Abstract
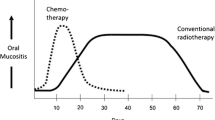
Neutropenic ulcerations are characterized by mucosal ulcerations which occur in the presence of neutropenia, suggesting a direct link between neutropenia and mucosal ulceration. An oral ulcer can be labeled as “neutropenic” only if the patients have primary (typically congenital) or secondary neutropenia, and neutropenia is the sole causative factor. Oral mucosal ulcers observed in patients undergoing oncologic therapy may also be termed as “neutropenic ulcers”, but the pathogenesis of these oral ulcers more likely involves mucosal events related to trauma, microbial factors, and direct cytotoxicity. In cancer patients, the early appearance of oral ulcers is often attributed to oral mucositis which is a condition primarily caused by the direct mucosal cytotoxicity of chemotherapeutic agents and radiation therapy. Oral ulcers that develop later during or after active cancer therapy may result from intraoral trauma and typically manifest on non-keratinized areas of the oral mucosa which are more susceptible to mucosal damage. In patients undergoing chemotherapy, factors such as disturbances in mucosal barrier function as well as bone marrow suppression lead to reduced neutrophil count and function, and can contribute to the development of oral ulcers. While the etiology of oral ulcers in cancer therapy receiving patients can vary, it is important to emphasize that the host’s response plays a crucial role in the progression and repair process of these lesions. This narrative review presents the etiopathogenesis, clinical presentation, and potential management approaches for oral ulcerations in neutropenic patients, with a particular focus on clarifying the usage of the term “neutropenic ulcer” since this term lacks diagnostic specificity and can be misleading in clinical practice regarding the underlying causes and treatment strategies.

Similar content being viewed by others
References
Frater JL (2020) How I investigate neutropenia. Int J Lab Hematol 42(Suppl 1):121–132. https://doi.org/10.1111/ijlh.13210
Copete MA, Sheridan DP (2000) Large granular lymphocyte leukemia and its association with oral neutropenic ulcerations: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90(4):474–477. https://doi.org/10.1067/moe.2000.107972
Feller L, Khammissa RA, Wood NH, Meyerov R, Pantanowitz L, Lemmer J (2012) Oral ulcers and necrotizing gingivitis in relation to HIV-associated neutropenia: a review and an illustrative case. AIDS Res Hum Retroviruses 28(4):346–351. https://doi.org/10.1089/AID.2011.0141
Newburger PE, Dale DC (2013) Evaluation and management of patients with isolated neutropenia. Semin Hematol 50(3):198–206. https://doi.org/10.1053/j.seminhematol.2013.06.010
Chaudhari PM, Mukkamalla SKR (2023) Autoimmune and chronic neutropenia. In: StatPearls. StatPearls Publishing, Treasure Island (FL)
Porter SR, Scully C, Standen GR (1994) Autoimmune neutropenia manifesting as recurrent oral ulceration. Oral Surg Oral Med Oral Pathol 78(2):178–180. https://doi.org/10.1016/0030-4220(94)90142-2
Tirali RE, Yalçınkaya Erdemci Z, Çehreli SB (2013) Oral findings and clinical implications of patients with congenital neutropenia: a literature review. Turk J Pediatr 55(3):241–245
