Abstract
Background
Poor health literacy may hamper health management and long-term outcomes in breast cancer survivorship. Knowledge of factors associated with poor health literacy is needed to identify survivors in need of additional support and to improve the quality of health care, but is currently scant. Here, we explore health literacy and associated factors in a nationwide sample of long-term survivors of breast cancer.
Material and methods
All survivors aged 20–65 years when diagnosed with stage I–III breast cancer in 2011 or 2012 were identified through the Norwegian Cancer Registry, and invited to participate in the Survivorship, Work and Sexual Health (SWEET) study. Health literacy was measured using The European Health Literacy Survey Questionnaire-12 (HLS-EU-Q12) and analyzed as a continuous and categorical variable. Associations between health literacy and socioeconomic, physical, and mental health variables, including the most common late effects after cancer treatment, were explored in uni- and multivariable linear regression models.
Results
The final sample consisted of 1355 survivors (48%) with a mean age of 60 years at survey (SD 8.7). Eight years had passed since diagnosis (SD.0.7), and the majority of survivors had high socioeconomic status. Advanced judgment calls concerning treatment and health risks were reported to be the most difficult for survivors to handle. Mean health literacy sum score was 36.2 (range 12–48, SD 5.4). Thirty-nine percent had intermediate, while 19.3% reported marginal or inadequate health literacy. Education, income, age at diagnosis, the personality trait neuroticism, and fear of cancer recurrence were significantly associated with health literacy in the multivariate model, explaining 12% of the variance in health literacy scores.
Conclusion
Low levels of health literacy were prevalent in this population-based sample of long-term survivors of breast cancer, despite high socioeconomic status. Communicating and interpreting risks seem to be especially challenging. Attention to health literacy at a societal and individual level is necessary in order to provide survivorship care of high quality.
Similar content being viewed by others
Background
Health literacy (HL) is the ability to access, understand, appraise, and apply health information [1], and effect long-term health outcomes [2, 3]. Within various chronic conditions, individuals with low HL are reported to have higher mortality, more frequent use of health care services, and reduced quality of life compared to individuals with high HL [4, 5]. Almost 1 in 2 Europeans is reported to have limited HL, but there are extensive variations in prevalence likely reflecting a social gradient [2, 6]. HL is especially relevant in an oncological setting given the sheer complexity of diagnostics and treatments, and the expectations of active patient involvement [7]. Despite the importance of sound knowledge of HL in oncology, research is limited compared to other major illnesses.[8].
Self-management encompasses individuals’ ability to monitor their health and manage cognitive, behavioral, and emotional responses to preserve quality of life [9], and has been identified as a possible mediator between HL and poor health outcomes [10]. Low HL and inefficient self-management skills are associated with increasing symptom burden [11] highlighting the importance of such skills for cancer survivorship. A recent study on survivors of head and neck cancer reported lower levels of self-management behaviors and health-related quality of life among survivors with low HL compared to individuals with high HL [12].
Patients with early-stage breast cancer have excellent long-term prognosis with 5-year survival rates above 90% in the Western World [13], resulting in an increasing population of survivors of breast cancer. Survivorship is characterized by substantial uncertainty due to risks of cancer recurrence and treatment-related late effects (LEs), such as fatigue, cognitive dysfunction, mental health problems, sleep disturbances, neuropathy, and pain [14, 15]. To mitigate these risks, survivors are recommended to adhere to a healthy lifestyle and follow-up guidelines. As such, cancer survivorship resembles that of other chronic diseases, including type 2 diabetes, where effective self-management is associated with improved health outcomes [4].
Among patients with breast cancer, low HL appears to be prevalent with estimates varying between 50 and 90%, with highest estimates among elderly and in lower socioeconomic groups [16, 17]. Survivors of breast cancer with low HL report more fear of cancer recurrence (FCR) [16], a higher degree of unmet informational and supportive care needs [18], and lower health-related quality of life compared to survivors with high HL [11].
