Abstract
Breast cancer accounts for 25% of all cancers among Canadian females. Despite successes of decreased mortality, adverse treatment effects, such as cardiotoxicity, contribute to a sedentary lifestyle and decreased quality of life. Physical activity (PA) is a possible therapy for the late effects; however, COVID-19 restricted access to in-person cardiovascular rehabilitation (CR) programs. The purposes are as follows: (1) compare PA of breast cancer survivors’ in-person CR to virtual CR following a transition during COVID-19 and (2) compare the PA of the pandemic cohort to a matched cohort who had completed the program in 2018/2019; (3) explore survivors’ experiences of transitioning to and engaging in virtual CR. Mixed methods included analysis of CR PA data from a pandemic cohort (n = 18) and a 2018/2019 cohort (n = 18) and semi-structured focus group interviews with the pandemic cohort (n = 9) in the context of the PRECEDE-PROCEED model. After the transition, there were no significant differences in mean activity duration, frequency, and cumulative activity (expressed as MET-minutes) (p > 0.05). However, variation of PA duration doubled following the transition from in-person to virtual (p = 0.029), while for the 2018/2019 cohort, variation remained unchanged. Focus groups revealed that women valued their CR experiences pre-COVID-19 and had feelings of anxiety during the transition. Perceived factors affecting participation were environmental, personal, and behavioural. Recommendations for virtual programs were to increase comradery, technology, and professional guidance. PA experiences during a transition to virtual care prompted by a pandemic vary among breast cancer survivors. Targeting individualised strategies and exercise prescriptions are important for improving PA programs and patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The vast majority (88%) of females with breast cancer survive more than 5 years; however, they have an increased risk of cardiovascular-specific mortality (1.3- to 3.6-fold) compared to age-matched values which may relate to direct and indirect cardiotoxic side effects of treatment [1]. A cardio-oncology rehabilitation model adapted from the comprehensive approach of cardiac rehabilitation (CR) prevents or reduces the severity of cardiovascular events for cancer survivors [1]. Exercise training is safe and effective and improves cardiorespiratory fitness, strength, body composition, fatigue, anxiety, depression, and quality of life [2].
CR programs were suspended or drastically altered due to the novel coronavirus (COVID-19) pandemic [3,4,5]. Protective restrictions influenced lifestyle at the population level, and early studies suggest potentially negative consequences on health behaviours [3]. With social isolation potentially causing changes to PA, Cunningham and O’Sullivan also suggested that disease and disorders related to inactivity will increase following the pandemic [3, 6]. This increased risk is of particular importance in breast cancer survivors who are already at higher risk of cardiovascular disease following treatment.
It is established that in-person CR programs have proven benefits for cardiorespiratory fitness as well as cancer-related side effects, and virtual programs such as coaching apps and community-based programs are promising for behaviour change and personalised guidance [7, 8]. However, the effects of a sudden transition to virtual care during a pandemic are unknown. Typical perceived barriers to participation may be exacerbated, such as those related to the environment (e.g. absence of equipment or access to facilities, safety), physical factors (e.g. mobility restrictions, lack of energy, fatigue, pain, worsening of disease), and psychosocial factors (e.g. lack of motivation, time, lack of confidence and skills, lack of support or someone to accompany) [9, 10].
We conducted a mixed methods study to better understand the effects of COVID-19 on PA in breast cancer survivors transitioning to a virtual CR program. Participants’ duration, METs, and frequency of moderate-vigorous PA performed weekly in-person before the COVID-19 pandemic were compared to weekly PA in a virtual CR model during the COVID-19 pandemic. Additionally, we compared the breast cancer survivors who transitioned to virtual care during the COVID-19 pandemic to a 2018/2019 cohort who had completed only in-person CR. Semi-structured focus groups, based on the PRECEDE-PROCEED model of health promotion, explored participants’ experiences, including the barriers, facilitators, and feelings that contributed to women’s ability to participate [11].
