descriptions including age and sex, diagnosis, curve type and severity, imaging methods, spinal measurements, descriptions of testing positions, and reported statistics comparing the positions.
Scoliosis measurement parameters including maximum curve angle, axial vertebral rotation (AVR), sagittal angles including kyphosis and lordosis, SVA, and any other relevant spino-pelvic parameters were extracted. Statistical results comparing positions were extracted. Kyphosis and lordosis angles were considered the primary outcomes.
Risk of bias assessment
The Appraisal tool for Cross-Sectional Studies (AXIS) was used to determine the quality of cross-sectional studies [21]. The AXIS quality appraisal was scored out of 12 for the 12 questions referring to methodological quality to avoid focusing on reporting quality (Table 1). We selected “positive” when the answer to the question was clear and precise. An “unclear” result was given when the answer to the question was vague. A “negative” result was given if the study did not report on the question. Each study was given a final score out of 12, and a corresponding rating. Scores ranging from 1 to 3 were rated low, scores from 4 to 7 were moderate, and scores above and including 8 were rated high quality. AXIS has been shown reliable in comparison to an adapted Newcastle–Ottawa Scale (NOS) [22]. Both reviewers read the manual on AXIS grading, reviewed one article, compared results, and then appraised the rest of the papers. Both reviewers were trained in determining how to rate methodological questions sufficiently [21]. Both reviewers independently completed the appraisal for each selected article. Disagreements in quality scoring were resolved by consensus.
Data synthesis
Summary tables were prepared: including levels of evidence summary statements based on quality assessment, study characteristics, extracted descriptive statistics, and outcome characteristics reported in and missing from current literature. Meta-analysis was performed for each measurement parameter if more than two studies reported on a similar spinal parameter and arm positions using RevMan 5.4.1 (The Cochrane Collaboration, version September 2020. Available at revman.cochrane.org). We used a random-effect meta-analysis of standardized mean differences for kyphosis and lordosis due to differences in measurement scales reported in the articles. In contrast, a random-effect meta-analysis of the mean differences was reported for SVA measurements due to consistent measurement scales used for this parameter. Point estimates and 95% confidence intervals were reported for each meta-analysis. Chi-square tests of heterogeneity were performed and I2 was reported for each meta-analysis. I2 results were interpreted as follows; 0–40% may not be considerable heterogeneity, 30–60% may represent moderate heterogeneity, 50–90% may represent substantial heterogeneity, and 75–100% represents considerable heterogeneity [23].
Levels of evidence summary statements were formulated for other results. As adapted by Cornelius et al., the summary of results was graded using the levels of evidence (Table 2) considering the methodological quality and the consistency of the results across studies for each parameter and positions comparisons [24].
Results
Study selection
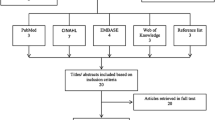
A total of 1440 studies were identified across all databases (MEDLINE = 78, EMBASE = 338, CINAHL = 65, WEB OF SCIENCE = 851) (Fig. 1). After 108 duplicates were excluded, 1332 abstracts and titles were screened by the two reviewers. After exclusion of 1299 irrelevant records, 33 full texts were screened by the two reviewers, and 26 studies were excluded. Seven papers were ultimately included for data extraction [7, 13, 14, 16, 25,26,27]. Percentage of agreement between the reviewers was 97.5% for title and abstract screening and 100% for full text screening.
Study description
Study characteristics including sample descriptions, disease characteristics, and methodology are shown in Table 3. Six arm positions were analyzed across included studies. These include: habitual standing, 30° or 45° active flexion, 30° passive flexion, fists to clavicle, and hands on wall. The most common positions reported in comparison studies were habitual standing (5 studies [13, 14, 25,26,27]), fists on clavicle (5 studies [7, 13, 25,26,27]), and active positions where the arms are raised and unsupported (3 studies [7, 13, 14]) (Table 3). The most commonly measured spinal alignment parameters were kyphosis (5 studies [7, 13, 16, 25, 27]), lordosis (5 studies [7, 13, 16, 25, 27]), and SVA (4 studies [7, 13, 14, 16]) (Table 4). Descriptive and comparative statistics for each of the imaging spine alignment outcomes extracted for the different positions are presented in Table 4.