To provide sufficient and adjusted support to individuals with low HL and to increase HL and thereby self-management are potentially potent pathways for improving long-term health outcomes among survivors of breast cancer. In order to succeed, we need to be able to identify individuals with low HL. Such knowledge may also stimulate efforts at a societal and health care level aimed at improving informational provision and communication. The aims of this study were to describe HL in a large, nationwide cohort of long-term survivors of breast cancer and to explore factors associated with HL, including the most prevalent physical and mental LEs.
Material and methods
Sampling
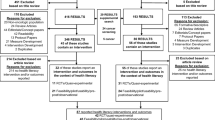
All Norwegian female survivors of breast cancer aged 20–65 years when diagnosed with breast cancer stage I–III in 2011–2012 were invited to participate in the Survivorship, Work and Sexual Health (SWEET) study, in total 2803 women. Survivors were identified through the Cancer Registry of Norway (CRN) which is based on mandatory reporting, providing close to complete prevalence estimates [19]. Survivors had to be free of prior or successive malignant disease in order to be included, with the exception of survivors diagnosed with non-melanoma skin cancer or ductal carcinoma in situ in addition to their invasive BC. One reminder was sent to survivors who did not respond to the first invitation (n = 1684). The non-responders in the SWEET study were significantly older (53.2 years at diagnosis versus 51.9 years), a larger proportion was lymph node-negative (64% versus 60%) and Her2-negative (80% versus 76%), and Ki67 was lower (mean 27 versus 31). There were no significant differences in tumor size, hormone receptor status, or type of surgery between responders and non-responders (results not shown).
Primary outcome
HL was self-reported using the European Health Literacy Survey Questionnaire-12 (HLS-Q12), a short version of the validated HLS-Q47. The short version consists of 12 items which measure HL across the four cognitive domains (access, understand, appraise, and apply health information) and the three health contexts (health care, disease prevention, and health promotion) capturing the multidimensionality of HL as proposed in the HLS-Q47 [1]. The HLS-Q12 is reported to be a valid screening tool for HL in a clinical setting, and has been validated in the Norwegian population [20]. Answers to each item are given on a 4-point rating scale from very difficult to very easy, resulting in a sum score from 12 to 48, where a higher score reflects higher levels of HL. In addition, a “don’t know” category is included for each item [20]. “Don’t know” responses and missing values were imputed with mean score of all items, if more than 80% of items were completed. In addition to the sum score, HL values were categorized into four levels based on previously defined thresholds: inadequate (12 to 26 points), marginal (27 to 32 points), intermediate (33 to 38 points), and advanced HL (39 to 48 points) [21].
Variables
Self-reported
Socioeconomic variables included education, financial income during the year prior to survey living arrangements, and employment (Table 1). Somatic comorbidity was based on a modified version of the Charlson comorbidity index [22, 23]. The personality trait neuroticism was assessed using a short version of the Eysenck Personality Questionnaire [24]. Missing values were substituted with mean values for that item from the overall sample when more than 50% of items had been answered. Cronbach’s alpha was 0.8.
Cancer-related characteristics
Age at diagnosis, pathological stage, hormone receptor and HER-2 status, and information on surgical treatment were obtained from the CRN. Additional treatment information was based on self-report.
Possible late effects after breast cancer
Pain intensity and cognitive function were assessed using the European Organization for Research and Treatment of Cancer quality of life questionnaire (EORTC- QLQ - C30 version 3) [25]. Cronbach’s alpha was 0.9. Neuropathy was assessed using the scale for chemotherapy-induced long-term neurotoxicity (SCIN) [26]. Arm and breast symptoms were assessed using the European Organization for Research and Treatment of Cancer Breast Cancer–Specific Quality of Life Questionnaire Module (EORTC QLQ-BR23 questionnaire) [27]. Cronbach’s alpha for the BR23 was 0.8. Fatigue was measured using Chalder’s Fatigue Questionnaire [28]. Cronbach’s alpha was 0.9. Sleep problems were defined using two items from the Nord-Trøndelag Health Study (the HUNT-study) [29]. Depressive symptoms were measured using The Patient Health Questionnaire-9 (PHQ-9) [30]. Cronbach’s alpha was 0.8. Anxiety symptoms were evaluated using the General Anxiety Disorder 7-item scale (GAD-7) [31] Cronbach’s alpha was 0.9. FCR was measured using four items from the Concern About Recurrence Questionnaire (CARQ) [32]. Cronbach’s alpha was 0.7 (Table 1).