Methods
Study design
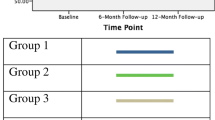
CR PA data from two groups were analysed: Breast cancer survivors enrolled in an in-person 2020 CR program who then transitioned to virtual CR (pandemic cohort) and an in-person only cohort (2018/2019 cohort) (Fig. 1). Semi-structured focus groups that elicit responses from group interactions were completed with the pandemic cohort, a particularly appropriate approach for females with breast cancer who prefer a group setting for exercise [12, 13]. The design merges the strengths of quantitative database analysis and qualitative techniques to quantify and explore participant’s experiences to provide a stronger understanding [14].
Participants
Both cohorts were drawn from the breast cancer specific CR program at the Toronto Rehabilitation Institute (TRI), Health, Exercise, Active Living and Therapeutic Lifestyle (HEALTh). This program seeks to improve cardiovascular health and follows the standard-of-care CR framework to improve physical (e.g. cardiorespiratory fitness) and psychological (e.g. quality of life and depression) function [15].
Patients were defined as early-stage, female, breast cancer survivors who had completed any phase of cancer treatment (i.e. surgery, chemotherapy, radiation, hormonal) [16]. Participants with incomplete files were excluded.
Intervention: virtual CR
Due to COVID-19 restrictions, the TRI program transitioned from in-person to virtual care in March 2020 over 1-3 weeks. The in-person CR PA prescription approach (Online Resource 1) remained unchanged in the virtual model [16]. Participants completed 8 ± 6.4 weeks in-person, and the remainder of sessions were completed virtually, for a total 22 weeks (pandemic cohort). Patients were contacted via telephone calls and/or email once a week by a CR supervisor to provide exercise recommendations, mental health, and dietary support. Educational seminars via an online platform (cardiaccollege.ca) were offered to patients, including topics about exercise, well-being, nutrition, medications, cardiovascular disease, and novel information concerning COVID-19.
Database review
Retrospective data were extracted from the TRI institutional electronic database for patients who previously consented. Descriptive measures are reported for baseline. PA data included approximately 4 weeks before and 4 weeks after the transition from in-person to virtual CR. PA duration was converted to MET-minutes/week using the corresponding MET values from the Compendium of Physical Activities [17].
Participants from the 2018/2019 cohort were matched (by JL) to the pandemic cohort in terms of duration of participation in CR, age (± 2.8 years), sex, primary diagnosis, and baseline physical fitness level (VO2peak: ± 1.5 mL∙kg-1∙min-1).
Focus groups
We aimed to recruit 8–12 participants from the pandemic cohort through email and phone calls, each freely provided informed consent to participate. This convenience sample followed the recommendation to have more online focus groups with fewer participants [12].
Step three of the PRECEDE-PROCEED model, with its focus on educational and ecological assessments, was used to create the script. This step considers three types of factors that affect health promotion: (a) predisposing factors, such as individual knowledge and attitudes; (b) enabling factors, including the environment and social action; and (c) reinforcing factors, such as behaviours and support after health programs [11]. The script was piloted (Online Resource 2) and revised based on CR expert feedback.
Focus groups took place virtually using an online meeting platform. Open-ended recursive questions, probes, and reflective re-iteration addressed experiences during the transition from in-person to virtual, barriers and facilitators of exercise, and ideas on how to improve the CR program. The 90-min sessions were facilitated by the primary author (JL), digitally audio recorded, and transcribed verbatim by JL which provided immersion in the data analyses [18]. Field notes were compiled and summarised by LV to facilitate member checking, with participants given the opportunity to review and clarify the summary of responses to each question.
Data analysis
Quantitative
Descriptive statistics were used to summarise participant characteristics in the two cohorts. Differences between continuous variables were tested using independent and paired-samples t-test and Wilcoxon signed rank test. Homogeneity of variance was assessed using Levene’s Test. Associations between variables were quantified using Pearson’s correlations. A priori power calculation was performed using G*Power version 3.1.9.7. SPSS version 26.0 (SPSS Inc., Chicago, IL, USA) was used for all analyses, and statistical significance was set as 5%.