Other spino-pelvic parameters were also assessed. Two studies assessed pelvic incidence, sacral slope, and pelvic tilt [7, 16] comparing Active 45° or Hands on wall to the Clavicle position, respectively (Online Resource 1). Further, Pasha et al. evaluated frontal balance, lateral pelvic tilt (LPT) and, and anterior pelvic plane (APP) inclination between Hands on wall and the Clavicle position [16]. Pasha et al. and Faro et al. both detected a significant sacral slope degree increase comparing the hands on wall and active 45°, respectively, to the clavicle position (p < 0.05) [7, 16] Wojciech et al. found no systematic differences for trunk vertical inclination angle in the sagittal plane between standing and the clavicle position [26].
Quality appraisal
Of the seven studies, two were rated as high methodological quality, three as moderate, and two as low quality (Table 1). Our AXIS results commonly flagged questions regarding response rate, addressing biases, and the lack of descriptions justifying sample size. Alternatively, AXIS positively scored questions justifying results and conclusions, as well as appropriate study design choices.
Meta-analysis estimates
Kyphosis
-
There is limited evidence from 2 moderate [13, 25] and 1 low quality studies [27] of a medium effect size of 0.78 [95% CI 0.48, 1.09, p < 0.01] where kyphosis is smaller in the clavicle position when compared to habitual standing. (Fig. 2a) This analysis had low heterogeneity (I2 = 0%).
-
Similarly, there is moderate evidence from 1 high [16] and 2 moderate quality studies [7, 13] of a non-significant and negligible effect size of 0.03 [95% CI − 0.38, 0.45, p = 0.88] for difference in kyphosis between the clavicle compared to the active position (Fig. 2b). This analysis has substantial heterogeneity (I2 = 56%).
Lordosis
-
There is limited evidence from 2 moderate [13, 25] and 1 low quality study [27] of a large effect size of − 1.21 [95% CI − 1.58, − 0.85, p < 0.01] where lordosis is larger in the clavicle position compared to habitual standing (Fig. 2c). This analysis has low heterogeneity (I2 = 20%).
-
There is moderate evidence from 1 high [16] and 2 moderate quality studies [7, 13] of a non-significant and negligible effect size of − 0.06 [95% CI − 0.32, 0.21, p = 0.68] about the difference in lordosis between the clavicle compared to the active positions (Fig. 2d). This analysis has low heterogeneity (I2 = 0%).
SVA
-
There is limited evidence from 2 moderate [13, 25] and 1 low quality study [27] of a large mean difference of 30.59 mm [95% CI 23.91, 37.27, p < 0.01] where the SVA is shifted more posteriorly in the clavicle position compared to habitual standing (Fig. 2e). This analysis however presented substantial heterogeneity (I2 = 67%).
-
There is also moderate evidence from 1 high [16] and 2 moderate quality studies [7, 13] of a significant but small mean difference of − 2.01 mm [95% CI − 3.38, − 0.64, p = 0.004] where SVA is shifted more posteriorly in active positions compared to the clavicle position (Fig. 2f). This analysis has substantial heterogeneity (I2 = 83%).
Level of evidence summary statements
A total of 24 strength of evidence summary statements were formulated based on the number and the quality of studies to include the evidence from studies contributing results which could not be meta-analysed with those in the meta-analysis that examined each spinal alignment outcome between standing positions (Table 5). No summary statement offered strong evidence, 14 offered limited strength and 7 moderate strength of evidence. Sixteen statements demonstrated evidence of no differences, two statements demonstrated conflicting evidence, and one insufficient evidence statement between compared positions.
Overall, for comparisons to habitual standing, one statement showed no significant differences vs habitual standing in whole thoracic kyphosis in Passive 30° and Active 30°. One statement each showed significant increases in lordosis in the clavicle position and significant posterior shifts in SVA in Active 45° or 30°, Passive 30° and Clavicle compared to habitual standing. Other summary statements for comparisons to habitual standing were either conflicting (Kyphosis vs Clavicle) or showed no difference (kyphosis and lordosis vs Passive and Active 30°).