Statistical analyses
Descriptive statistics was performed for the sample in total. For the HL variable, response frequencies across the 12 items of the HLS-Q12, in total and within each response category, were performed, before analyzing HL both as a categorical and continuous variable. Mean scores for HL based on imputed and original values were calculated. Univariate linear regression with HL as the dependent variable was carried out, and all statistically significant associations (p-value ≤ 0.1) were incorporated into a multivariate linear model. Survivors with one or more missing values on any of the included variables were excluded from the regression analyses. IBM SPSS statistics version 26 (SPSS, Chicago, IL) was used for all analyses.
Results
In total, 1361 survivors returned the survey (49% response rate) among whom three were excluded due to incomplete consent, and three due to self-reported breast cancer recurrence. The final sample included 1355 (48%) survivors. Mean age at time of survey was close to 60 years (59.9 years, SD 8.7), and on average, eight years (SD 0.7) had passed since diagnosis. More than half of the sample had higher education (51%), including 30% who had more than 4 years of higher education, and 68% had a high household income. At time of diagnosis, 3/4 of the survivors were employed (76.4%). Most had undergone surgical treatment (99.5%), and close to 68% had received chemotherapy. Almost 80% reported at least one comorbid condition (78%). Sleep problems were present among 44% and 20% reported a high degree of neuropathy (Table 1).
The HL item concerning the ability to judge the advantages and disadvantages of different treatment options had the lowest scores, rated as difficult or very difficult by 41.1%, followed by the item assessing the ability to judge if information on health risk in the media is reliable (35.3%). In contrast, the items on ability to follow written instructions on medications and to understand why health screening was important were reported to be easy or very easy by 91.7% and 93.8% respectively (Table 2). HL scores in the inadequate or marginal range were reported among 19.3%, while 39% had intermediate HL. The mean HL sum scores were 36.4 (SD 5.5) before imputation and 36.2 (SD 5.4) after imputation (Table 2).
In the univariate analyses, HL was associated with educational attainment (B = 2.4, p <0.01), age at survey (B = −0.07, p <0.01), and income (B = 2.2, p <0.01). Employment was inversely associated with HL (B = −1.2, p 0.01), as was neuroticism (B = −0.67, p <0.01). The only cancer-related variables associated with HL were hormone receptor positivity (B = −1.2, p 0.01) and age at diagnosis (B = −0.07, p <0.01). Comorbidity (B = −1.48, p <0.01) and all late effects (pain: B = −0.02, p-value >0.01; breast symptoms: B = −0.04, p <0.01; arm symptoms: B = −0.03, p <0.01; neuropathy: B = −0.87, p 0.04; sleep problems: B = −0.67, p <0.01; fatigue: B = −0.11, p <0.01; depressive symptoms: B = −0.21, p <0.01; anxiety symptoms: B = −0.32, p <0.01; and fear of cancer recurrence: B = −0.15, p <0.01) were inversely associated with HL, except for cognitive function which was positively associated with HL (B = 0.03, p <0.01) (Table 3).
In multivariate analyses, HL was significantly associated with more than 4 years of higher education (B =1.32, p <0.01), age at diagnosis (B = −0.08, p <0.01) and income (B = 1.1, p 0.01). Other socioeconomic variables were no longer significantly associated with HL. FCR and neuroticism remained inversely associated with HL (B = −0.08, p <0.01, and B = −0.27, p 0.03 respectively). All other late effects were non-significant in the adjusted analyses. The included explanatory variables collectively explained 12% of the variance in HL (R2adj 0.12) (Table 4). Age at survey was not included in the analysis due to high collinearity with age at diagnosis.
