Abstract
Purpose
Pelvic incidence (PI) is unique to each individual and does not change throughout life. High PI is related to lumbar spondylolisthesis, but associations of PI with lumbar osteophyte formation and disc degeneration are unclear. The objective was to evaluate relationships of PI with lumbar osteophyte formation and disc degeneration, as well as spinal sagittal alignment and geriatric diseases, in middle-aged and elderly people.
Methods
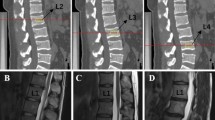
A total of 1002 volunteers (male: 434, female: 568, average age: 63.5) were prospectively examined for lumbar osteophyte formation (Nathan class ≥ 2) and disc degeneration (disc score ≥ 3). High (PI > 51, n = 501) and low (PI ≤ 51, n = 501) PI groups were defined. Clinical factors, frailty, sarcopenia, and physical quality of life (QOL) were compared between these groups, and risk factors for lumbar osteophyte formation and disc degeneration were identified in multivariate logistic regression analysis.
Results
Physical QOL was poorer in people with lumbar osteophyte formation (54.8%) and disc degeneration (33.6%). Age, male gender, spinal parameters including PI, bone mineral density, back muscle strength, and gait ability differed significantly between the groups, whereas frailty and sarcopenia were not significantly different. Low PI, low lumbar lordosis, elder age, male gender, high BMI, and weak back muscle strength were significant risk factors for lumbar osteophyte formation and disc degeneration.
Conclusions
Low PI was identified as a risk factor for lumbar osteophyte formation and disc degeneration, both of which reduce physical QOL in middle-aged and elderly people.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.



Similar content being viewed by others
References
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis research society-schwab adult spinal deformity classification: a validation study. Spine 37:1077–1082. https://doi.org/10.1097/brs.0b013e31823e15e2
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstuck F, Perez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A, European Spine Study G (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99:1661–1672. https://doi.org/10.2106/JBJS.16.01594
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V, International Spine Study G (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine 38:E803–E812. https://doi.org/10.1097/brs.0b013e318292b7b9
Miyakoshi N, Hongo M, Maekawa S, Ishikawa Y, Shimada Y, Itoi E (2007) Back extensor strength and lumbar spinal mobility are predictors of quality of life in patients with postmenopausal osteoporosis. Osteoporos Int 18:1397–1403. https://doi.org/10.1007/s00198-007-0383-3
Imagama S, Hasegawa Y, Matsuyama Y, Sakai Y, Ito Z, Hamajima N, Ishiguro N (2011) Influence of sagittal balance and physical ability associated with exercise on quality of life in middle-aged and elderly people. Arch Osteoporos 6:13–20
Imagama S, Matsuyama Y, Hasegawa Y, Sakai Y, Ito Z, Ishiguro N, Hamajima N (2011) Back muscle strength and spinal mobility are predictors of quality of life in middle-aged and elderly males. Eur Spine J 20:954–961
Imagama S, Ando K, Kobayashi K, Seki T, Hamada T, Machino M, Ota K, Tanaka S, Morozumi M, Kanbara S, Ito S, Ishiguro N, Hasegawa Y (2019) Impact of comorbidity rates of lumbar spondylosis, knee osteoarthritis, and osteoporosis on physical QOL and risk factors for poor physical QOL in middle-aged and elderly people. Mod Rheumatol. https://doi.org/10.1080/14397595.2019.1601839
Kasai T, Hasegawa Y, Imagama S, Sakai T, Wakai K, Suzuki K, Ishiguro N (2017) The impact of musculoskeletal diseases on mortality-comparison with internal diseases: a 15-year longitudinal study. J Orthop Sci 22:1126–1131. https://doi.org/10.1016/j.jos.2017.06.014
Tsuboi M, Hasegawa Y, Matsuyama Y, Suzuki S, Suzuki K, Imagama S (2011) Do musculoskeletal degenerative diseases affect mortality and cause of death after 10 years in Japan? J Bone Miner Metab 29:217–223. https://doi.org/10.1007/s00774-010-0214-z
Berven S, Wadhwa R (2018) Sagittal alignment of the lumbar spine. Neurosurg Clin N Am 29:331–339. https://doi.org/10.1016/j.nec.2018.03.009
Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Chopin D, Hresko T, Dimnet J (2004) Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine 29:2049–2054
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16:1459–1467. https://doi.org/10.1007/s00586-006-0294-6
