Abstract
Purpose
Mitochondrial diseases are a heterogeneous group of disorders. Patients with such diseases often need general anesthesia for diagnostic procedures and surgery; guidelines are lacking for the anesthetic care of these patients.
Methods
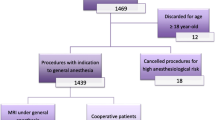
We conducted a survey to investigate the current practices of pediatric anesthesiologists in the US in order to determine and document current practice. The survey consisted of twenty questions, including two demographic questions. A link to the survey was sent via email to members of the Society for Pediatric Anesthesia (2440), and was available online for 14 weeks.
Results
Only 503 completed the survey: a response rate of 20.61 %. Among the responders, 93.2 % had children with mitochondrial disorders among their patients, but only 11 % had institutional guidelines for such cases in place. Among the responders, 80.3 % used the standard nil per os (NPO) status guidelines, while the rest give intravenous dextrose solution once NPO was in effect. Only 18.3 % took precautions for malignant hyperthermia during treatment. The majority of the practitioners chose sevoflurane as the safest inhaled agent for induction and maintenance (89.7 and 78.5 %, respectively). Regional anesthesia was deemed safe by 97.3 % of the responders. Lactated Ringer’s solution was considered safe for these children by 49 %; only 47.8 % used dextrose-containing fluids for fluid replacement. The blood glucose was monitored by 72.7 %, and the majority (85 %) of this monitoring was done in a postanesthesia care unit.
Conclusion
Although the response rate was low, the majority of the responders provide care to these children routinely, so it can be inferred that the results of this survey are the closest published results to the true trend.
Similar content being viewed by others
References
Blm M. Current management in child neurology. 4th ed. Shelton: People’s Medical Publishing House; 2008.
Thorburn DR, Smeitink J. Diagnosis of mitochondrial disorders: clinical and biochemical approach. J Inherit Metab Dis. 2001;24:312–6.
Bernier FP, Boneh A, Dennett X, Chow CW, Cleary MA, Thorburn DR. Diagnostic criteria for respiratory chain disorders in adults and children. Neurology. 2002;59:1406–11.
Footitt EJ, Sinha MD, Raiman JA, Dhawan A, Moganasundram S, Champion MP. Mitochondrial disorders and general anaesthesia: a case series and review. Br J Anaesth. 2008;100:436–41.
Driessen J, Willems S, Dercksen S, Giele J, van der Staak F, Smeitink J. Anesthesia-related morbidity and mortality after surgery for muscle biopsy in children with mitochondrial defects. Paediatr Anaesth. 2007;17:16–21.
Rosaeg OP, Morrison S, MacLeod JP. Anaesthetic management of labour and delivery in the parturient with mitochondrial myopathy. Can J Anaesth. 1996;43:403–7.
Hsiao PN, Cheng YJ, Tseng HC, Chuang YH, Kao PF, Tsai SK. Spinal anesthesia in MELAS syndrome: a case with mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes. Acta Anaesthesiol Sin. 2000;38:107–10.
Lauwers MH, Van Lersberghe C, Camu F. Inhalation anaesthesia and the Kearns–Sayre syndrome. Anaesthesia. 1994;49:876–8.
Miller RD. Miller’s anesthesia. 7th ed. Philadelphia: Churchill Livingstone; 2009.
Fleisher LA. Anesthesia and uncommon diseases. 5th ed. Philadelphia: Elsevier; 2005.
Hanley PJ, Ray J, Brandt U, Daut J. Halothane, isoflurane and sevoflurane inhibit NADH:ubiquinone oxidoreductase (complex I) of cardiac mitochondria. J Physiol. 2002;544:687–93.
Bains R, Moe MC, Vinje ML, Berg-Johnsen J. Sevoflurane and propofol depolarize mitochondria in rat and human cerebrocortical synaptosomes by different mechanisms. Acta Anaesthesiol Scand. 2009;53:1354–60.
Morgan PG, Hoppel CL, Sedensky MM. Mitochondrial defects and anesthetic sensitivity. Anesthesiology. 2002;96:1268–70.