Qualitative
Braun and Clarke’s six-phased, iterative, and reflexive approach to thematic analysis was followed using Microsoft Excel software [18]. Transcripts were reviewed by all researchers, and two authors (JL and LV) independently coded and identified categories and preliminary themes inductively. To achieve rigour, JL and LV acted as “critical friends” throughout the data analysis process [19]. Evolving themes were reviewed by all authors, and unanimous consensus was obtained following debate and critical peer discussions. The aforementioned components of step three of the PRECEDE-PROCEED model provided structure for data interpretation while targeting the assessment of participants’ health needs and evaluation of the CR program [11]. This model was appropriate for use as it has been used to design health education programs to increase exercise among rural breast cancer survivors, and it addresses environmental factors that directly or indirectly affect behaviour [20, 21]. Data saturation was achieved when no new themes emerged from thematic analysis following the third focus group session [22]. The consolidated criteria for reporting qualitative research were used to ensure quality, and important aspects of the qualitative investigation were reported [22].
Results
Retrospective data
Eighteen female breast cancer survivors who completed the transition to virtual CR were identified (Table 1). The matched 2018/2019 cohort did not differ on baseline characteristics (Table 1). Baseline VO2peak were in the 20th and 30th Canadian normative percentiles [23].
Participation in CR programs
Duration and frequency of PA did not differ within or between the pandemic and 2018/2019 cohort at the matched first (approx. 1.5 month from entry) or second (approx. 3 months) time points (p > 0.05) (Table 2). However, variation of PA duration doubled for the pandemic cohort from the first time point in-person (SD = 51 min/week) to the second virtual time point (SD = 105 min/week) (F(1,34) = 5.183, p = 0.029), while this variation remained unchanged for the 2018/2019 cohort. When grouped, 39% of pandemic participants saw a significant increase in PA duration (p = 0.024), whereas 56% significantly decreased (p = 0.005), with 6% having no change (Table 3). Comparatively, the 2018/2019 cohort saw a significant increase in 61% of participants (p < 0.01) and a non-significant decrease in 33% and maintenance in 6%.
For both cohorts, there were no correlations of change in PA duration minutes/week with time since diagnosis (r = 0.086, p = 0.743), BMI (r = 0.172, p = 0.495), VO2peak (r = -.149, p = 0.555), age (r = 0.046, p = 0.855), CES-D (r = 0.165, p = 0.608), or duration of participation (r = -0.235, p = 0.349). There were no significant differences between the cohorts for mean change in duration of PA +2.7 min/week (p = 0.919), frequency of PA -0.05 days/week (p = 0.977), or cumulative MET-minutes/week -30.3 (p = 0.5). Given the large variations with power (1-β) set at 0.80 and α = 0.05, two-tailed, the sample size would have to exceed 34 per group for differences to reach statistical significance at the .05 level.
Focus groups
Nine pandemic cohort breast cancer survivors participated in three semi-structured focus groups (2, 3, and 4 participants) (Table 1). Baseline VO2peak was in the 10th percentile of Canadian norms [23].
Thematic analysis revealed four overarching themes and seven subthemes. Overarching themes include the following: “unified as a group pre-COVID-19”, “the transition in CR experience due to COVID-19”, “CR participation during COVID-19”, and “Recommendations: stay connected and continue on”. Table 4 contextualises the themes in relation to step three of the PRECEDE-PROCEED model. The number of participants who experienced the responses is noted (e.g. 7/9).
Theme 1: unified as a group pre-COVID-19
All participants expressed positive experiences while participating in in-person CR. They reported enjoyment (9/9) and highlighted the comradery and unification as a group (6/9). Some women appreciated the professional guidance and accountability to the CR supervisor (4/9). The routine of CR was reported to be helpful (5/9).
Theme 2: the transition in CR experience due to COVID-19
The end of in-person CR was difficult for most women (7/9). They experienced anxiety, depression, disappointment, and feelings of abandonment. Some were tolerant of the change (2/9). Participants expressed increased stress related to follow-up medical appointments during COVID-19 (5/7). Main stressors were personal protection measures and procedures at the hospitals, anxiety of getting sick, and delays of follow-up appointments.
The women all displayed commitment to remain in the program as it transitioned. Their rationale was to complete the program (2/8), stay engaged and connect with others (4/8), and see how the program would evolve in a virtual setting (2/8).
