Abstract
Background
Achalasia is a well-known esophageal motility disorder, but epidemiological studies in Japan are lacking. We investigated the incidence and period prevalence of achalasia in Japan, including the rate of coexistence of esophageal carcinoma, and evaluated treatment trends.
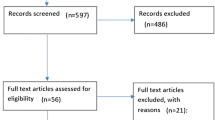
Methods
To estimate the nationwide number of patients with achalasia, a large-scale insurance claims database from 2005 to 2017 were used for our analyses. Patients with achalasia and coexistence of esophageal carcinoma were identified based on the diagnosis code registered. Interventional treatment was also evaluated.
Results
Of the total 5,493,650 populations, 385 were diagnosed with primary achalasia. The incidence was calculated as 0.81–1.37 per 100,000 person-years (male-to-female ratio was almost 1; mean age at diagnosis was 43.3 ± 14.4 years). The period prevalence was 7.0 per 100,000 persons. There were statistically significant trends of increase in the incidence and period prevalence over age groups (all p values < 0.0001). Four men with achalasia developed esophageal carcinoma, and the incidence of esophageal carcinoma with achalasia was estimated as 0.25 per 100 person-years. With regard to intervention, esophageal dilation was performed as a first treatment in 64.7% of patients, with repeat intervention required in 56.9% of these. The proportion of patients treated using peroral endoscopic myotomy (POEM) increased annually to 41.1% in 2017.
Conclusions
In Japan, the incidence and period prevalence of achalasia is comparable to that in other countries. The absolute risk of esophageal carcinoma is rather low. Esophageal dilation has been the mainstay of achalasia treatment, and the role of POEM has increased annually.



Similar content being viewed by others
References
Richter JE. Oesophageal motility disorders. Lancet. 2001;358:823–8.
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383(9911):83–93.
Goldblum JR, Whyte RI, Orringer MB, et al. Achalasia. A morphologic study of 42 resected specimens. Am J Surg Pathol. 1994;18:327–37.
Nakajima N, Sato H, Takahashi K, et al. Muscle layer histopathology and manometry pattern of primary esophageal motility disorders including achalasia. Neurogastroenterol Motil. 2017;29:e12968.
Sato H, Takahashi K, Mizuno KI, et al. A clinical study of peroral endoscopic myotomy reveals that impaired lower esophageal sphincter relaxation in achalasia is not only defined by high-resolution manometry. PLoS One. 2018;13:e0195423.
Csendes A, Smok G, Braghetto I, et al. Histological studies of Auerbach’s plexuses of the oesophagus, stomach, jejunum, and colon in patients with achalasia of the oesophagus: correlation with gastric acid secretion, presence of parietal cells and gastric emptying of solids. Gut. 1992;33:150–4.
Eckardt AJ, Eckardt VF. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastro Hepat. 2011;8:311–9.
Clark SB, Rice TW, Tubbs RR, et al. The nature of the myenteric infiltrate in achalasia: an immunohistochemical analysis. Am J Surg Pathol. 2000;24:1153–8.
Sato H, Takahashi K, Mizuno KI, et al. Esophageal motility disorders: new perspectives from high-resolution manometry and histopathology. J Gastroenterol. 2018;53:484–93.
Gockel HR, Schumacher J, Gockel I, et al. Achalasia: will genetic studies provide insights? Hum Genet. 2010;128:353–64.
Raymond L, Lach B, Shamji FM. Inflammatory aetiology of primary oesophageal achalasia: an immunohistochemical and ultrastructural study of Auerbach’s plexus. Histopathology. 1999;35:445–53.
Ghoshal UC, Daschakraborty SB, Singh R. Pathogenesis of achalasia cardia. World J Gastroenterol. 2012;18:3050–7.
Gockel I, Becker J, Wouters MM, et al. Common variants in the HLA-DQ region confer susceptibility to idiopathic achalasia. Nat Genet. 2014;46:901–4.
Samo S, Carlson DA, Gregory DL, et al. Incidence and prevalence of achalasia in Central Chicago, 2004–2014, since the widespread use of high-resolution manometry. Clin Gastroenterol Hepatol. 2017;15:366–73.
Duffield JA, Hamer PW, Heddle R, et al. Incidence of achalasia in South Australia based on esophageal manometry findings. Clin Gastroenterol Hepatol. 2017;15:360–5.
van Hoeij FB, Ponds FA, Smout AJ, et al. Incidence and costs of achalasia in The Netherlands. Neurogastroenterol Motil. 2018;30:e13195.
Wadhwa V, Thota PN, Parikh MP, et al. Changing trends in age, gender, racial distribution and inpatient burden of achalasia. Gastroenterol Res. 2017;10:70–7.
O’Neill OM, Johnston BT, Coleman HG. Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2013;19:5806–12.
Dunaway PM, Wong RK. Risk and surveillance intervals for squamous cell carcinoma in achalasia. Gastrointest Endosc Clin N Am. 2001;11(425–34):ix.
Sato H, Takahashi K, Nakajima N, et al. Full-layer mucosal histology in achalasia: Histological epithelial wave is characteristic in “pinstripe pattern”-positive achalasia. Neurogastroenterol Motil. 2018;30:e13168.
Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–16.
Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–71.
Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg. 2015;221:256–64.
Herrinton LJ, Liu L, Lafata JE, et al. Estimation of the period prevalence of inflammatory bowel disease among nine health plans using computerized diagnoses and outpatient pharmacy dispensings. Inflamm Bowel Dis. 2007;13:451–61.
Howard PJ, Maher L, Pryde A, et al. Five year prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh. Gut. 1992;33:1011–5.
Leeuwenburgh I, Scholten P, Alderliesten J, et al. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol. 2010;105:2144–9.
National cancer center, Japan. Center for cancer control and information services. https://www.ncc.go.jp/en/cis/index.html.
Vaezi MF, Pandolfino JE, Vela MF. ACG Clinical Guideline: diagnosis and Management of Achalasia. Am J Gastroenterol. 2013;108:1238–49.
Zaninotto G, Bennett C, Boeckxstaens G, et al. The 2018 ISDE achalasia guidelines. Dis Esophagus. 2018;31.
Inoue H, Shiwaku H, Iwakiri K, et al. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc. 2018;30:563–79.
Tuason J, Inoue H. Current status of achalasia management: a review on diagnosis and treatment. J Gastroenterol. 2017;52:401–6.
Acknowledgements
This work was supported by JSPS KAKENHI Grant Number 18K15805.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Sato, H., Yokomichi, H., Takahashi, K. et al. Epidemiological analysis of achalasia in Japan using a large-scale claims database. J Gastroenterol 54, 621–627 (2019). https://doi.org/10.1007/s00535-018-01544-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-018-01544-8