Discussion
Despite high socioeconomic status, one in five long-term survivors of breast cancer had HL levels in the marginal or inadequate range. If not provided with sufficient support, survivors with HL at this level may struggle to understand and make use of health-related information and engage in effective self-management, which are key aspects of successful cancer survivorship.
Three HL items were labelled as difficult or very difficult by less than 10% of the sample, reflecting a high degree of more basic or functional HL skills present in the sample, such as following written instructions. However, 35–41% reported difficulty with advanced HL tasks, such as complex judgment calls regarding treatment and health risks, which reflect the cognitive domain “appraisal” in the original HL framework [1]. These findings support the theory that HL is as a multi-dimensional concept which may vary across health-related contexts. This is in line with other studies, including the European Health Literacy survey (HLS-EU), where items reflecting more advanced, critical HL skills were experienced as the most difficult [6, 33]. In the HLS-EU, HL was as expected highest in Western European countries, but with substantial variations related to age, health, and socioeconomic status [6]. Breast cancer risk is positively associated with high socioeconomic status, and the majority of survivors in this survey had high SES. This may account for the relatively high mean HL score. The most critical HL skills for cancer survivorship may still be lacking for a substantial proportion of survivors. In line with previous findings, we observed an association between lower HL and increasing age [12, 16]. Old age involves declining sensory and cognitive functioning which may affect HL skills directly. Additionally, with age, the risk of comorbidity also increases. Multi-morbid, more fragile patients report lower HL when faced with cancer than patients with higher performance status [11], possibly because they already engage in complex self-management behaviors. Dealing with cancer in this context may exceed their overall coping capacity. Survivors of older age may therefore represent a particularly vulnerable group with regard to the effects of low HL.
FCR, the persistent fear or worry that the cancer will return or progress [34], is a frequent concern among survivors of breast cancer [35], shown to persist over time, also among survivors with favorable long-term prognosis, such as survivors of breast cancer [36]. In the present study, FCR was the only late effect that remained significantly associated with HL in the adjusted model. Our finding is in line with results presented by Halbach et al. who concluded that limited HL is an independent risk factor for higher levels of FCR [16]. Low HL may impact the risk of FCR through different mechanisms, such as reduced ability to navigate, critically assess, understand, and handle health-related information, but also through sub-optimal interaction with health care providers, for instance, through avoidance behavior. Among patients with cancer, low HL has been associated with lower perceived information provision and information satisfaction compared to higher HL [37]. Combined, low HL may result in unmet informational and supportive care needs and perhaps unnecessarily high levels of FCR, as demonstrated in previous studies [18].
In an oncological setting, neuroticism, the propensity for negative emotions when faced with negative stress, has been associated with reduced quality of life and increased risk of post-traumatic stress disorder following cancer [38]. Neuroticism may affect self-management behaviors, as reported for patients with other chronic diseases such as diabetes [39], thereby linking it to HL skills. Although research is limited, low HL has been associated with neuroticism [40]. We observed the same association, which remained stable in the adjusted analyses. We have not been able to find other studies specifically exploring HL and neuroticism among survivors of breast cancer warranting further investigations. Our finding implies that specific personality characteristics may indicate poorer HL skills. Such knowledge may be valuable in a clinical setting making it easier for clinicians to identify individuals at risk of poorer outcomes.
As symptom burden and functional limitations increase, self-perceived HL and self-management seem to decline [11]. Following this line of reasoning, individuals with low HL may be particularly vulnerable when faced with treatment-related late effects. This was not the case in the present sample. This may be due to the survivors’ relatively high HL levels, enabling them to handle these stressors, or that increasing demands in fact has stimulated HL skills over time. It is also possible that HL is more clearly linked to late effects during the first years of cancer survivorship, before effective coping strategies are in place and the emotional distress is likely to be higher. Exploring HL among patients living with advanced breast cancer will be interesting for further studies.
Strengths and limitations
Survivors of breast cancer included in this study were recruited from an unselected, unbiased population. All long-term, early-stage survivors diagnosed with breast cancer and within working age registered in the CRN were invited to participate, granting us with a large sample of high quality.