Family L, Li Y, Chen LH, Page JH, Klippel ZK, Chao C (2018) A study of novel febrile neutropenia risk factors related to bone marrow or immune suppression, barrier function, and bacterial flora. J Natl Compr Canc Netw: JNCCN 16(10):1201–1208. https://doi.org/10.6004/jnccn.2018.7051
Skokowa J, Dale DC, Touw IP, Zeidler C, Welte K (2017) Severe congenital neutropenias. Nat Rev Dis Primers 3:17032. https://doi.org/10.1038/nrdp.2017.32
Cotomacio CC, Magliano GC, Alves FA, Simões A (2020) Local management of neutropenic ulcer in a patient under breast cancer treatment. Photodiagnosis Photodyn Ther 32:101997. https://doi.org/10.1016/j.pdpdt.2020.101997
Donadieu J, Beaupain B, Fenneteau O, Bellanné-Chantelot C (2017) Congenital neutropenia in the era of genomics: classification, diagnosis, and natural history. Br J Haematol 179(4):557–574. https://doi.org/10.1111/bjh.14887
Dale DC, Makaryan V (2002) ELANE-Related Neutropenia. In: Adam MP, Mirzaa GM, Pagon RA et al (eds) GeneReviews®. University of Washington, Seattle, Seattle (WA)
Connelly JA, Choi SW, Levine JE (2012) Hematopoietic stem cell transplantation for severe congenital neutropenia. Curr Opin Hematol 19(1):44–51. https://doi.org/10.1097/MOH.0b013e32834da96e
Lazzareschi I, Rossi E, Curatola A, Capozio G, Benacquista L, Iezzi L, Rigante D (2022) Assessment of congenital neutropenia in children: common clinical sceneries and clues for management. Mediterr J Hematol Infect Dis 14(1):e2022008. https://doi.org/10.4084/MJHID.2022.008
Donadieu J, Fenneteau O, Beaupain B, Mahlaoui N, Chantelot CB (2011) Congenital neutropenia: diagnosis, molecular bases and patient management. Orphanet J Rare Dis 6:26. https://doi.org/10.1186/1750-1172-6-26
Chen Y, Fang L, Yang X (2013) Cyclic neutropenia presenting as recurrent oral ulcers and periodontitis. J Clin Pediatr Dent 37(3):307–308. https://doi.org/10.17796/jcpd.37.3.n8k0111177074828
Beattie G, Whelan J, Cassidy J, Milne L, Burns S, Leonard R (1989) Herpes simplex virus, Candida albicans and mouth ulcers in neutropenic patients with non-haematological malignancy. Cancer Chemother Pharmacol 25(1):75–76. https://doi.org/10.1007/BF00694344
Luzzi GA, Jones BJ (1996) Treatment of neutropenic oral ulceration in human immunodeficiency virus infection with G-CSF. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 81(1):53–54. https://doi.org/10.1016/s1079-2104(96)80148-x
Field EA, Allan RB (2003) Review article: oral ulceration—aetiopathogenesis, clinical diagnosis and management in the gastrointestinal clinic. Aliment Pharmacol Ther 18(10):949–962. https://doi.org/10.1046/j.1365-2036.2003.01782.x
Laha B, Guha R, Hazra A (2012) Multiple cutaneous neutropenic ulcers associated with azathioprine. Indian J Pharm 44(5):646–648. https://doi.org/10.4103/0253-7613.100405
Moore DC (2016) Drug-induced neutropenia: a focus on rituximab-induced late-onset neutropenia. P & T 41(12):765–768
Andrès E, Mourot-Cottet R, Maloisel F, Séverac F, Keller O, Vogel T, Tebacher M, Weber JC, Kaltenbach G, Gottenberg JE, Goichot B, Sibilia J, Korganow AS, Herbrecht R (2017) Idiosyncratic drug-induced neutropenia & agranulocytosis. QJM 110(5):299–305. https://doi.org/10.1093/qjmed/hcw220
Woo SB, Sonis ST, Monopoli MM, Sonis AL (1993) A longitudinal study of oral ulcerative mucositis in bone marrow transplant recipients. Cancer 72(5):1612–1617. https://doi.org/10.1002/1097-0142(19930901)72:5<1612::aid-cncr2820720520>3.0.co;2-q