Theme 3: CR participation during COVID-19
Participants perceived their PA to either decrease (6/8) or be maintained (2/8) after they transitioned from in-person to virtual programming. They noted that virtual was not as fulfilling as their in-person experience. Some women reported that they were not provided with enough details to access the virtual program or that they lacked skills to use it.
In addition to the guidance of the CR supervisor, the women’s PA levels were affected positively by support from family and friends (4/9), access to equipment (6/9), and good weather (3/9). If the CR supervisor made routine calls/emails and displayed compassion to their struggles, it was considered good professional guidance. Support from family and friends included spouses and neighbours joining in PA. Access to a stationary bicycle, walking the dog and public parks were the main resource facilitators.
The participants expressed the loss they felt without the face-to-face connection to each other and difficulty associated with performing their activities alone. The women shared their perceived negative experiences that included the following: a lack of comradery (7/9), professional guidance (6/9), and resources (4/9); overcrowding and COVID-19 concerns (4/9); and bad weather (3/9). The perceptions of support from their CR leader included reduced follow-ups to questions about their training plan, lack of specificity through email, or reduced personal connection to the leader. Many expressed concerns of going to public places where social distancing was not followed for fear of contracting COVID-19. Additionally, the lack of facilities, equipment, or space at home was a barrier. When the weather was too cold or hot, it was an issue for exercising outside.
The women shared the importance of being active and their motivation to feel better and mitigate treatment symptoms such as fatigue (7/9). Despite the awareness of the benefits of PA, most women reported they lacked motivation (5/7), routine (3/7), or skill (3/7), and missed the support or inspiration provided previously in in-person CR (7/9). Barriers included full-time work and/or family members to take care of; inconsistent timing of contact from the CR supervisor, frustration with the online platform, and fear of hurting themselves or not doing the exercises right.
Theme 4: recommendations—stay connected and continue on
Participants’ recommendations to improve the virtual program delivery focused on increasing comradery (6/9), the use of technology (6/9), professional guidance (6/9), and improving routine (3/9). The women suggested connecting the group through personal emails or phone numbers to talk or workout together virtually or while physically distanced. Other suggestions included an app to monitor their progress, improved video quality, and demonstration of the exercises. More educational components, specific follow-ups at a set time each week and video chats with CR supervisors were recommended. Finally, virtual sessions scheduled routinely may help with motivation to stay physically active.
Discussion
PA behaviours of breast cancer survivors were explored between in-person and virtual CR during the COVID-19 pandemic with focus groups explaining the quantitative results. The qualitative analysis provides additional information regarding feelings during the transition, perceived factors affecting participation, and recommendations for virtual programs. Firstly, the CR virtual model preserved PA according to the recommended protocol of moderate intensity aerobic exercise at least three times per week for at least 30 min [24]. The finding suggests that the TRI CR program had a positive impact during COVID-19. The focus groups confirm the benefits of professional guidance of the TRI CR program, social support, and shared experience between breast cancer survivors as contributors to activity maintenance and to the positive experience and health benefits of in-person CR [9]. As general comparators, the first COVID-19 lockdown in Spain saw a significant decrease of moderate-intensity PA in females with chronic conditions which included cancer (-33.2 min/day) [25]; in Turkey, the mean PA level for post-menopausal women was low during quarantine [26]; in Japan, female older adults’ PA was reduced by 5–10% at the onset of COVID-19 restrictions [27]. In pre-COVID-19 studies only 32% met PA recommendations, and 70% were not consistently exercising following breast cancer [24, 28].
The virtual CR model appears to have helped participants maintain PA and may have helped with coping through the pandemic given the known association between PA and health. This aligns with other research. Post-menopausal females who exercised before COVID-19 had higher PA levels during the pandemic [26]. Peterson et al., (2021) suggested that higher self-efficacy for PA may help overcome the barriers presented by the pandemic [29]. Older adults with social interaction had higher odds of maintaining PA during the restrictions in Japan [27] and a systematic review of CR models revealed no difference in main health outcomes for those who received a virtual intervention compared to centre-based CR [30]. As well, a recent randomised control trial found virtual CR was safe and superior to usual care in reducing cardiovascular disease risk [31].