Given the inclusion criteria for the present study, non-responders did not differ according to diagnosis (early-stage BC), gender, or time of diagnosis. Additional clinical data from the CRN concerning cancer-related variables revealed only slight differences between responders and non-responders. We cannot exclude the possibility that non-responders differ according to other variables, such as ethnic background and HL skills, as reading and understanding Norwegian were necessary in order to complete the questionnaire. However, data use restrictions prohibited us from performing complete analyses of the non-responders. Although declining response rates in health surveys in general may threaten external validity, a response rate of 49% is considered acceptable and comparable to other large-scale surveys on long-term survivors of cancer in Norway [41]. Furthermore, in comparable survey studies, with more modest response rates than reported here, evidence of response bias was not found [42].
This sample reflects the Norwegian population of breast cancer survivors, which is quite homogenous in terms of SES and ethnic background. Although the results are likely to be generalizable to a Scandinavian and Western European setting, more caution must be paid when interpreting the results within a more global context. We only included survivors of working age at diagnosis (20–65 years) given the main outcomes of interest in the SWEET study. Inclusion of the oldest age groups may have further underlined the importance of increasing age as a risk factor for poor HL and should be further explored in upcoming studies. Due to the cross-sectional design, we were unable to explore the directionality between HL and the other variables. A prospective methodology should be applied to assess these associations further. Data on HL is based on self-report and reflect present skills.
Although validated in the Norwegian population and for Norwegians with diabetes type II [20, 43], the HLS-Q12 it has not been extensively used. Furthermore, categorization of HL is empirically based, and threshold values will vary. Consequently, we chose to use HL as a continuous variable for the regression analyses. The HLS-Q47 allows for the opportunity to measure HL across three health care settings. This procedure has not been described for the HLS-Q12 as of yet. Still, the HLS-Q12 is reported to be a valid, quick, and easy-to-use tool to measure HL in a clinical setting.
Conclusions
Within this nationwide cohort of long-term survivors of breast cancer, one in five reports HL levels within the marginal or inadequate range. Despite high SES, HL tasks specifically pertaining to advanced judgment calls were rated as difficult or very difficult by 35–41%, demonstrating that both presenting risk and understanding risk are challenging. This study demonstrates that the presence of basic HL does not automatically imply more advanced skills, which are likely to be the most crucial with regard to long-term survivorship. Sufficient individual support must be provided alongside implementing measures to improve HL at a societal and health care level. Survivors with higher age, neurotic personality traits, and reports of FCR may warrant specific attention from health care providers. It needs to be recognized that HL is likely to vary over time, with context and functional demands, and identification of individuals at risk of low HL based on objective markers alone is insufficient.
Availability of data
All data are available at Oslo University Hospital.
Code availability
Not applicable
References
Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H (2012) Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 12:80
Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K (2011) Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 155(2):97–107
PJ KI, Apfel F et al (2013) Health literacy: the solid facts. World Health Organization 2013, Europe
Bailey SC, Brega AG, Crutchfield TM, Elasy T, Herr H, Kaphingst K, Karter AJ, Moreland-Russell S, Osborn CY, Pignone M et al (2014) Update on health literacy and diabetes. Diabetes Educ 40(5):581–604
Muellers KA, Chen L, O'Conor R, Wolf MS, Federman AD, Wisnivesky JP (2019) Health literacy and medication adherence in COPD Patients: when caregiver presence is not sufficient. Copd 16(5-6):362–367