Walsh LJ (2010) Clinical assessment and management of the oral environment in the oncology patient. Aust Dent J 55(Suppl 1):66–77. https://doi.org/10.1111/j.1834-7819.2010.01201.x
Dixon CC, Thomson FJ, Barry SM (2019) Oral manifestations of autoimmune neutropenia: a case report. J Clin Pediatr Dent 43(1):46–50. https://doi.org/10.17796/1053-4625-43.1.9
Compilato D, Cirillo N, Termine N, Kerr AR, Paderni C, Ciavarella D, Campisi G (2009) Long-standing oral ulcers: proposal for a new ‘S-C-D classification system’. J Oral Pathol Med 38(3):241–253. https://doi.org/10.1111/j.1600-0714.2008.00722.x
Elad S, Zadik Y, Caton JG, Epstein JB (2019) Oral mucosal changes associated with primary diseases in other body systems. Periodontol 2000 80(1):28–48. https://doi.org/10.1111/prd.12265
Hastürk H, Tezcan I, Yel L, Ersoy F, Sanal O, Yamalik N, Berker E (1998) A case of chronic severe neutropenia: oral findings and consequences of short-term granulocyte colony-stimulating factor treatment. Aust Dent J 43(1):9–13. https://doi.org/10.1111/j.1834-7819.1998.tb00144.x
MacPhail LA, Greenspan D, Feigal DW, Lennette ET, Greenspan JS (1991) Recurrent aphthous ulcers in association with HIV infection. Description of ulcer types and analysis of T-lymphocyte subsets. Oral Surg Oral Med Oral Pathol 71(6):678–683. https://doi.org/10.1016/0030-4220(91)90273-f
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, China medical treatment expert group for Covid-19 et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18):1708–1720. https://doi.org/10.1056/NEJMoa2002032
Bouslama B, Pierret C, Khelfaoui F, Bellanné-Chantelot C, Donadieu J, Héritier S (2021) Post-COVID-19 severe neutropenia. Pediatr Blood Cancer 68(5):e28866. https://doi.org/10.1002/pbc.28866
Mank VMF, Mank J, Ogle J, Roberts J (2021) Delayed, transient and self-resolving neutropenia following COVID-19 pneumonia. BMJ Case Rep 14(5):e242596. https://doi.org/10.1136/bcr-2021-242596
Folino F, Menis C, Di Pietro GM, Pinzani R, Marchisio P, Bosis S (2022) Incidental occurrence of neutropenia in children hospitalised for COVID-19. Ital J Pediatr 48(1):43. https://doi.org/10.1186/s13052-022-01234-5
López-Pereira P, Iturrate I, de La Cámara R, Cardeñoso L, Alegre A, Aguado B (2020) Can COVID-19 cause severe neutropenia? Clin Case Rep 8(12):3349–3351. https://doi.org/10.1002/ccr3.3369
Singh R, Ratre BK, Sirohiya P, Bhatnagar S (2021) Self-limiting severe neutropenia in a patient with COVID-19. BMJ Case Rep 14(11):e247057. https://doi.org/10.1136/bcr-2021-247057
Sampson MM, Nanjappa S, Greene JN (2017) Mucositis and oral infections secondary to gram negative rods in patients with prolonged neutropenia. IDCases 9:101–103. https://doi.org/10.1016/j.idcr.2017.06.014
Barrett AP (1987) Neutropenic ulceration. A distinctive clinical entity. J Periodontol 58(1):51–55. https://doi.org/10.1902/jop.1987.58.1.51
Ali K, Raja M, Osman S, Zulfiqar G, Janjua O (2022) Recognition and management of drug-associated oral ulceration: a review. Br Dent J 233(7):564–568. https://doi.org/10.1038/s41415-022-5032-x
De Conno F, Ripamonti C, Sbanotto A, Ventafridda V (1989) Oral complications in patients with advanced cancer. J Palliat Care 5(1):7–15
