Abstract
Purpose
The aim of the study was to investigate whether MRI findings together with epidemiological data could help in differentiating between tuberculous and pyogenic spondylodiscitis.
Methods
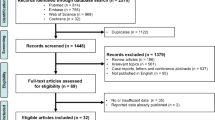
Clinical records of 260 patients with a suspicion of spondylodiscitis were analysed. Patients were selected using the following inclusion criteria: confirmed diagnosis of spondylodiscitis either from pyogenic bacteria or from Mycobacterium tuberculosis and contrast-enhanced MRI performed before treatment. Clinical data concerning age, sex and country-of-origin were also collected. For each patient, several MRI-features were evaluated by two-expert musculoskeletal radiologists. A chi-squared test and a multiple logistic regression were used to find the best predictors of tuberculous or pyogenic spondylodiscitis.
Results
114 patients were retrospectively enrolled, 30 with tuberculous and 84 with pyogenic spondylodiscitis. We found 18 MRI-features, significantly different between the two groups. Among these, the most strongly associated with tuberculous spondylodiscitis were: heterogeneous vertebral signal on T1w-sequences (Odds Ratio(OR) = 205.759-p < 0.001), presence of epidural abscess (OR = 86.221-p < 0.001), severe vertebral destruction (OR = 10.017-p < 0.001) and absence of epidural phlegmon (OR = 86.221-p < 0.001). Moreover, patients coming from countries with a middle-high prevalence of tuberculosis were more frequently affected by tuberculous spondylodiscitis than others were (OR = 229.136-p < 0.001). The best prediction model demonstrated a correct classification rate of 94.7%.
Conclusion
To the best of our knowledge this is the largest study comparing MRI-features of tuberculous and pyogenic spondylodiscitis. The above-mentioned MRI-features and epidemiological data are crucial in the differential diagnosis between these two entities, guiding the choice of the appropriate therapy, especially when a pathogen cannot be clearly identified with other modalities.



Similar content being viewed by others
References
Dziurzyńska-Białek E, Kruk-Bachonko J, Guz W, Łosicki M, Krupski W (2012) Diagnostic difficulties resulting from morphological image variation in spondylodiscitis MR imaging. Pol J Radiol 77(3):25
Gouliouris T, Aliyu SH, Brown NM. (2010). Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother, 65(suppl_3), iii11-iii24.
Zhang N, Zeng X, He L, Liu Z, Liu J, Zhang Z et al (2019) The Value of MR Imaging in Comparative Analysis of Spinal Infection in Adults: Pyogenic Versus Tuberculous. World neurosurgery 128:e806–e813
Doutchi M, Seng P, Menard A, Meddeb L, Adetchessi T, Fuentes S et al (2015) Changing trends in the epidemiology of vertebral osteomyelitis in Marseille, France. New microbes and new infections 7:1–7
Sato K, Yamada K, Yokosuka K, Yoshida T, Goto M, Matsubara T, et al. (2019). Pyogenic Spondylitis: Clinical Features, Diagnosis and Treatment. The Kurume medical journal, MS653001.
Skaf GS, Domloj NT, Fehlings MG, Bouclaous CH, Sabbagh AS, Kanafani ZA, Kanj SS (2010) Pyogenic spondylodiscitis: an overview. J Infect Public Health 3(1):5–16
Frel M, Białecki J, Wieczorek J, Paluch Ł, Dąbrowska-Thing A, Walecki J (2017) Magnetic resonance imaging in differentatial diagnosis of pyogenic spondylodiscitis and tuberculous spondylodiscitis. Pol J Radiol 82:71
Kumar Y, Gupta N, Chhabra A, Fukuda T, Soni N, Hayashi D (2017) Magnetic resonance imaging of bacterial and tuberculous spondylodiscitis with associated complications and non-infectious spinal pathology mimicking infections: a pictorial review. BMC Musculoskelet Disord 18(1):244
Chang MC, Wu HTH, Lee CH, Liu CL, Chen TH (2006) Tuberculous spondylitis and pyogenic spondylitis: comparative magnetic resonance imaging features. Spine 31(7):782–788
Souza CGD, Gasparetto EL, Marchiori E, Bahia PRV (2013) Pyogenic and tuberculous discitis: magnetic resonance imaging findings for differential diagnosis. Radiol Bras 46(3):173–177
Lee KY (2014) Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian spine journal 8(2):216
Mavrogenis AF, Megaloikonomos PD, Igoumenou VG, Panagopoulos GN, Giannitsioti E, Papadopoulos A, Papagelopoulos PJ (2017) Spondylodiscitis revisited EFORT open reviews 2(11):447–461
Harada Y, Tokuda O, Matsunaga N. (2008). Magnetic resonance imaging characteristics of tuberculous spondylitis vs. pyogenic spondylitis. Clinical imaging, 32(4), 303–309.
Li T, Li W, Du Y, Gao M, Liu X, Wang G, et al. (2018). Discrimination of pyogenic spondylitis from brucellar spondylitis on MRI. Medicine, 97(26).
Park JH, Shin HS, Park JT, Kim TY, Eom KS (2011) Differentiation between tuberculous spondylitis and pyogenic spondylitis on MR imaging. Korean Journal of Spine 8(4):283
Garg RK, Somvanshi DS (2011) Spinal tuberculosis: a review. J Spinal Cord Med 34(5):440–454
Rivas-Garcia A, Sarria-Estrada S, Torrents-Odin C, Casas-Gomila L, Franquet E (2013) Imaging findings of Pott’s disease. Eur Spine J 22(4):567–578
Berbari EF, Kanj SS, Kowalski TJ, Darouiche RO, Widmer AF, Schmitt SK et al (2015) 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adultsa. Clin Infect Dis 61(6):e26–e46
Jung NY, Jee WH, Ha KY, Park CK, Byun JY (2004) Discrimination of tuberculous spondylitis from pyogenic spondylitis on MRI. Am J Roentgenol 182(6):1405–1410
Spira D, Germann T, Lehner B, Hemmer S, Akbar M, Jesser J, et al. (2016). CT-guided biopsy in suspected spondylodiscitis–the association of paravertebral inflammation with microbial pathogen detection. PloS one, 11(1), e0146399.
Sertic M, Parkes L, Mattiassi S, Pritzker K, Gardam M, Murphy K (2019) The efficacy of computed tomography-guided percutaneous spine biopsies in determining a causative organism in cases of suspected infection: a systematic review. Can Assoc Radiol J 70(1):96–103
Ahuja N, Sharma H (2017) The effectiveness of computed tomography-guided biopsy for the diagnosis of spondylodiscitis: an analysis of variables affecting the outcome. Eur Rev Med Pharmacol Sci 21(9):2021–2026
Kim CJ, Kim EJ, Song KH, Choe PG, Park WB, Bang JH et al (2016) Comparison of characteristics of culture-negative pyogenic spondylitis and tuberculous spondylitis: a retrospective study. BMC Infect Dis 16(1):1–5
Lönnroth K, Migliori GB, Abubakar I, D’Ambrosio L, De Vries G, Diel R et al (2015) Towards tuberculosis elimination: an action framework for low-incidence countries. Eur Respir J 45(4):928–952
World Health Organization. Global tuberculosis report 2019: World Health Organization; 2019.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Naselli, N., Facchini, G., Lima, G.M. et al. MRI in differential diagnosis between tuberculous and pyogenic spondylodiscitis. Eur Spine J 31, 431–441 (2022). https://doi.org/10.1007/s00586-021-06952-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06952-8