Summary statements about comparisons of elevated arms positions to the clavicle positions found: decreased T4/T5 kyphosis with Hands on wall and Active 45°; posterior shift of SVA with Active 30° or 45° and Hands on wall; decreased sacral slope in Active 45° and Hands on wall; and decreased Sagittal T1 tilt angle in Hands on wall. Other summary statements including comparisons among arms-elevated positions and Clavicle were either conflicting (whole kyphosis vs Passive 30°, Active 30° or 45° and Hands on wall) or showed no difference (lordosis for Active 30° or 45o and Hands on wall; lumbar and thoracic AVR or apical vertebral translation (AVT) in Hands on wall; pelvic incidence angle in Active 45° and Hands on wall; in four other spino-pelvic parameters in Hands on wall and one other spino-pelvic parameter in Active 45°).
Summary statements comparing Active 30° to Passive 30° found no differences in kyphosis and lordosis but a posterior SVA shift in Active compared to Passive 30o.
For eight of the parameters of interest stated a priori, summary statements were formulated to quickly identify positions tested to date and help researchers determine which positions have not yet been studied (no evidence) (Table 6). Positions that have not yet been reported depending on the alignment parameters are hands actively raised above the shoulders, hands on wall or blocks, hands to chin, hands to cheeks, and hands to eyebrows. Among hand raised positions, which could allow assessing skeletal maturity, only hands on wall has been previously studied [16]. Studies seldom reported on all spinal parameters we identified as of interest a priori, most notably, frontal (maximum curve angle) and transverse angles have been rarely studied (AVR twist) (Table 6). Only one study to date assessed the effects on curve angle, AVT, and AVR [16].
Discussion
The results of our systematic review found limited evidence on arm positions in adolescents that compared spinal parameters to habitual standing. Of the few positions that are discussed in the existing literature, our meta-analysis shows there are also mixed results when using these positions. The spinal parameters most commonly discussed are kyphosis, lordosis, and SVA—all sagittal parameters. We prioritized finding the effect of positioning on sagittal parameters, but little to no research has been published on the effect of arm positions on frontal or transverse plane parameters like Cobb angle, AVT, and AVR or AVR twist, respectively. Our meta-analysis results show that the most commonly used arm position during radiography clinically, the clavicle position, significantly decreases kyphosis and increases lordosis compared to habitual standing. Consequently, this position also significantly shifts SVA posteriorly. Our meta-analysis results show that active arm positions, when compared to the clavicle position, show non-significant decreases in kyphosis and increases in lordosis (Fig. 2b, d). Further, active positions significantly shift SVA posteriorly when compared to the clavicle position (Fig. 2f). There are a number of positions that have not been tested in the literature that would allow for the hands to be exposed for the scoring of skeletal maturity. Pasha et al. reported results for the hands-on wall position, and is the lone study comparing a position that could expose the hands but did not compare spinal alignment parameters in this position to habitual standing [16].
It is important to ensure that arm positioning during radiography is not having significant effects on spinal alignment parameters for a number of reasons. If conclusions about treatment for patients with AIS is made based upon radiograph measurements that are not accurately reflecting habitual standing or the position adopted during prior radiographs, this could result in incorrect treatment options recommendation in the clinic. Accurate parameters are needed to construct custom braces and plan surgeries for AIS. If these are inaccurate based on changing arm positioning, brace construction may be inappropriate and cause this treatment to be uncomfortable and unsuccessful. If patients with AIS are nearing indications of surgery, which is defined by the SRS as a curve degree of over 45°–50° and/or those who are at high risk of continued worsening, precise radiograph results are imperative to determine if surgery will be recommended [28]. Similarly, if patients are consistently changing arm positions over the course of treatment, it may be hard to determine curve degree over time and adequately detect progression. For these reasons, it is critical to guarantee the arm position used during radiography is consistent and a reflection of habitual standing parameters.