Imagama S, Hasegawa Y, Ando K, Kobayashi K, Hida T, Ito K, Tsushima M, Nishida Y, Ishiguro N (2017) Staged decrease of physical ability on the locomotive syndrome risk test is related to neuropathic pain, nociceptive pain, shoulder complaints, and quality of life in middle-aged and elderly people—the utility of the locomotive syndrome risk test. Mod Rheumatol 27:1051–1056. https://doi.org/10.1080/14397595.2017.1285856
Kobayashi K, Ando K, Tsushima M, Machino M, Ota K, Morozumi M, Tanaka S, Kanbara S, Ishiguro N, Hasegawa Y, Imagama S (2018) Predictors of locomotive syndrome in community-living people: a prospective five-year longitudinal study. Mod Rheumatol. https://doi.org/10.1080/14397595.2018.1514705
Imagama S, Ando K, Kobayashi K, Seki T, Hamada T, Machino M, Ota K, Tanaka S, Morozumi M, Kanbara S, Ito S, Ishiguro N, Hasegawa Y (2019) Shoulder pain has most impact on poor quality of life among various types of musculoskeletal pain in middle-aged and elderly people: Yakumo study. Mod Rheumatol. https://doi.org/10.1080/14397595.2019.1623364
Imagama S, Hasegawa Y, Wakao N, Hirano K, Muramoto A, Ishiguro N (2014) Impact of spinal alignment and back muscle strength on shoulder range of motion in middle-aged and elderly people in a prospective cohort study. Eur Spine J 23:1414–1419. https://doi.org/10.1007/s00586-014-3251-9
Jackson RP, Kanemura T, Kawakami N, Hales C (2000) Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine 25:575–586
Jackson RP, Peterson MD, McManus AC, Hales C (1998) Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine 23:1750–1767
Imagama S, Hasegawa Y, Wakao N, Hirano K, Hamajima N, Ishiguro N (2012) Influence of lumbar kyphosis and back muscle strength on the symptoms of gastroesophageal reflux disease in middle-aged and elderly people. Eur Spine J 21:2149–2157
Imagama S, Ito Z, Wakao N, Seki T, Hirano K, Muramoto A, Sakai Y, Matsuyama Y, Hamajima N, Ishiguro N (2013) Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J 22:1346–1353
Nathan H (1962) Osteophytes of the vertebral column—an anatomical study of their development according to age, race, and sex with considerations as to their etiology and significance. J Bone Joint Surg Am 44:243–268. https://doi.org/10.2106/00004623-196244020-00003
Imagama S, Hasegawa Y, Seki T, Matsuyama Y, Sakai Y, Ito Z, Ishiguro N, Ito Y, Hamajima N, Suzuki K (2011) The effect of beta-carotene on lumbar osteophyte formation. Spine 36:2293–2298. https://doi.org/10.1097/brs.0b013e3182254a18
Miyakoshi N, Itoi E, Murai H, Wakabayashi I, Ito H, Minato T (2003) Inverse relation between osteoporosis and spondylosis in postmenopausal women as evaluated by bone mineral density and semiquantitative scoring of spinal degeneration. Spine 28:492–495. https://doi.org/10.1097/01.brs.0000048650.39042.58
Miyakoshi N, Abe E, Shimada Y, Hongo M, Chiba M, Sato K (1999) Anterior decompression with single segmental spinal interbody fusion for lumbar burst fracture. Spine 24:67–73. https://doi.org/10.1097/00007632-199901010-00016
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research G (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156
Satake S, Shimada H, Yamada M, Kim H, Yoshida H, Gondo Y, Matsubayashi K, Matsushita E, Kuzuya M, Kozaki K, Sugimoto K, Senda K, Sakuma M, Endo N, Arai H (2017) Prevalence of frailty among community-dwellers and outpatients in Japan as defined by the Japanese version of the cardiovascular health study criteria. Geriatr Gerontol Int 17:2629–2634. https://doi.org/10.1111/ggi.13129
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JS, Lee WJ, Lee Y, Liang CK, Limpawattana P, Lin CS, Peng LN, Satake S, Suzuki T, Won CW, Wu CH, Wu SN, Zhang T, Zeng P, Akishita M, Arai H (2014) Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc 15:95–101. https://doi.org/10.1016/j.jamda.2013.11.025
Hida T, Imagama S, Ando K, Kobayashi K, Muramoto A, Ito K, Ishikawa Y, Tsushima M, Nishida Y, Ishiguro N, Hasegawa Y (2018) Sarcopenia and physical function are associated with inflammation and arteriosclerosis in community-dwelling people: the Yakumo study. Mod Rheumatol 28:345–350. https://doi.org/10.1080/14397595.2017.1349058
Hida T, Ando K, Kobayashi K, Ito K, Tsushima M, Kobayakawa T, Morozumi M, Tanaka S, Machino M, Ota K, Kanbara S, Ito S, Ishiguro N, Hasegawa Y, Imagama S (2018) Editors’ choice ultrasound measurement of thigh muscle thickness for assessment of sarcopenia. Nagoya J Med Sci 80:519–527. https://doi.org/10.18999/nagjms.80.4.519
Tanimoto Y, Watanabe M, Sun W, Hirota C, Sugiura Y, Kono R, Saito M, Kono K (2012) Association between muscle mass and disability in performing instrumental activities of daily living (IADL) in community-dwelling elderly in Japan. Arch Gerontol Geriatr 54:e230–e233. https://doi.org/10.1016/j.archger.2011.06.015