Gurrieri C, Kivela JE, Bojanic K, Gavrilova RH, Flick RP, Sprung J, Weingarten TN. Anesthetic considerations in mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes syndrome: a case series. Can J Anaesth. 2011;58:751–63.
Cohen PJ. Effect of anesthetics on mitochondrial function. Anesthesiology. 1973;39:153–64.
Koruk S, Mizrak A, Kaya Ugur B, Ilhan O, Baspinar O, Oner U. Propofol/dexmedetomidine and propofol/ketamine combinations for anesthesia in pediatric patients undergoing transcatheter atrial septal defect closure: a prospective randomized study. Clin Ther. 2010;32:701–9.
Segal IS, Vickery RG, Walton JK, Doze VA, Maze M. Dexmedetomidine diminishes halothane anesthetic requirements in rats through a postsynaptic alpha 2 adrenergic receptor. Anesthesiology. 1988;69:818–23.
Shukry M, Kennedy K. Dexmedetomidine as a total intravenous anesthetic in infants. Paediatr Anaesth. 2007;17:581–3.
Engelhard K, Werner C, Kaspar S, Mollenberg O, Blobner M, Bachl M, Kochs E. Effect of the alpha2-agonist dexmedetomidine on cerebral neurotransmitter concentrations during cerebral ischemia in rats. Anesthesiology. 2002;96:450–7.
Wong J, Steil GM, Curtis M, Papas A, Zurakowski D, Mason KP. Cardiovascular effects of dexmedetomidine sedation in children. Anesth Analg. 2012;114:193–9.
Mastronicola D, Arcuri E, Arese M, Bacchi A, Mercadante S, Cardelli P, Citro G, Sarti P. Morphine but not fentanyl and methadone affects mitochondrial membrane potential by inducing nitric oxide release in glioma cells. Cell Mol Life Sci. 2004;61:2991–7.
Finsterer J, Stratil U, Bittner R, Sporn P. Increased sensitivity to rocuronium and atracurium in mitochondrial myopathy. Can J Anaesth. 1998;45:781–4.
D’Ambra MN, Dedrick D, Savarese JJ. Kearns–Sayer syndrome and pancuronium–succinylcholine-induced neuromuscular blockade. Anesthesiology. 1979;51:343–5.
Wiesel S, Bevan JC, Samuel J, Donati F. Vecuronium neuromuscular blockade in a child with mitochondrial myopathy. Anesth Analg. 1991;72:696–9.
Rowe RW, Helander E. Anesthetic management of a patient with systemic carnitine deficiency. Anesth Analg. 1990;71:295–7.
Stickler DE, Valenstein E, Neiberger RE, Perkins LA, Carney PR, Shuster JJ, Theriaque DW, Stacpoole PW. Peripheral neuropathy in genetic mitochondrial diseases. Pediatr Neurol. 2006;34:127–31.
Muravchick S. Clinical implications of mitochondrial disease. Adv Drug Deliv Rev. 2008;60:1553–60.
Fernandes J. Inborn metabolic diseases: diagnosis and treatment. 4th ed. Heidelberg: Springer; 2006.
Paut O, Lacroix F. Recent developments in the perioperative fluid management for the paediatric patient. Curr Opin Anaesthesiol. 2006;19:268–77.
Hirshberg E, Larsen G, Van Duker H. Alterations in glucose homeostasis in the pediatric intensive care unit: hyperglycemia and glucose variability are associated with increased mortality and morbidity. Pediatr Crit Care Med. 2008;9:361–6.
Delogu G, Antonucci A, Moretti S, Marandola M, Tellan G, Signore M, Famularo G. Oxidative stress and mitochondrial glutathione in human lymphocytes exposed to clinically relevant anesthetic drug concentrations. J Clin Anesth. 2004;16:189–94.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Rafique, M.B., Cameron, S.D., Khan, Q. et al. Anesthesia for children with mitochondrial disorders: a national survey and review. J Anesth 27, 186–191 (2013). https://doi.org/10.1007/s00540-012-1488-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-012-1488-1