A 2017 literature review compared arm positions during radiography [29]. The review included 22 studies using radiograph measurements and 16 studies that used photogrammetry measurements. All populations including adults, adolescents, scoliotic, and healthy participants were included. Our review differs most notably from this review because we included only the adolescent populations within the search. Our reviews retrieved only one study in common and, we did not miss any relevant articles that were retrieved by Okazaki and Porto [29]. This 2017 literature review included the comparison of radiography and photogrammetry imaging methods and was only interested in extracting thoracic kyphosis and lordosis measurements. Like our review, it was concluded there is a lack of standardized patient positioning during imaging. Okazaki and Porto suggested that, due to the lack of studies with comparisons among different arm positioning, radiographs be performed with arms flexed and fists resting on the clavicles, ensuring changes in the sagittal vertical axis and pelvic parameters do not occur [29]. Although a conclusive statement was made, it remains unclear how to ensure that any changes are not occurring in the SVA and/or other pelvic parameters during imaging in the clavicle position. Our review results concur with Faro et al., who stated that although the fingers on clavicle position is commonly used in clinics and in the literature [7], this position is not a reflection of habitual standing due to significant decreases in kyphosis, increases in lordosis, and shifts in SVA reported in adolescents.
The literature found in this review did not use consistent imaging methods. Only three studies used radiographs to detect differences in spinal parameters [7, 14, 16]. The remaining studies used varying surface topography methods [25,26,27] or reflective markers [13]. Across the studies we reviewed, only one justified the sample size [16]. Among studies that did not justify sample, the size ranged from 15 to 695 participants. Small samples (< 30 participants) may be insufficient to detect clinically important differences between positions. The choice and description of methods used for measuring the different spinal parameters were found to be inconsistent across the literature. Due to methodological inconsistencies across the studies we reviewed, and according to AXIS scoring, only two studies were deemed high quality, three were deemed moderate, and two were deemed low quality studies. It is recommended for future research to use consistent imaging methods and spinal parameter measuring techniques when comparing arm positions to habitual standing. The SRS Radiographic Measurement Manual and the SRS-Schwab Adult Spinal Deformity Classification offer clear instructions obtaining relevant measurements and we recommend these measurements be used in future studies [6, 30]. Sample size estimation strategies should be presented, and studies planned with adequate power to detect clinically important differences in the relevant parameters used in comparing positions.
The summary statements of our review show there are non-significant effects on lordosis among the commonly used arms elevated positions (clavicle, active, and passive positions). However, our statement comparing the clavicle position to habitual standing is in agreement with our meta-analysis, by showing a significant increase in lordosis measurements in the clavicle position compared to habitual standing. This suggests that most arm-elevated positions may change the spinal sagittal alignment compared to habitual standing. One study in our review also showed a significant decrease in kyphosis during the hands-on wall position compared to the clavicle position, but our meta-analysis did not show any significant differences in kyphosis measurements when comparing similar active positions [16]. Our summary statements show a conflicted strength of evidence with two studies [25, 27] showing significant decreases and one finding no difference [13] in whole thoracic kyphosis when comparing the clavicle position to habitual standing. Our meta-analysis, however, shows significant decreases in kyphosis across the literature when combining the evidence comparing these positions. Most of the literature shows significant posterior shifts in SVA in all positions with elevated arms measured compared to habitual standing [7, 13, 14] (Table 4). When the arms are held in active positions, there appears to be more important posterior shifts in the sagittal profile, and thus, such positions do not represent habitual standing. Similarly, the literature shows that the clavicle position, when compared to active positions and when the hands are held on the wall, are also not interchangeable [7, 16]. Only one study directly compared active and passive positions, showing that while there are no significant effects on kyphosis and lordosis, active arm elevation led to a significantly larger posterior shift in SVA [13]. The majority of the literature found on this topic did not compare enough positions and does not report on all relevant spinal parameters (Table 6). Only one paper addresses sex differences without reporting data, stating differences between the clavicle position and standing were significant regardless of sex [26]. A significant gap in knowledge remains.