Secondly, the variation of PA duration and frequency in the pandemic group differed significantly (two times as large) from the in-person 2018/2019 cohort. This suggests subgroups or individual differences in behaviour. It is speculated that a decline in PA could be from physical or psychosocial effects of breast cancer and an increase in PA could stem from the motivation to prolong healthy survival or sociodemographic and socioeconomic reasons [28, 32, 33]. Enduring a natural disaster or adjusting to a global pandemic may cause emotional distress, disrupt routine and affect PA levels [34,35,36,37]. While PA was affected positively by the motivation to feel better, focus groups revealed that it was affected negatively by an overall lack of motivation. Family support, feedback by trainers, access to CR, social support, and engaging in PA with others affected by cancer were expected environmental facilitators [38,39,40].
The motivation to finish the program suggest that survivors seek feelings of self-control after a cancer diagnosis and treatment [9, 41]. During a pandemic, when the world is rapidly changing, loss of control could be exacerbated, thus further encouraging women to engage in a structured program. On a positive note, the women remained enrolled in the program as it transitioned to a virtual format. The women were aware of the benefits of PA, but this was not a priority given the stressors of the pandemic. The results reported anxiety, depression, disappointment, and abandonment during the transition to virtual CR at the beginning of COVID-19 which may have contributed to subsequent PA reductions for some individuals.
Furthermore, participants reported that in the early days, there was limited publicity of exercise or other healthy behaviours coming from news outlets or government officials. A previous virtual study indicated that personal facilitators included ongoing support from healthcare providers and self-management activities [42]. Continuation of education in a virtual CR format, from a support network they were comfortable with, may help women stay motivated to maintain PA.
The stress regarding appointments and delays for oncology/surgery follow-up are consistent with other cancer patients who reported higher depression and anxiety levels during the pandemic, correlated with the disruption of their treatment [43]. The participants in our study were fearful of going to potentially crowded public spaces, another potential contributor to the anxiety they experienced [44].
The pandemic also created unique barriers to access support from other participants and professionals. The Cancer Care Ontario “Exercise for People with Cancer” guidelines recommend that survivors exercise in a group setting with their peers to increase quality of life and fitness outcomes [13]. This was not possible during the Spring 2020 lockdown. Moreover, as participants noted, virtual communication does not compare to face-to-face human interaction. Furthermore, due to the shutdown of public gyms, access/use of personal equipment varied depending on existing supply, space, and proximity to parks. Education on safe outdoor activities could address this barrier.
Finally, behavioural barriers were noted as lack of time, lack of routine, technology issues, and poor computer skills, barriers also identified by Banner et al. [42]. COVID-19 may have exacerbated these barriers with employees working from home and children of all ages attending class online. Participants with families reported taking on bigger roles at home and putting others before their own health [9].
Study limitations
No objective data regarding compliance with the prescribed exercise was available. Although the sample size may reduce the generalisability of these results to other populations, the results do provide insight into contrasting PA patterns in an in-person program with virtual CR during a pandemic.
Focus groups occurred after CR was completed, and it cannot be determined how participants’ perceptions may have been relayed in the moment. Moreover, circumstances may limit the transferability to other subgroups: individuals were diagnosed with early-stage breast cancer, attended CR in-person, chose to continue CR as it transitioned, had a computer, and were comfortable discussing their experiences of PA.
Future directions
Given the value of peer support during in-person CR, the creation of an online chat group/phone application could help to unify participants, increase their sense of connection, and encourage participation in cardio-oncology rehabilitation programs. Participants’ preferences for professional contact type and online participation could be addressed in future virtual programs. Participants should be provided training on the virtual platform and personalised contact options, for example, phone calls, video chat, or texts to suit their varying lifestyles. Participants suggested more contact from health professionals, tracking PA via an application, and live online videos at regularly scheduled times. Discussions with CR supervisors to reduce barriers from the pandemic, as well as opportunities to identify creative solutions for staying active, could also give breast cancer survivors a greater sense of control.