Dale DC, Cottle TE, Fier CJ, Bolyard AA, Bonilla MA, Boxer LA, Cham B, Freedman MH, Kannourakis G, Kinsey SE, Davis R, Scarlata D, Schwinzer B, Zeidler C, Welte K (2003) Severe chronic neutropenia: treatment and follow-up of patients in the Severe Chronic Neutropenia International Registry. Am J Hematol 72(2):82–93. https://doi.org/10.1002/ajh.10255
Gorsky M, Epstein J, Raviv A, Yaniv R, Truelove E (2008) Topical minocycline for managing symptoms of recurrent aphthous stomatitis. Spec Care Dentist 28(1):27–31. https://doi.org/10.1111/j.1754-4505.2008.00006.x
Yarom N, Zelig K, Epstein JB, Gorsky M (2017) The efficacy of minocycline mouth rinses on the symptoms associated with recurrent aphthous stomatitis: a randomized, double-blind, crossover study assessing different doses of oral rinse. Oral Surg Oral Med Oral Pathol Oral Radiol 123(6):675–679. https://doi.org/10.1016/j.oooo.2017.02.013
Lalla RV, Bowen J, Barasch A, Elting L, Epstein J, Keefe DM, McGuire DB, Migliorati C, Nicolatou-Galitis O, Peterson DE, Raber-Durlacher JE, Sonis ST, Elad S, Mucositis Guidelines Leadership Group of the Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO) (2014) MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 120(10):1453–1461. https://doi.org/10.1002/cncr.28592
Zadik Y, Arany PR, Fregnani ER, Bossi P, Antunes HS, Bensadoun RJ, Gueiros LA, Majorana A, Nair RG, Ranna V, Tissing WJE, Vaddi A, Lubart R, Migliorati CA, Lalla RV, Cheng KKF, Elad S, Mucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) (2019) Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27(10):3969–3983. https://doi.org/10.1007/s00520-019-04890-2
Elad S, Cheng KKF, Lalla RV, Yarom N, Hong C, Logan RM, Bowen J, Gibson R, Saunders DP, Zadik Y, Ariyawardana A, Correa ME, Ranna V, Bossi P, Mucositis Guidelines Leadership Group of the Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO) (2020) MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 126(19):4423–4431. https://doi.org/10.1002/cncr.33100
Lago ADN, Fortes ABC, Furtado GS, Menezes CFS, Gonçalves LM (2020) Association of antimicrobial photodynamic therapy and photobiomodulation for herpes simplex labialis resolution: case series. Photodiagnosis Photodyn Ther 32:102070. https://doi.org/10.1016/j.pdpdt.2020.102070
Elad S, Yarom N, Zadik Y, Kuten-Shorrer M, Sonis ST (2022) The broadening scope of oral mucositis and oral ulcerative mucosal toxicities of anticancer therapies. CA Cancer J Clin 72(1):57–77. https://doi.org/10.3322/caac.21704
Pedroni ACF, Miniello TG, Hirota C, Carvalho MH, Lascala CA, Marques MM (2020) Successful application of antimicrobial photodynamic and photobiomodulation therapies for controlling osteoradionecrosis and xerostomia after laryngeal carcinoma treatment: a case report of full oral rehabilitation. Photodiagnosis Photodyn Ther 31:101835. https://doi.org/10.1016/j.pdpdt.2020.101835
Ruiz Roca JA, López Jornet P, Gómez García FJ, Marcos Aroca P (2022) Effect of photobiomodulation on atrophic-erosive clinical forms of oral lichen planus: a systematic review. Dentistry journal 10(12):221. https://doi.org/10.3390/dj10120221
Haverman TM, Raber-Durlacher JE, Rademacher WM, Vokurka S, Epstein JB, Huisman C, Hazenberg MD, de Soet JJ, de Lange J, Rozema FR (2014) Oral complications in hematopoietic stem cell recipients: the role of inflammation. Mediators Inflamm 2014:378281. https://doi.org/10.1155/2014/378281