Our review was specific to adolescent populations, limited to arm positions while standing. By eliminating adult populations and sitting or lying positions, we limited results in our search. This being said, we only included adolescents because they are the population effected by AIS for which treatment decisions should be made based on regular radiograph comparisons during growth. We could have missed studies in our search due to excluding languages other than English. Including more databases could have resulted in finding more research. Articles and abstracts were screened by two independent and blinded reviewers. Both reviewers were novice but reached good levels of agreement. Our meta-analysis results may be affected by the use of differing measurement methodologies between studies. Notably, the standardized mean difference was reported for kyphosis and lordosis analysis due to a difference in the reporting of these parameters between the studies. Our chosen quality appraisal tool, AXIS and scoring strategy, focuses mainly on the methodological quality of the chosen methods and analysis and is less focused on the quality of reporting [21]. We were then able to accurately determine the methodological quality of the studies reported.
Our review shows sagittal spinal parameters, most notably posterior shifts in SVA, are more prone to change when raising the arms in comparison to habitual standing measurements. Similarly, there are reported differences among positions that raise the arms and therefore prevent these positions from being used interchangeably. Therefore, spinal parameters in radiographs using these positions do not accurately reflect habitual standing. No position exposing the hands during imaging have been compared to habitual standing, and only the hands on wall position has been compared to other arm positions. Limited literature in this topic that is specific to AIS reinforces the need for more research and it remains unclear which arm position best represents habitual standing during radiography in patients with AIS.
Data and/or code availability
Data extraction information is provided within the paper and tables and supplementary data.
References
Weinstein SL, Dolan LA, Cheng JC et al (2008) Adolescent idiopathic scoliosis. Lancet 371:1527–1537. https://doi.org/10.1016/S0140-6736(08)60658-3
Levy AR, Goldberg MS, Mayo NE et al (1996) Reducing the lifetime risk of cancer from spinal radiographs among people with adolescent idiopathic scoliosis. Spine 21:1540–1547
Ronckers CM, Land CE, Miller JS et al (2010) Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res 199:83–90
Nash CLJ, Gregg EC, Brown RH, Pillai K (1979) Risks of exposure to X-rays in patients undergoing long-term treatment for scoliosis. JBJS 61:371–374
Knott P, Pappo E, Cameron M et al (2014) SOSORT 2012 consensus paper: reducing x-ray exposure in pediatric patients with scoliosis. Scoliosis 9:4. https://doi.org/10.1186/1748-7161-9-4
O’Brien M, Kulklo T, Blanke K, Lenke L (2008) Radiographic measurement manual. spinal deformity study group radiographic measurement manual 120
Faro FD, Marks MC, Pawelek J, Newton PO (2004) Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine 29:2284–2289
Tao F, Wang Z, Li M et al (2012) A comparison of anterior and posterior instrumentation for restoring and retaining sagittal balance in patients with idiopathic adolescent scoliosis. J Spinal Disord Tech 25:303–308. https://doi.org/10.1097/BSD.0b013e3182204c3e
Gajny L, Ebrahimi S, Vergari C et al (2019) Quasi-automatic 3D reconstruction of the full spine from low-dose biplanar X-rays based on statistical inferences and image analysis. Eur Spine J 28:658–664. https://doi.org/10.1007/s00586-018-5807-6
Saito T, Uesugi M, Ishida K et al (2009) Does the fists-on-clavicles position represent a functional standing position? Spine 34:808–812. https://doi.org/10.1097/BRS.0b013e31819e2191
Kaneko K, Aota Y, Sekiya T et al (2016) Validation study of arm positions for evaluation of global spinal balance in EOS imaging. Eur J Orthop Surg Traumatol 26:725–733. https://doi.org/10.1007/s00590-016-1813-8
Aota Y, Saito T, Uesugi M et al (2011) Optimal arm position for evaluation of spinal sagittal balance. J Spinal Disord Tech 24:105–109. https://doi.org/10.1097/BSD.0b013e3181da36c4
Marks M, Stanford C, Newton P et al (2009) Which lateral radiographic positioning technique provides the most reliable and functional representation of a patient’s sagittal balance? Spine 03622436(34):949–954. https://doi.org/10.1097/BRS.0b013e318199650a