Conclusion
Prescribed PA is a possible adjuvant therapy for the late effects of cancer, the pandemic restricted access to in-person CR programs. Increased effort is needed to implement virtual models because PA levels and participant satisfaction differ after the transition [45]. In this study, average PA for virtual CR was similar but highly variable compared to in-person levels, and the PA experiences and behaviours varied among breast cancer survivors as they transitioned from on-site to virtual CR during COVID-19. Some were resilient to the change, while others would have benefited from additional individualised support. Suggestions for future directions may be transferrable to other virtual programs to help create individualised strategies and exercise prescriptions to improve outcomes during an unanticipated critical disruption.
Data availability
The authors have full control of all primary data and agree to allow the journal to review data if requested.
Code availability
Not applicable.
References
Gilchrist SC, Barac A, Ades PA, Alfano CM, Franklin BA, Jones LW et al (2019) Cardio-oncology rehabilitation to manage cardiovascular outcomes in cancer patients and survivors: a scientific statement from the American Heart Association. Circulation 139. https://doi.org/10.1161/CIR.0000000000000679
Kirkham AA, Davis MK (2015) Exercise prevention of cardiovascular disease in breast cancer survivors. J Oncol 2015:1–13. https://doi.org/10.1155/2015/917606
Mattioli AV, Ballerini PM (2020) Lifestyle at time of COVID-19: how could quarantine affect cardiovascular risk. Am J Lifestyle Med 14:240–242. https://doi.org/10.1177/1559827620918808
Thomas E, Gallagher R, Grace SL (2020) Future-proofing cardiac rehabilitation: transitioning services to telehealth during COVID-19. Eur J Prev Cardiol 2047487320922926. https://doi.org/10.1177/2047487320922926
Marzolini S, Ghisi GL d M, Hébert A-A, Ahden S, Oh P (2021) Cardiac rehabilitation in Canada during COVID-19. CJC Open 3:152–158. https://doi.org/10.1016/j.cjco.2020.09.021
Cunningham C, O’ Sullivan R (2020) Why physical activity matters for older adults in a time of pandemic. Eur Rev Aging Phys Act 17:16. https://doi.org/10.1186/s11556-020-00249-3
Monteiro-Guerra F, Signorelli GR, Tadas S, Dorronzoro Zubiete E, Rivera Romero O, Fernandez-Luque L et al (2020) A personalized physical activity coaching app for breast cancer survivors: design process and early prototype testing. JMIR MHealth UHealth 8:e17552. https://doi.org/10.2196/17552
Sabiston CM, Fong AJ, O’Loughlin EK, Meterissian S (2019) A mixed-methods evaluation of a community physical activity program for breast cancer survivors. J Transl Med 17:206. https://doi.org/10.1186/s12967-019-1958-4
Brunet J, Taran S, Burke S, Sabiston CM (2013) A qualitative exploration of barriers and motivators to physical activity participation in women treated for breast cancer. Disabil Rehabil 35:2038–2045. https://doi.org/10.3109/09638288.2013.802378
Campkin LM, Boyd JM, DJT C (2017) Coronary artery disease patient perspectives on exercise participation. J Cardiopulm Rehabil Prev 37:305–314. https://doi.org/10.1097/HCR.0000000000000195
Porter CM (2016) Revisiting precede–proceed: a leading model for ecological and ethical health promotion. Health Educ J 75:753–764. https://doi.org/10.1177/0017896915619645
Kite J, Phongsavan P (2017) Insights for conducting real-time focus groups online using a web conferencing service. F1000Research 6:122. https://doi.org/10.12688/f1000research.10427.1
Segal R, Zwaal C, Green E, Tomasone JR, Loblaw A, Petrella T et al (2017) Exercise for people with cancer: a clinical practice guideline. Curr Oncol 24:40–46. https://doi.org/10.3747/co.24.3376
Fetters MD, Curry LA, Creswell JW (2013) Achieving integration in mixed methods designs-principles and practices. Health Serv Res 48:2134–2156. https://doi.org/10.1111/1475-6773.12117
