Abstract
Purpose
The purpose of this study was to evaluate the usefulness of Trachlight (TL) for nasotracheal intubation and to determine the relationship between the grade of laryngeal view and the subsequent ease of nasotracheal intubation using TL.
Methods
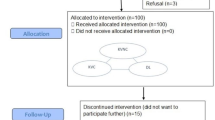
Patients requiring nasotracheal intubation were enrolled in this study. Laryngoscopy was performed in all patients under topical anesthesia, with 8% lidocaine spray applied to the supraglottic region and the vocal cords. Glottic visualization during laryngoscopy was assessed using the Cormack and Lehane classification. Patients were allocated to four groups according to this classification. If the TL intubation was unsuccessful after three attempts, intubation was carried out using direct laryngoscopy. Intubation difficulty was assessed by the original 6-point scale and the total intubation time was also recorded.
Results
Trachlight intubation was successful in 89.1% of the 110 patients enrolled in the study. There was no observed correlation between the original 6-point scale and glottic visualization. The total intubation time and the ratio of “unsuccessful” cases were not significantly different among the four groups.
Conclusion
No relationship was found between the ease of nasotracheal intubation using TL and glottic visualization.
Similar content being viewed by others
References
Hung OR, Pytka S, Morris I, Murphy M, Stewart RD. Lightwand intubation: II. Clinical trial of a new lightwand for tracheal intubation in patients with difficult airway. Can J Anaesth. 1995;42:826–30.
Weis FR, Hatton MN. Intubation by use of the light wand: experience in 253 patients. J Oral Maxillofac Surg. 1989;47:577–80.
Roberto F, Paolo T, Francesco DL, Donato C, Giancarla E, Sabrina Q, Alassandro G. Effective nasotracheal intubation using a modified transillumination technique. Can J Anesth. 2002;49:91–5.
Friedman PG, Rosenberg MK, Lebenbom-Mansour M. A comparison of lightwand and suspension Laryngoscopic intubation techniques in outpatients. Anesth Analg. 1997;85:578–82.
Hung OR, Pytka S, Morris I, Murphy M, Launcelott G, Stevens S, MacKay W, Stewart RD. Clinical trial of a new lightwand device (Trachlight) to intubate the trachea. Anesthesiology. 1995;83:509–14.
Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11.
Ainsworth QP, Howells TH. Transilluminated tracheal intubation. Br J Anaesth. 1989;62:494–7.
Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, Liu PL. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc. 1985;32:429–34.
Kim YC, Lee SH, Noh GJ, Cho SY, Yeom JH, Shin WJ, Lee DH, Ryu JS, Park YS, Cha KJ, Lee SC. Thermosoftening treatment of the nasotracheal tube before intubation can reduce epistaxis and nasal damage. Anesth Analg. 2000;91:698–701.
Elstraete ACV, Pennant JH, Gajraj NM, Victory RA. Tracheal tube cuff inflation as an aid to blind nasotracheal intubation. Br J Anaesth. 1993;70:691–3.
Yamamura H, Yamamoto T, Kamiyama M. Device for blind nasal intubation. Anesthesiology. 1959;20:221.
Inoue Y, Koga K, Shigematsu A. A comparison of two tracheal intubation techniques with Trachlight™ in patients with cervical spine disorders. Anesth Analg. 2002;94:667–71.
Fox DJ, Castro T, Rastrelli AJ. Comparison of intubation techniques in the awake patient: the Flexi-lum surgical light (lightwand) versus blind nasal approach. Anesthesiology. 1987;66:69–71.
Locker GJ, Staudinger T, Knapp S, Burgmann H, Laczika KF, Zimmerl M, Hormann M, Frass MRM. Assessment of the proper depth of endotracheal tube placement with Trachlight. J Clin Anesth. 1998;10:389–93.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Manabe, Y., Seto, M., Iwamoto, S. et al. The success rate of nasotracheal intubation using lightwand does not depend on the laryngoscopic view. J Anesth 25, 350–355 (2011). https://doi.org/10.1007/s00540-011-1117-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1117-4