Sørensen K, Pelikan JM, Röthlin F, Ganahl K, Slonska Z, Doyle G, Fullam J, Kondilis B, Agrafiotis D, Uiters E et al (2015) Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Pub Health 25(6):1053–1058
Koay K, Schofield P, Jefford M (2012) Importance of health literacy in oncology. Asia-Pac J Clin Oncol 8(1):14–23
Kieffer Campbell J (2020) Health literacy in adult oncology: an integrative review. Oncol Nurs Forum 47(1):18–32
Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J (2002) Self-management approaches for people with chronic conditions: a review. Patient Educ Couns 48(2):177–187
Mackey LM, Doody C, Werner EL, Fullen B (2016) Self-management skills in chronic disease management: what role does health literacy have? Medical Decision Making : an International Journal of the Society for Medical Decision Making 36(6):741–759
Eton DT, Anderson RT, Cohn WF, Kennedy EM, St Sauver JL, Bucknell BJ, Ruddy KJ (2019) Risk factors for poor health-related quality of life in cancer survivors with multiple chronic conditions: exploring the role of treatment burden as a mediator. Patient Relat Outcome Meas 10:89–99
Clarke N, Dunne S, Coffey L, Sharp L, Desmond D, O'Conner J, O'Sullivan E, Timon C, Cullen C, Gallagher P (2021) Health literacy impacts self-management, quality of life and fear of recurrence in head and neck cancer survivors. J Cancer Surviv Res Pract
Cancer in Norway 2019 - Cancer incidence, mortality, survival and prevalence in Norway. Oslo: Cancer Registry of Norway, 2020
Joly F, Lange M, Dos Santos M, Vaz-Luis I, Di Meglio A (2019) Long-term fatigue and cognitive disorders in breast cancer survivors. Cancers:11(12)
Rietman JS, Dijkstra PU, Hoekstra HJ, Eisma WH, Szabo BG, Groothoff JW, Geertzen JH (2003) Late morbidity after treatment of breast cancer in relation to daily activities and quality of life: a systematic review. European Journal of Surgical Oncology : the Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 29(3):229–238
Halbach SM, Enders A, Kowalski C, Pförtner TK, Pfaff H, Wesselmann S, Ernstmann N (2016) Health literacy and fear of cancer progression in elderly women newly diagnosed with breast cancer--A longitudinal analysis. Patient Educ Couns 99(5):855–862
Rakhshkhorshid M, Navaee M, Nouri N, Safarzaii F (2018) The Association of Health Literacy with Breast Cancer Knowledge, Perception and Screening Behavior. Eur J Breast Health 14(3):144–147
Halbach SM, Ernstmann N, Kowalski C, Pfaff H, Pförtner TK, Wesselmann S, Enders A (2016) Unmet information needs and limited health literacy in newly diagnosed breast cancer patients over the course of cancer treatment. Patient Educ Couns 99(9):1511–1518
Larsen IK, Småstuen M, Johannesen TB, Langmark F, Parkin DM, Bray F, Møller B (2009) Data quality at the Cancer Registry of Norway: an overview of comparability, completeness, validity and timeliness. European Journal of Cancer (Oxford, England : 1990) 45(7):1218–1231
Finbråten HS, Wilde-Larsson B, Nordström G, Pettersen KS, Trollvik A, Guttersrud Ø (2018) Establishing the HLS-Q12 short version of the European Health Literacy Survey Questionnaire: latent trait analyses applying Rasch modelling and confirmatory factor analysis. BMC Health Serv Res 18(1):506
Guttersrud Ø, Pettersen KS, Finbråten HS (2019) Measuring health literacy using HLS-NO-Q12: Empirically identifying and describing cumulative benchmarks for statistically different levels of performance. In: The 4th European Health Literacy Conference, Dublin
Armitage JN, van der Meulen JH (2010) Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg 97(5):772–781
Brusselaers N, Lagergren J (2017) The Charlson comorbidity index in registry-based research. Methods Inf Med 56(5):401–406
Grav S, Stordal E, Romild UK, Hellzen O (2012) The relationship among neuroticism, extraversion, and depression in the HUNT Study: in relation to age and gender. Issues Ment Health Nurs 33(11):777–785
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Oldenburg J, Fosså SD, Dahl AA (2006) Scale for chemotherapy-induced long-term neurotoxicity (SCIN): psychometrics, validation, and findings in a large sample of testicular cancer survivors. Qual Life Res Int J Qual Life Asp Treat Care Rehab 15(5):791–800
Sprangers MA, Groenvold M, Arraras JI, Franklin J, te Velde A, Muller M, Franzini L, Williams A, de Haes HC, Hopwood P et al (1996) The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology 14(10):2756–2768
Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, Wallace EP (1993) Development of a fatigue scale. J Psychosom Res 37(2):147–153
Krokstad S, Langhammer A, Hveem K, Holmen TL, Midthjell K, Stene TR, Bratberg G, Heggland J, Holmen J (2013) Cohort Profile: the HUNT Study. Norway Int J Epidemiol 42(4):968–977
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613
Spitzer RL, Kroenke K, Williams JB, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092–1097
Thewes B, Zachariae R, Christensen S, Nielsen T, Butow P (2015) The Concerns About Recurrence Questionnaire: validation of a brief measure of fear of cancer recurrence amongst Danish and Australian breast cancer survivors. J Cancer Surviv Res Pract 9(1):68–79
Heijmans M, Waverijn G, Rademakers J, van der Vaart R, Rijken M (2015) Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ Couns 98(1):41–48
Lebel S, Ozakinci G, Humphris G, Mutsaers B, Thewes B, Prins J, Dinkel A, Butow P (2016) From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Supportive Care in Cancer : Official Journal of the Multinational Association of Supportive Care in Cancer 24(8):3265–3268
Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, Ozakinci G (2013) Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv Res Pract 7(3):300–322
Vandraas KF, Reinertsen KV, Kiserud CE, Lie HC (2020) Fear of cancer recurrence among young adult cancer survivors-exploring long-term contributing factors in a large, population-based cohort. J Cancer Surviv Res Pract
Verkissen MN, Ezendam NPM, Fransen MP, Essink-Bot M-L, Aarts MJ, Nicolaije KAH, Vos MC, Husson O (2014) The role of health literacy in perceived information provision and satisfaction among women with ovarian tumors: A study from the population-based PROFILES registry. Patient Educ Couns 95(3):421–428
Dahl AA (2010) Link between personality and cancer. Future Oncology (London, England) 6(5):691–707
Novak JR, Anderson JR, Johnson MD, Hardy NR, Walker A, Wilcox A, Lewis VL, Robbins DC (2017) Does personality matter in diabetes adherence? Exploring the pathways between neuroticism and patient adherence in couples with Type 2 diabetes. Appl Psychol Health Well-Being 9(2):207–227
Kim HZQ, Svynarenko R (2017) Personality traits and health literacy. J Family Med Commun Health 4(1):1102
Bøhn SH, Lie HC, Reinertsen KV, Fosså SD, Haugnes HS, Kiserud CE, Loge JH, Wisløff T, Thorsen L (2021) Lifestyle among long-term survivors of cancers in young adulthood. Supportive Care in Cancer : Official Journal of the Multinational Association of Supportive Care in Cancer 29(1):289–300
Lie HC, Rueegg CS, Fossa SD, Loge JH, Ruud E, Kiserud CE (2019) Limited evidence of non-response bias despite modest response rate in a nationwide survey of long-term cancer survivors-results from the NOR-CAYACS study. J Cancer Surviv Res Pract 13(3):353–363
Finbråten HS, Pettersen KS, Wilde-Larsson B, Nordström G, Trollvik A, Guttersrud Ø (2017) Validating the European Health Literacy Survey Questionnaire in people with type 2 diabetes: Latent trait analyses applying multidimensional Rasch modelling and confirmatory factor analysis. J Adv Nurs 73(11):2730–2744
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital) This study was funded by the Pink Ribbon Movement and Norwegian Breast Cancer Society through grant nr 197255.
Author information
Authors and Affiliations
Contributions
VR and KV were in charge of research design and data collection. KV, KVR, and CEK designed this sub-study, KV performed all statistical analysis together with HCL. All authors contributed through the entire process including interpretation.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Regional Committee for Medical Research Ethics (2018/2170), the Norwegian Cancer Registry, and the Data Protection Officer at Oslo University Hospital.
Informed consent to participate
Informed consent was obtained from all participants included in the study.
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vandraas, K.F., Reinertsen, K.V., Kiserud, C.E. et al. Health literacy among long-term survivors of breast cancer; exploring associated factors in a nationwide sample. Support Care Cancer 30, 7587–7596 (2022). https://doi.org/10.1007/s00520-022-07183-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07183-3