Hamm LF, Sanderson BK, Ades PA, Berra K, Kaminsky LA, Roitman JL et al (2011) Core competencies for cardiac rehabilitation/secondary prevention professionals: 2010 update. J Cardiopulm Rehabil Prev 31:2–10. https://doi.org/10.1097/HCR.0b013e318203999d
Dolan LB, Barry D, Petrella T, Davey L, Minnes A, Yantzi A et al (2018) The cardiac rehabilitation model improves fitness, quality of life, and depression in breast cancer survivors. J Cardiopulm Rehabil Prev 38:246–252. https://doi.org/10.1097/HCR.0000000000000256
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C et al (2011) 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 43:1575–1581. https://doi.org/10.1249/MSS.0b013e31821ece12
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3:77–101. https://doi.org/10.1191/1478088706qp063oa
Smith B, McGannon KR (2018) Developing rigor in qualitative research: problems and opportunities within sport and exercise psychology. Int Rev Sport Exerc Psychol 11:101–121. https://doi.org/10.1080/1750984X.2017.1317357
Rogers LQ, Markwell SJ, Courneya KS, McAuley E, Verhulst S (2009) Exercise preference patterns, resources, and environment among rural breast cancer survivors. J Rural Health 25:388–391. https://doi.org/10.1111/j.1748-0361.2009.00249.x
Glanz K, Rimer BK, Viswanath K (eds) (2008) Health behavior and health education: theory, research, and practice, 4th edn. Jossey-Bass, San Francisco, CA
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19:349–357. https://doi.org/10.1093/intqhc/mzm042
Colley R, Wong S, Hoffmann MD, Doyon CY, Lang JJ, Tomkinson GR (2019) Normative-referenced percentile values for physical fitness among Canadians. Health Rep 2019 30(10):3–11. https://doi.org/10.25318/82-003-X201901000002-ENG
Irwin ML, McTiernan A, Bernstein L, Gilliland FD, Baumgartner R, Baumgartner K et al (2004) Physical activity levels among breast cancer survivors. Med Sci Sports Exerc 36:1484–1491
López-Sánchez GF, López-Bueno R, Gil-Salmerón A, Zauder R, Skalska M, Jastrzębska J et al (2021) Comparison of physical activity levels in Spanish adults with chronic conditions before and during COVID-19 quarantine. Eur J Public Health 31:161–166. https://doi.org/10.1093/eurpub/ckaa159
Belgen Kaygısız B, Güçhan Topcu Z, Meriç A, Gözgen H, Çoban F (2020) Determination of exercise habits, physical activity level and anxiety level of postmenopausal women during COVID-19 pandemic. Health Care Women Int 41:1240–1254. https://doi.org/10.1080/07399332.2020.1842878
Sasaki S, Sato A, Tanabe Y, Matsuoka S, Adachi A, Kayano T et al (2021) Associations between socioeconomic status, social participation, and physical activity in older people during the COVID-19 pandemic: a cross-sectional study in a northern Japanese city. Int J Environ Res Public Health 18:1477. https://doi.org/10.3390/ijerph18041477
An K-Y, Kang D-W, Morielli AR, Friedenreich CM, Reid RD, McKenzie DC et al (2020) Patterns and predictors of exercise behavior during 24 months of follow-up after a supervised exercise program during breast cancer chemotherapy. Int J Behav Nutr Phys Act 17:23. https://doi.org/10.1186/s12966-020-00924-9
Petersen JA, Naish C, Ghoneim D, Cabaj JL, Doyle-Baker PK, McCormack GR (2021) Impact of the COVID-19 pandemic on physical activity and sedentary behaviour: a qualitative study in a Canadian city. Int J Environ Res Public Health 18:4441. https://doi.org/10.3390/ijerph18094441
Huang K, Liu W, He D, Huang B, Xiao D, Peng Y et al (2015) Telehealth interventions versus center-based cardiac rehabilitation of coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol 22:959–971. https://doi.org/10.1177/2047487314561168
Lear SA, Singer J, Banner-Lukaris D, Horvat D, Park JE, Bates J et al (2014) Randomized trial of a virtual cardiac rehabilitation program delivered at a distance via the Internet. Circ Cardiovasc Qual Outcomes 7:952–959. https://doi.org/10.1161/CIRCOUTCOMES.114.001230
Andrykowski MA, Beacham AO, Jacobsen PB (2007) Prospective, longitudinal study of leisure-time exercise in women with early-stage breast cancer. Cancer Epidemiol Biomarkers Prev 16:430–438. https://doi.org/10.1158/1055-9965.EPI-06-0735