Queremel Milani DA, Davis DD (2023) Pain management medications. In: StatPearls. StatPearls Publishing, Treasure Island (FL)
Shetty K (2005) Thalidomide in the management of recurrent aphthous ulcerations in patients who are HIV-positive: a review and case reports. Spec Care Dentist 25(5):236–241. https://doi.org/10.1111/j.1754-4505.2005.tb01656.x
Cronshaw M, Parker S, Anagnostaki E, Mylona V, Lynch E, Grootveld M (2020) Photobiomodulation and oral mucositis: a systematic review. Dent J 8(3):87. https://doi.org/10.3390/dj8030087
Ferreira B, da Motta Silveira FM, de Orange FA (2016) Low-level laser therapy prevents severe oral mucositis in patients submitted to hematopoietic stem cell transplantation: a randomized clinical trial. Supportive care in cancer 24(3):1035–1042. https://doi.org/10.1007/s00520-015-2881-8
Salvador DRN, Soave DF, Sacono NT, de Castro EF, Silva GBL, Silva E, Pereira e Silva L, Silva TA, Valadares MC, Mendonça EF, Batista AC (2017) Effect of photobiomodulation therapy on reducing the chemo-induced oral mucositis severity and on salivary levels of CXCL8/interleukin 8, nitrite, and myeloperoxidase in patients undergoing hematopoietic stem cell transplantation: a randomized clinical trial. Lasers Med Sci 32(8):1801–1810. https://doi.org/10.1007/s10103-017-2263-1
Elad S, Zadik Y, Yarom N (2017) Oral complications of nonsurgical cancer therapies. Atlas Oral Maxillofac Surg Clin North Am 25(2):133–147. https://doi.org/10.1016/j.cxom.2017.04.006
Robijns J, Nair RG, Lodewijckx J, Arany P, Barasch A, Bjordal JM, Bossi P, Chilles A, Corby PM, Epstein JB, Elad S, Fekrazad R, Fregnani ER, Genot MT, Ibarra AMC, Hamblin MR, Heiskanen V, Hu K, Klastersky J et al (2022) Photobiomodulation therapy in management of cancer therapy-induced side effects: WALT position paper 2022. Front Oncol 30(12):927685. https://doi.org/10.3389/fonc.2022.927685
Medrado AR, Pugliese LS, Reis SR, Andrade ZA (2003) Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts. Lasers Surg Med 32(3):239–244. https://doi.org/10.1002/lsm.10126
Arany PR (2016) Craniofacial wound healing with photobiomodulation therapy: new insights and current challenges. J Dent Res 95(9):977–984. https://doi.org/10.1177/0022034516648939
Teo J, Codarini M (2001) Fevers and mouth ulcers. J Paediatr Child Health 37(5):507–509. https://doi.org/10.1046/j.1440-1754.2001.00685.x
Zakrzewska JM, Robinson P, Williams IG (1997) Severe oral ulceration in patients with HIV infection: a case series. Oral Dis 3(Suppl 1):S194–S196. https://doi.org/10.1111/j.1601-0825.1997.tb00359.x
Raber-Durlacher JE, Elad S, Barasch A (2010 Jun) Oral mucositis. Oral Oncol 46(6):452–456. https://doi.org/10.1016/j.oraloncology.2010.03.012
Aggarwal R, Bansal D, Naru J, Salaria M, Rana A, Minz RW, Trehan A, Marwaha RK (2014) HSV-1 as well as HSV-2 is frequent in oral mucosal lesions of children on chemotherapy. Supportive care in cancer 22(7):1773–1779. https://doi.org/10.1007/s00520-014-2152-0
Author information
Authors and Affiliations
Contributions
PG, JBE, and GB wrote the main manuscript text. RTS edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Güneri, P., Epstein, J.B., Bolukbasi, G. et al. Neutropenic ulcers in oncology: terminology, diagnosis, and management. Support Care Cancer 31, 716 (2023). https://doi.org/10.1007/s00520-023-08187-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-08187-3