Hasegawa K, Okamoto M, Hatsushikano S, Shimoda H, Ono M, Watanabe K (2016) Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J 25:3675–3686. https://doi.org/10.1007/s00586-016-4702-2
Yoshida G, Alzakri A, Pointillart V, Boissiere L, Obeid I, Matsuyama Y, Vital JM, Gille O (2018) Global spinal alignment in patients with cervical spondylotic myelopathy. Spine 43:E154–E162. https://doi.org/10.1097/brs.0000000000002253
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30:346–353
Cacciola G, Pisani A, Cavaliere P, Pitrone B, Rizzo D, Rizzo G, Cascio F, Meo F, Barbanera A (2018) High values of pelvic incidence: a possible risk factor for zigoapophyseal facet arthrosis in young. J Orthop 15:333–336. https://doi.org/10.1016/j.jor.2018.02.011
Lv X, Liu Y, Zhou S, Wang Q, Gu H, Fu X, Ding Y, Zhang B, Dai M (2016) Correlations between the feature of sagittal spinopelvic alignment and facet joint degeneration: a retrospective study. BMC Musculoskelet Disord 17:341. https://doi.org/10.1186/s12891-016-1193-6
Jentzsch T, Geiger J, Konig MA, Werner CM (2017) Hyperlordosis is associated with facet joint pathology at the lower lumbar spine. Clin Spine Surg 30:129–135. https://doi.org/10.1097/BSD.0b013e3182aab266
Jang HJ, Hughes LC, Oh DW, Kim SY (2017) Effects of corrective exercise for thoracic hyperkyphosis on posture, balance, and well-being in older women: a double-blind, group-matched design. J Geriatr Phys Ther. https://doi.org/10.1519/jpt.0000000000000146
Kadono N, Tsuchiya K, Uematsu A, Kamoshita H, Kiryu K, Hortobagyi T, Suzuki S (2017) A Japanese stretching intervention can modify lumbar lordosis curvature. Clin Spine Surg 30:297–300. https://doi.org/10.1097/BSD.0000000000000247
Zaina F, Atanasio S, Ferraro C, Fusco C, Negrini A, Romano M, Negrini S (2009) Review of rehabilitation and orthopedic conservative approach to sagittal plane diseases during growth: hyperkyphosis, junctional kyphosis, and Scheuermann disease. Eur J Phys Rehabil Med 45:595–603
Jalai CM, Diebo BG, Cruz DL, Poorman GW, Vira S, Buckland AJ, Lafage R, Bess S, Errico TJ, Lafage V, Passias PG (2017) The impact of obesity on compensatory mechanisms in response to progressive sagittal malalignment. Spine J 17:681–688. https://doi.org/10.1016/j.spinee.2016.11.016
Araujo F, Lucas R, Alegrete N, Azevedo A, Barros H (2014) Individual and contextual characteristics as determinants of sagittal standing posture: a population-based study of adults. Spine J 14:2373–2383. https://doi.org/10.1016/j.spinee.2014.01.040
Hongo M, Itoi E, Sinaki M, Miyakoshi N, Shimada Y, Maekawa S, Okada K, Mizutani Y (2007) Effect of low-intensity back exercise on quality of life and back extensor strength in patients with osteoporosis: a randomized controlled trial. Osteoporos Int 18:1389–1395. https://doi.org/10.1007/s00198-007-0398-9
Song H, Luo Y, Wang W, Li S, Yang K, Dai M, Shen Y, Zhang Y, Zhang L (2017) Effects of alendronate on lumbar intervertebral disc degeneration with bone loss in ovariectomized rats. Spine J 17:995–1003. https://doi.org/10.1016/j.spinee.2017.03.002
Xiao ZF, He JB, Su GY, Chen MH, Hou Y, Chen SD, Lin DK (2018) Osteoporosis of the vertebra and osteochondral remodeling of the endplate causes intervertebral disc degeneration in ovariectomized mice. Arthr Res Ther 20:207. https://doi.org/10.1186/s13075-018-1701-1
Liu Q, Wang X, Hua Y, Kong G, Wu X, Huang Z, Huang Z, Liu J, Yang Z, Zhu Q (2018) Estrogen deficiency exacerbates intervertebral disc degeneration induced by spinal instability in rats. Spine. https://doi.org/10.1097/brs.0000000000002904
Acknowledgements
We are grateful to the staff of the Comprehensive Health Care Programme held in Yakumo, Hokkaido; to Mr. Masato Kako and Ms. Azusa Kayamoto in the Department of Rehabilitation, Nagoya University Hospital; to Ms. Aya Hemmi and Ms. Hiroko Ino at Nagoya University; and to all the staff of the central clerk desk in Nagoya University Hospital for their assistance throughout this study.
Funding
This study was supported by Japanese Ministry of Health, Labour, and Welfare Grants-in-Aid for Scientific Research (C) (18K09102). No other funds were received in support of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest except for this national Grant.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Imagama, S., Ando, K., Kobayashi, K. et al. Impact of pelvic incidence on lumbar osteophyte formation and disc degeneration in middle-aged and elderly people in a prospective cross-sectional cohort. Eur Spine J 29, 2262–2271 (2020). https://doi.org/10.1007/s00586-019-06204-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06204-w