Robinson E, Boyland E, Chisholm A, Harrold J, Maloney NG, Marty L et al (2021) Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite 156:104853. https://doi.org/10.1016/j.appet.2020.104853
Engberg E, Alen M, Kukkonen-Harjula K, Peltonen JE, Tikkanen HO, Pekkarinen H (2012) Life events and change in leisure time physical activity: a systematic review. Sports Med 42:433–447. https://doi.org/10.2165/11597610-000000000-00000
Kristensen IV, Rasmussen B, Livingston PM, Meldgaard A, Zerlang I, Jensen-Johansen MB et al (2019) The transitional experience of women with newly diagnosed breast cancer. J Nurs Educ Pract 9:23. https://doi.org/10.5430/jnep.v9n6p23
Littman AJ, Tang M-T, Rossing MA (2010) Longitudinal study of recreational physical activity in breast cancer survivors. J Cancer Surviv 4:119–127. https://doi.org/10.1007/s11764-009-0113-2
Stults-Kolehmainen MA, Sinha R (2014) The effects of stress on physical activity and exercise. Sports Med 44:81–121. https://doi.org/10.1007/s40279-013-0090-5
Ormel HL, van der Schoot GGF, Sluiter WJ, Jalving M, Gietema JA, Walenkamp AME (2018) Predictors of adherence to exercise interventions during and after cancer treatment: a systematic review. Psychooncology 27:713–724. https://doi.org/10.1002/pon.4612
Durosini I, Triberti S, Sebri V, Giudice AV, Guiddi P, Pravettoni G (2021) Psychological benefits of a sport-based program for female cancer survivors: the role of social connections. Front Psychol 12:751077. https://doi.org/10.3389/fpsyg.2021.751077
Scarapicchia TMF, Amireault S, Faulkner G, Sabiston CM (2017) Social support and physical activity participation among healthy adults: a systematic review of prospective studies. Int Rev Sport Exerc Psychol 10:50–83. https://doi.org/10.1080/1750984X.2016.1183222
Sabiston CM, McDonough MH, Crocker PRE (2007) Psychosocial experiences of breast cancer survivors involved in a dragon boat program: exploring links to positive psychological growth. J Sport Exerc Psychol 29:419–438. https://doi.org/10.1123/jsep.29.4.419
Banner D, Lear S, Kandola D, Singer J, Horvat D, Bates J et al (2015) The experiences of patients undertaking a “virtual” cardiac rehabilitation program. Stud Health Technol Inform 209:9–14
Yildirim OA, Poyraz K, Erdur E (2021) Depression and anxiety in cancer patients before and during the SARS-CoV-2 pandemic: association with treatment delays. Qual Life Res. https://doi.org/10.1007/s11136-021-02795-4
Goethals L, Barth N, Guyot J, Hupin D, Celarier T, Bongue B (2020) Impact of home quarantine on physical activity among older adults living at home during the COVID-19 pandemic: qualitative interview study. JMIR Aging 3:e19007. https://doi.org/10.2196/19007
Faro JM, Mattocks KM, Nagawa CS, Lemon SC, Wang B, Cutrona SL et al (2021) Physical activity, mental health, and technology preferences to support cancer survivors during the COVID-19 pandemic: cross-sectional study. JMIR Cancer 7:e25317. https://doi.org/10.2196/25317
Author information
Authors and Affiliations
Contributions
All authors designed the study. JL collected and analysed the quantitative data. JL and LV planned and carried out the focus groups. JL, LV, ST, TC, and PO contributed to the interpretation of the results. JL took the lead in writing the manuscript. All authors provided critical feedback and helped shape the research, analysis, and manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained from University Health Network/TRI’s Research Ethics Board CAPCR/UHN REBs: 20-5612.0 and 20-5759, respectively. All procedures performed involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Larkin, J., Vanzella, L., Thomas, S. et al. Breast cancer survivors’ physical activity and experiences while transitioning to a virtual cardiovascular rehabilitation program during a pandemic (COVID-19). Support Care Cancer 30, 7575–7586 (2022). https://doi.org/10.1007/s00520-022-07142-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07142-y