Marks MC, Stanford CF, Mahar AT, Newton PO (2003) Standing lateral radiographic positioning does not represent customary standing balance. Spine 28:1176–1182. https://doi.org/10.1097/00007632-200306010-00018
Vedantam R, Lenke LG, Bridwell KH et al (2000) The effect of variation in arm position on sagittal spinal alignment. Spine 25:2204–2209
Pasha S, Capraro A, Cahill P et al (2016) Bi-planar spinal stereoradiography of adolescent idiopathic scoliosis: considerations in 3D alignment and functional balance. Eur Spine J 25:3234–3241. https://doi.org/10.1007/s00586-016-4661-7
Sanders JO, Khoury JG, Kishan S et al (2008) Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am 90A:540–553
Minkara A, Bainton N, Tanaka M et al (2020) High risk of mismatch between sanders and Risser staging in adolescent idiopathic scoliosis: Are we guiding treatment using the wrong classification? J Pediatric Orthopaedics 40:60–64. https://doi.org/10.1097/BPO.0000000000001135
Page MJ, Moher D, Bossuyt PM, et al (2021) Suplemento do Guia de Elaboração PRISMA2020. The BMJ 372:Data supplement
Innovation VH Covidence systematic review software. www.covidence.org
Downes MJ, Brennan ML, Williams HC, Dean RS (2016) Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 6:e011458. https://doi.org/10.1136/bmjopen-2016-011458
Moskalewicz A, Oremus M (2020) No clear choice between Newcastle-Ottawa Scale and Appraisal Tool for Cross-Sectional Studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J Clin Epidemiol 120:94–103. https://doi.org/10.1016/j.jclinepi.2019.12.013
Green S, Sussex W (2010) 27- Cochrane of Systematic Reviews. 6:143–148
Cornelius LR, van der Klink JJL, Groothoff JW, Brouwer S (2011) Prognostic factors of long term disability due to mental disorders: a systematic review. J Occup Rehabil 21:259–274. https://doi.org/10.1007/s10926-010-9261-5
Abe Y, Satoh S, Yamada K (2016) Does lateral whole-spine radiograph taken with fists-on-clavicle position represent reliable global sagittal spinal alignment? Eur Spine J 25:S434–S435. https://doi.org/10.1007/s00586-016-4723-x
Wojciech G, Czyżak I, Glinkowska B et al (2013) The position with fingers on clavicles has no influence on vertical trunk inclination and kyphosis but significantly changes surface topography lordosis angle. Scoliosis 17487161(8):O21–O22. https://doi.org/10.1186/1748-7161-8-S2-O21
Asano F, Abe Y, Sato S et al (2015) Does lateral whole-spine radiograph taken by fists-on-clavicle position represent reliable global sagittal spinal alignment in adolescent patients? Scoliosis 10:1
Society SR (2015) Scoliosis Research Society E-Textbook, 1.1. Scoliosis Research Society
Porto AB, Okazaki VHA (2017) Procedures of assessment on the quantification of thoracic kyphosis and lumbar lordosis by radiography and photogrammetry: a literature review. J Bodyw Mov Ther 21:986–994. https://doi.org/10.1016/j.jbmt.2017.01.008
Schwab F, Ungar B, Blondel B et al (2012) Scoliosis research society-schwab adult spinal deformity classification: a validation study. Spine 37:1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Acknowledgements
We thank University of Alberta Health Sciences Librarian, Liz Dennett, who helped build the search for this review.
Funding
Financial support was received from the Women in Scholarship, Engineering, Science, and Technology student program at the University of Alberta for Annika Visser. The faculty of Rehabilitation Medicine and the Alberta Graduate Excellence Scholarship financially supported Brianna Fehr through Graduate Research Assistantship Funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, ECP, BJF; methodology, ECP, BJF; Screening, BJF AV; data extraction, BJF, AV; formal analysis, BJF, AV; writing—original draft preparation, BJF; writing—review and editing, ECP, BJF, AV; supervision, ECP; project administration, ECP; All authors have read and agreed to the published version of the manuscript. This research has not yet been published, submitted, or accepted for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
Ethical approval is not required for this systematic review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fehr, B.J., Visser, A. & Parent, E.C. Systematic review of imaging comparisons of spinal alignment among standing positions in healthy adolescents or adolescents with idiopathic scoliosis: SOSORT 2023 award winner. Eur Spine J 32, 3941–3960 (2023). https://doi.org/10.1007/s00586-023-07815-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07815-0